Original Article - (2019) Volume 20, Issue 1
1Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA
2Indiana University School of Medicine, Indianapolis, IN, US
Received November 15th, 2018 - Accepted January 10th, 2019
Introduction Damage control laparotomy is a widely accepted practice in trauma surgery. We applied this approach selectively to severely ill patients requiring open pancreatic débridement. We sought to evaluate outcomes associated with this novel, staged approach to operative pancreatic débridement. Methods Retrospective review evaluating 75 consecutive patients (12 DCD, 63 single-stage debridement) undergoing open pancreatic débridement by a single surgeon (2006-2016). Damage control débridement was compared to single staged débridement only as a point of reference and not to evaluate the technique as potentially superior. Results Patients treated by damage control débridement were more severely ill globally with increased preoperative organ failure (83% DCD vs. 43% SSD), intensive care unit admission (83% vs. 48%), and mean APACHE II (12.0 vs. 7.3). Indications for damage control débridement included: hemodynamic compromise (n=4), medical coagulopathy (n=4), or a combination (n=4). Six of 12 damage control débridement patients required three or more débridements prior to definitive abdominal closure (mean number of total débridements=2.6; range 2-4). Length of stay (43.8 vs. 17.1 days) and intensive care unit stay (20.8 vs. 5.9 days) was longer in damage control débridement patients. However, readmission (42% vs. 41%) and repeat intervention (58% vs. 33%; endoscopic: 17% vs. 11%; percutaneous drain: 42% vs. 19%; repeat operation after abdominal closure: 0% vs. 13%) were similar. Overall mortality was 2.7%; mortality was similar between damage control débridement (8%) and single staged débridement (2%). Conclusions Despite more severe acute illness, necrotizing pancreatitis patients treated with damage control débridement had similar morbidity and mortality as those undergoing elective single stage pancreatic débridement. Damage control débridement is an effective technique with which to salvage severely ill necrotizing pancreatitis patients.
Critical Illness; Debridement; Pancreatitis, Acute Necrotizing; Pancreatitis ; surgery; Treatment Outcome
AP acute pancreatitis; ANC acute necrotic collection; APACHE II acute physiology and chronic health evaluation II; DCD damage control débridement; DCL damage control laparotomy; ERCP endoscopic retrograde cholangiopancreatography; ICU intensive care unit; INR international normalized ratio; NP necrotizing pancreatitis; SAP severe acute pancreatitis; SSD single staged débridement, WON walled off necrosis
Acute pancreatitis (AP) is a local and systemic inflammatory disease process responsible for greater than 275,000 United States hospital admissions per year [1, 2]. The spectrum of AP severity varies widely. Most AP patients develop a mild and self-limited course requiring a short hospital stay; however, others experience multiple organ failure, severe sepsis, and a protracted hospital course. Severe acute pancreatitis (SAP) is frequently complicated with infection, need for intervention, multiple organ support, severe physical deconditioning and frequent readmissions. Up to 15-25% of all SAP patients develop necrotizing pancreatitis, with mortality rates in this subgroup as high as 30% [3]. Necrotizing Pancreatitis (NP) is defined as a non-enhancing area of pancreatic parenchyma on contrast-enhanced CT imaging, best visualized after the first week of the disease [4]. Infection of pancreatic necrosis or failure to improve in the absence of infection are the two indications for intervention in NP [5].
In the last decade, the “step-up approach” has become the standard of care in patients with pancreatic necrosis requiring intervention. With failure of more conservative management, the treatment is then “stepped-up.” This approach begins with percutaneous drainage, advances to endoscopic or video-assisted débridement, with surgical débridement reserved for those patients failing less invasive measures [6]. Thus, in current practice, those NP patients undergoing operative débridement have not improved or resolved with less invasive means and are the sickest of NP patients. These patients undergo operative débridement with historically high perioperative mortality rates, ranging from 5-40% [7, 8, 9, 10]. Despite advances in technique and critical care, mortality with débridement remains high, likely related to the fact that open pancreatic débridement is reserved for the most challenging situation.
