Research Article - (2017) Volume 25, Issue 4
Abebaw Miskir
Arba Minch University, Arba Minch, Southern Ethiopia
Wanzahun Godana
Arba Minch University, Arba Minch, Southern Ethiopia
Meseret Girma
Arba Minch University, Arba Minch, Southern Ethiopia
Feleke G/Miskel*
Arba Minch University, Arba Minch, Southern Ethiopia
Corresponding Author:
Feleke Gebremeskel W/Hawariat
Arba Minch University
Arba Minch, Southern Ethiopia. P.Box 021, Ethiopia
Tel: 251912455496
E-mail: fgfpeace@gmail.com
Submitted date: August 01, 2017; Accepted date: August 08, 2017; Published date: August 15, 2017
Background: Acute malnutrition is usually the result of a combination of inadequate dietary intake and infection. It is a third most risk factor for death of under-five children in the world. Acute malnutrition among children under-five years of age is a long last problem in most areas of Ethiopia including the study area, Konso. The aim of this study was to identify determinants of acute malnutrition among under-five children in Karat district hospital and Karat health center, Southern Ethiopia 2015-2016.
Methods: Institutional based case control study was conducted at Karat district general Hospital and Karat Health Center among under-five children who were acute malnourished and well- nourished babies visit in the public health facilities during the study period. Data were collected from February 28 to April 13, 2016 using structured interview for mothers, and anthropometric measurement of children. A sample of 343 with 114 cases and 229 controls with case to control ratio of 1:2, respectively, were taken at the public health facilities.
Findings: Acute malnutrition was associated with: mothers education, maternal marital status (single, widowed or divorced), family size of five and above, joint decision on household consumption, water source for drinking from river, duration of child breast feeding below 12 months, dietary diversity of less than or equal to three food groups and children who had diarrhea illness for the last two weeks prior to data collection.
Conclusion: To reduce childhood acute malnutrition, due emphasis should be given in empowering women and improving the knowledge and practice of parents on appropriate infant and young child caring practices.
Keywords
Acute malnutrition; Arba Minch; Southern Ethiopia
Abbreviations
AMHC: Arba Minch Health center; AMN: Acute Malnutrition; ANC: Antenatal Care; AOR: Adjusted Odds Ratio; CBN: Community Based Nutrition; CI: Confidence Interval; Cm: Centimeters; EDHS: Ethiopian Demographic and Health Survey; EMDHS: Ethiopian Mini Demographic and Health Survey; EOS: Enhanced Outreach Strategy; HEP: Health Extension Program; Km: Kilometer; MAM: Moderately Acute Malnutrition; MDG: Millennium Development Goals; MUAC: Mid Upper Arm Circumference; NGO: Non Governmental Organization; PNC: Postnatal Care; SAM: Severe Acute Malnutrition; SAPZ: Segen Area Peoples Zone; SD: Standard Devation; SNNPR: Southern Nation; Nationalities and People Region; SPSS: Statistical Package for Social Science; TSF: Targeted Supplementary Food; UNICEF: United Nations Children’s Fund; WFH: Weight for Height; WHO: World Health Organization
Background
Child malnutrition is one of the measures of health status as world health organization (WHO) recommends for the equity in health. As commonly known the term malnutrition refers to both under nutrition and over nutrition [1].
Acute malnutrition is usually the result of a combination of inadequate dietary intake and infection. In children, acute malnutrition is synonymous with growth failure in which the malnourished child is shorter and lighter than they should be for their age. Protein energy malnutrition has been identified as a major health and nutritional problem. It is not only an important cause of mortality and morbidity but also leads to physical and mental impairment in children [2]. When the nutritional status of a child deteriorates in a relatively short period of time (his or her weight drops to such a low level that they are at risk of dying), the child can be said to have acute malnutrition [3,4].
Acute malnutrition of a child can be, severe acute malnutrition (SAM), carries the highest risk of death - nine times higher than for a healthy child, or moderate acute malnutrition (MAM), faces a three times greater risk of dying than a well-nourished child. There are two immediate causes of acute malnutrition. The first is when a child does not have enough to eat and the second is when a child develops an illness or infection. In most cases, these factors combined to cause a rapid and significant loss of weight and - if things deteriorate and the child is not treated – death [3].
According to WHO in 2009 child growth standards and identification of severe acute malnutrition in infants and children, a child’s weight for height measurement is less than 70% of the normal range for his age and the child’s MUAC is less than 11.5 cm, would be diagnosed as having severe acute malnutrition [4-6].
Various studies show that children and women are the primary victims of malnutrition, who suffer the most lasting consequences [7]. Acute malnutrition among children at the globe level is still a critical problem; its effects are long lasting and go beyond childhood; it has both short and long term consequences. For instance, undernourished children are physically, emotionally and intellectually less productive and suffer more from chronic illnesses and disabilities than well-nourished children [8].
In Ethiopia a considerable effort to monitor child acute malnutrition rates over the last two decades done and shows some improvement. Even though Ethiopia has already achieved a remarkable progress in reducing under-five mortality in the last decades, recent studies shows that Ethiopia is among countries with the highest acute malnutrition rates in the world and approximately half of the children under-five are still malnourished [9].
Although, the problem of acute malnutrition in Ethiopia is relatively well documented, its specific determinants are not well understood. To reduce acute malnutrition, one must understand its causes; nonetheless, there has been a paucity of micro-level data and information regarding the key determinants of both acute and chronic malnutrition in different geographic regions [10].
Malnutrition is a serious problem in the world; currently, 195 million under-five children are affected by malnutrition globally; 55 million of them suffer from acute malnutrition and around 26 million under-five children are severely acute malnourished. Among the total under-five children suffering from malnutrition, 90% lives in sub-Saharan Africa and South Asia. Every year, 3.5 million children die of malnutrition-related causes in the world [2,8]. Hence, it is at third level in the world of the disease burden in this age group [4].
Even though childhood acute malnutrition declined relatively during the year 1990’s globally; its burden in Africa was increased. Thus, in the developing countries more than 25% (143 million) under-five children are malnourished. Among these, nearly three quarters live in just 10 countries in Sub-Saharan Africa region and more than one-quarter of children under-five are malnourished in Nigeria and Ethiopia alone which accounts more than 33% [8].
According to EDHS 2011 report, one in every 17 Ethiopian children dies before the first birthday, and one in every 11 children dies before the fifth birthday [2,4].
Ethiopia is among the nations with very high burden of under nutrition in the world and at least 53-57% of under-five children mortality rate can be attributed directly or indirectly to malnutrition. According to the latest Ethiopian Mini Demographic and Health Survey 2014 (EMDHS) report; there has been a substantial decline in