Damage control laparotomy (DCL) has become a widely accepted practice in trauma surgery [11]. In DCL, the surgeon rapidly corrects the underlying pathology in short fashion, and expeditiously transfers the patient from the operating room to the intensive care unit for appropriate resuscitation and correction of metabolic disturbances. After goals of resuscitation have been achieved, the patient is taken back to the operating room for definitive care under more favorable physiologic circumstances. In our high volume clinical pancreatic surgery practice, we have begun to apply the principle of DCL selectively to the most severely ill NP patients requiring operative débridement. Thus, damage control débridement (DCD) is a staged approach to operative pancreatic débridement. The decision to pursue this technique is based on the clinical judgment of an experienced pancreatic surgeon intra-operatively, taking into account the patient’s unique, individual circumstance. Similar to DCL, the major indications guiding the decision to proceed with DCD are hemodynamic instability, medical coagulopathy, acidosis, hypothermia, or a combination of these factors. After a 10- year experience, we sought to critically evaluate outcomes associated with this technique.
Patient Population
Our institutional necrotizing pancreatitis database is a prospectively collected database beginning with patient data from 2006. The database includes all necrotizing pancreatitis patients treated at our institution’s University Hospital, regardless of management strategy. Among the 539 patients treated between 2006 and 2016, 356 patients underwent open pancreatic débridement. 75 patients were identified who underwent open pancreatic débridement by a single, experienced pancreatic surgeon. Twelve of the 75 patients underwent DCD. The remainder underwent traditional single stage débridement (SSD).
Diagnosis of Necrotizing Pancreatitis
Acute pancreatitis is defined according to the revised Atlanta classification as published in 2012 [4]. Patients met criteria if they had two or more of the following three features: “typical” acute onset epigastric abdominal pain radiating to the back, serum amylase/lipase level of greater than three times the upper limit of normal, or characteristic findings of acute pancreatitis on abdominal cross-sectional imaging studies. Severe acute pancreatitis is defined as AP with persistent organ failure (>48 hours), or local complication of acute peripancreatic fluid collection or acute necrotic collection [4].
Organ failure was defined according to the Modified Marshall scoring system for organ dysfunction: PaO2:FiO2 ratio of <300 defined respiratory failure; serum creatinine >1.9 mg/dL or 2 times baseline creatinine defined renal failure; and systolic blood pressure of <90 mmHg after fluid resuscitation or need for vasoactive agents defined cardiovascular failure [4].
Necrotizing pancreatitis is defined as parenchymal necrosis and/or peripancreatic necrosis represented as lack of pancreatic parenchymal enhancement and/or findings of acute necrotic collection (ANC) or walled off necrosis (WON) on contrast-enhanced imaging [4].
Necrosis Intervention
Treatment strategy of all patients with NP focuses on supportive care and avoids intervention of pancreatic necrosis, if possible. Indications for intervention on pancreatic necrosis in this study mirror those now published by the International Association of Pancreatology and the American Pancreatic Association [5]. The decision to pursue operative débridement is always made in consultation with the multi-disciplinary team, which includes medical pancreatologists, pancreatic endoscopists, interventional radiologists, and pancreatic surgeons. Whenever possible, intervention is delayed at least 4 weeks to allow maturation of the acute necrotic collection into walled off necrosis; operation is only performed earlier in the event of emergency, such as ischemic bowel, perforated viscus, or hemorrhage. At the time of operation, all patients, regardless of operative strategy, receive perioperative antibiotics within sixty minutes of incision, which are re-dosed as appropriate. Patients with documented infected necrosis based on intraoperative cultures are given a 7 to 10-day course of antibiotics postoperatively (after source control).
Damage Control Débridement
Decision to pursue DCD was based on the following intraoperative findings: hemodynamic instability requiring increasing doses of vasoactive medications or persistent acidosis despite volume resuscitation, medical coagulopathy that was clinically obvious during the operation, persistent hypothermia despite active rewarming efforts, or a combination. The primary goal of a damage control operation was to achieve maximal débridement prior to reaching an indicated endpoint, as above.
While débridement must be tailored to the individual patient with NP (based on anatomic distribution, parenchymal involvement, and individual clinical scenario), our general principals are as follows. Necrosis tracking down the paracolic gutters is approached from lateral to medial to allow safe access into the retroperitoneum. Lesser sac necrosis is approached after dividing the gastrocolic ligament. Débridement is performed manually (surgeon’s fingers) or with a ring forceps, taking only the necrosis that is freely mobile. Each field is debrided individually and packed with lap sponges while proceeding to the next field. Oozing from the inflamed surfaces is common and is often controlled with packing alone. Finally, vigorous irrigation helps to dislodge the necrosis.
At termination of damage control débridement, an open abdomen negative pressure therapy system was applied, and the patient was transported to the ICU setting for ongoing resuscitation and care. Once stabilized, one to three days later, the patient returned to the operating room for the next staged débridement. Following successful débridement of all necrotic tissue, wide closed-suction drains were placed, and the patient’s fascia was closed primarily or with vicryl mesh.
Data and Statistical Analysis
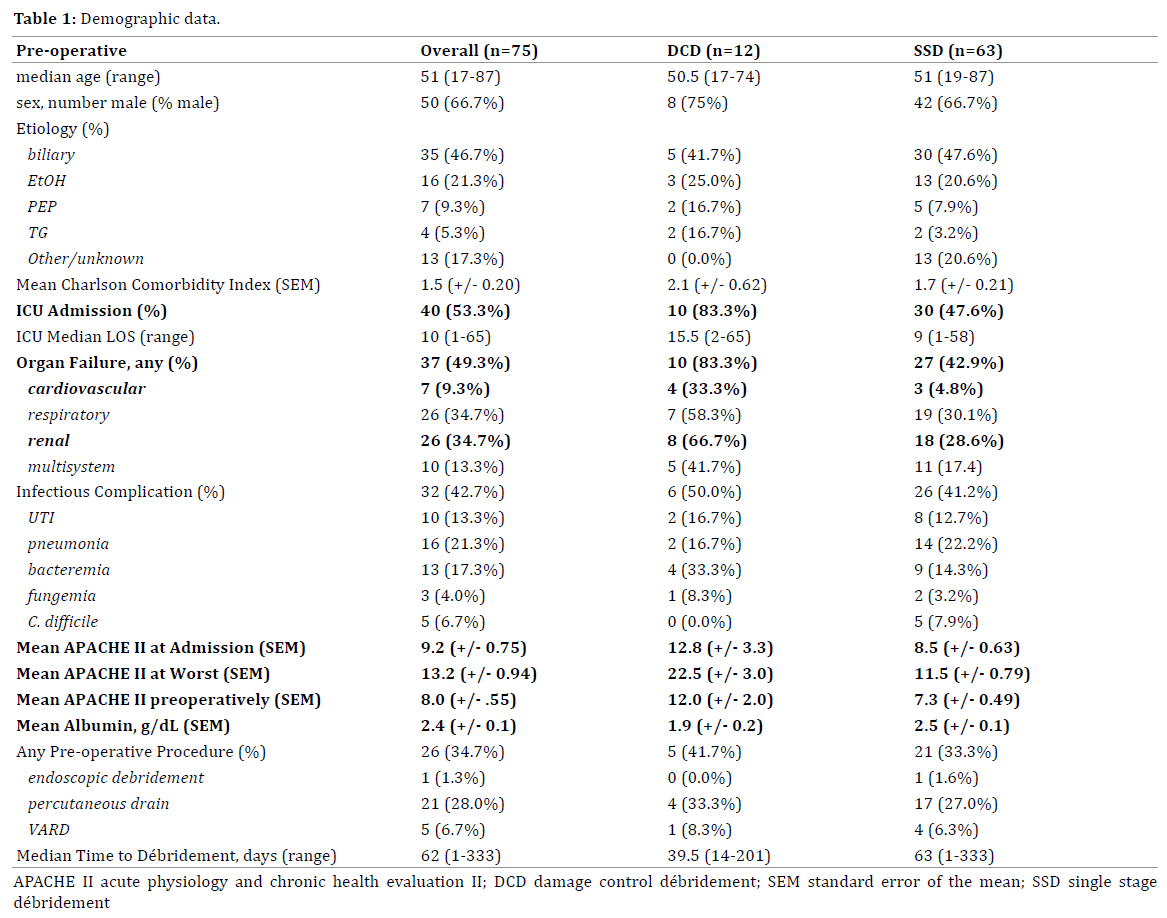
Individual demographic and clinical data were recorded, including: age, sex, Charlson co-morbidity index, and etiology (Table 1). Data regarding the patient’s clinical course were evaluated pre-, peri-, and post-operatively. Pre-operative data points included: APACHE II score at admission, worst, and immediately pre-operatively; cardiovascular, respiratory, and renal organ system failure; infectious complications including urinary tract infection, bacteremia, fungemia, pneumonia, and C. difficile colitis; need for ICU admission and duration; pre-operative INR, albumin, and total bilirubin; preoperative means of management and number of days from diagnosis until operation. Peri- and post-operative data points included: pH, base excess, and temperature at worst and at the conclusion of the operation, organ failure, infectious complications, need for ICU admission and duration, pancreatic fistula, need for re-intervention, discharge disposition, readmission, duration of follow-up, and mortality.
The aim of this review is to evaluate a novel technique used in the most severely ill NP patients. As such, outcomes are not compared statistically as this is purely a descriptive discussion. A cohort of only 12 patients does not allow sufficient power in the study group to objectively compare outcomes. Instead, SSD is used as a baseline to establish the inherent high morbidity associated with the disease, particularly those patients that require operative débridement. This point of reference highlights the extreme severity of illness in those patients requiring a staged approach to débridement.
Ethics
Data were compiled and reported in strict compliance with patient confidentiality protocols set forth by the Health Care Accountability and Portability Act (HIPAA) and our Institutional Review Board (IRB), which approved the conduct of this study. This work has been reported in line with the STROCSS criteria [12]. Written or oral consent were obtained from each patient and the study protocol conforms to the ethical guidelines of the World Medical Association Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects [13].
Population Characteristics
In 75 patients undergoing open pancreatic débridement, median age was 51 years (range 17-87). Fifty- (67%) patients were male and 25 (33%) patients were female. Etiology of AP was: biliary (47%), alcohol (21%), post-ERCP (5%), hypertriglyceridemia (5%), and other/idiopathic (17%). Average Charlson Comorbidity Index was 1.5 (+/- 0.2). Preoperatively, surgical ICU admission was required in 40 (53%) patients, and 37 (49%) had developed organ failure (26 respiratory failure, 26 renal failure, 7 cardiovascular failure, and 10 with multi-system organ failure). Mean APACHE II score was measured at admission (9.2 +/- 0.8), worst (13.2 +/- 0.9), and pre-operatively (8.0 +/- 0.6). Overall, 26 (35%) underwent a pre-operative procedure (21 percutaneous drainage, 5 endoscopic débridement, 1 videoassisted retroperitoneal débridement). Infected necrosis was documented by intraoperative cultures in 56 (75%) patients. Median time to débridement was 62 days (range 1-333). Indications for DCD were hemodynamic compromise (4, 33%), medical coagulopathy (4, 33%), or both (4, 33%). Median follow up was 27.6 months (range 1-134) (Table 1).
Comparison of Groups (DCD vs. SSD)
Groups were similar in mean age (DCD 50.5 vs. SSD 51), sex (75% vs. 67% male), and etiology (biliary 42% vs. 48%, alcohol 25% vs. 21%, post-ERCP 17% vs. 8%, hypertriglyceridemia 17% vs. 3%, or other 0% vs. 21%). Patients treated by DCD were more severely ill globally as evidenced by increased need for ICU admission (83% vs. 48%), incidence of organ failure (83% vs. 43%), preoperative APACHE II score (12.0 vs. 7.3), and malnutrition (albumin 1.9 vs. 2.5 g/dL) (Figure 1).
Intra-operatively, base excess at worst was lower in DCD patients (DCD -3 +/- 2.4 vs. SSD 0.5 +/- 1.9). The median number of planned débridements was 2.5 (range 2-4). Primary fascial closure was performed in eight patients (75%), while the remaining four (25%) required fascia approximation with vicryl mesh.
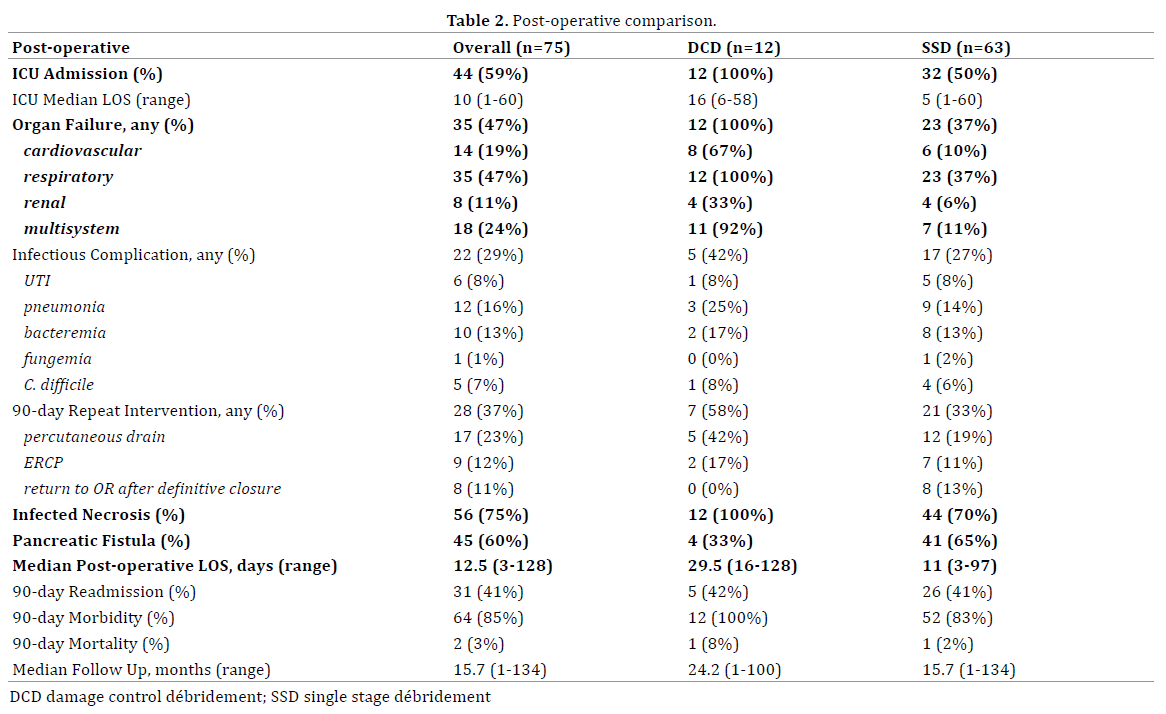
Post-operatively, DCD patients had a higher incidence of need for ICU admission (100% vs. 50%) and organ failure (100% vs. 37%). Organ failure was more prevalent in all aspects: respiratory (100% vs. 37%), renal (33% vs. 6%), cardiovascular (67% vs. 10%) and multisystem (92% vs. 11%).
The incidence of post-operative infectious complications was similar: any (42% vs. 27%), pneumonia (25% vs. 14%), bacteremia (17% vs. 13%), urinary tract infection (8% vs. 8%), C. difficile (8% vs. 6%), or fungemia (0% vs. 2%). Additionally, the need for post-operative repeat intervention were similar: any (58% vs. 33%), percutaneous drain (42% vs. 19 %), ERCP (17% vs. 11%), or return to OR after definitive closure (0% vs. 13%). Median post-operative length of stay was longer in the DCD group (30 vs. 11 days). However, DCD and SSD had similar 90- day readmission (42% vs. 41%), 90-day morbidity (100% vs. 83%), and 90-day mortality (8% vs. 2%) (Table 2).
Necrotizing pancreatitis patients requiring operative débridement have a protracted hospital course with a high degree of acute illness complicated by organ failure, infection, and malnutrition. As our treatment practices have changed over the last several years, NP patients treated at our quaternary care center often undergo pancreatic débridement as the definitive step in the modern algorithmic approach. However, despite unfavorable operative circumstances, we have reported acceptable morbidity and mortality in patients undergoing operative pancreatic débridement [14]. As critical care and minimally invasive techniques improve survival following the initial NP insult, more chronically and critically ill NP patients are undergoing operative débridement. Thus, there has become a need for new methods of open pancreatic débridement to salvage these critically ill patients with acceptable morbidity and mortality (Figure 2).
In 2010, the Dutch Pancreatitis Study Group published a landmark paper describing the “step-up” approach in managing NP requiring intervention. This randomized controlled trial compared the traditional gold standard of open pancreatic débridement to the “step-up” approach: percutaneous drainage, followed, if necessary, by minimally invasive retroperitoneal necrosectomy. The “step-up” approach was associated with decreased major complications or death and long-term complications and obviates the need for operative intervention in 30% of patients. This approach has been validated and is now advocated as the standard of care [15]. Our center has seen a similar evolution in our practice over the past 10 years [16]. In the current study, only 35% of patients underwent a minimally invasive procedure as the initial step in management. The time-period of the study spans a decade of significant evolution in the management of NP. Between 2006 and 2010, operative management was applied more frequently. This evolved into the step-up approach in the patients treated between 2011-2016. During this latter time period, more patients were treated initially with percutaneous or endoscopic therapy [17]. As such, in the modern treatment algorithm, operative débridement is now reserved for patients refractory to percutaneous and/or endoscopic therapy. Some of these patients do not have the physiologic reserve to undergo satisfactory débridement in a single operation and may represent a role for a staged-approach in the modern treatment algorithm for the most severely ill NP patient.
Damage control laparotomy dates to the early 1900s, with management of liver injuries by gauze packing and open drainage [18]. Although abandoned following the early 1900s, it was resurrected by the Detroit Receiving group in 1976 [19] and gained further interest following description of survival in 9 out of 10 patients undergoing perihepatic packing following major hepatic injuries [20]. Widespread acceptance began by the mid 1980s as Feliciano and colleagues described “rapid conservative operative technique” in a large volume study with improved outcomes [21]. Over the next 20 years, technique was honed and studies continued to validate the practice in a select population of patients with traumatic injuries requiring laparotomy [11]. Thus DCL is accepted as a “rational approach to an apparently hopeless situation [22].” Damage control techniques have been applied to pancreatic surgery, but have not been reported to date for pancreatic débridement [23].
Resolution of NP often takes greater than 6 months, multiple procedures, several readmissions, and is associated with high morbidity. NP has profound systemic effects including organ failure, infection, severe malnutrition, and physical deconditioning. The mean worst APACHE II score in our study was 16.8, which carries a predicted mortality of 25% [24]. Pre-operatively, 49% of patients developed organ failure, with 21% having multiple organ failure. Infection was widely prevalent: 43% were treated pre-operatively for an infectious complication. The inflammatory response severely effects nutrition as evidenced by a mean pre-operative albumin of 2.4 mg/dL. 27% of patients surviving to discharge required placement into a facility for ongoing rehabilitation and care, and those going home almost ubiquitously required outpatient nursing and rehabilitation services. The physiologic consequence of this systemic disease is devastating and far from the ideal operative scenario.
Given the “stacked-deck” against the surgeon, application of damage control laparotomy to open pancreatic débridement seems logical. Historically, multidébridement approaches to NP have been described. In 1987, Bradley described a technique of operative debridement followed by open abdominal packing and healing by secondary intent [25]. While this laparostomy technique improved mortality, compared to contemporary standards, morbidity was significant with high rates of intestinal fistula and 100% hernia rate. Sarr et al described an approach with planned re-laparotomy in 1991 [26]. This “zipper” technique also improved morality; however, the majority of patients underwent greater than five operations, closure of the abdominal wound was infrequently performed, and fistula rates were remarkably high.
Damage control débridement, as described in the current report, represents a combination of historical approaches to pancreatic débridement, with the addition of modern trauma principles based on physiology. DCD is a staged approach aimed to accomplish complete débridement, achieve wound closure, and limit the physiologic insult by terminating operations based on physiologic derangement. Decision to pursue DCD was based on the intraoperative findings; however, some preoperative indices may suggest which patients benefit from DCD, such as pre-operative APACHE II score, albumin, and organ failure. Ultimately, decision to pursue DCD is based on pre-operative indices combined with intraoperative findings, but importantly the ability of an experienced pancreatic surgeon to critically judge the global picture of the individual patient.
This review of our experience with damage control débridement was not intended to compare a novel technique to a single stage débridement, but instead use the single stage group as a point of reference. No matter the technique, patients requiring operative débridement traditionally have high morbidity and mortality. Our experience with operative débridement and the postoperative care of NP patients is extensive; as a result, the overall cohort has a remarkably low mortality of 4%. Patients undergoing an operative débridement are incredibly acutely ill, and the subset of patients requiring a damage control débridement are the most severely ill of this patient population. A damage control approach to these patients offers definitive operative therapy with similar morbidity and mortality to those undergoing traditional operative débridement despite significantly increased severity of illness.
Limitations to this study are clear. While data is obtained prospectively, the study was evaluated retrospectively. Similar to trauma DCL, application of DCD is at the discretion of the surgeon and not randomized based on quantitative data; refinement of discrete indices for DCD are needed. This study is underpowered to perform a comparative univariate or multivariate analysis with a sample size of 12 patients. However, the intent was not to report the superiority of DCD, but instead to display its feasibility compared to our reference patients undergoing single staged débridement.
Moving forward, development of a necrotizing pancreatitis severity index may help guide the decision to pursue a damage control approach. Indices could include: active sepsis, malnutrition, organ failure, APACHE II score, and close intraoperative monitoring for acidosis, need for vasoactive agents, coagulopathy, and hypothermia.
A select percentage of NP patients are so severely ill that a definitive open débridement cannot be tolerated in a single operation. In these patients a staged approach is required. Damage control débridement proved to be a very effective approach in the “sickest of the sick.” Use of this staged approach to débridement may improve outcomes for select, critically ill necrotizing pancreatitis patients who require open débridement.
The authors have no conflicts of interests to declare.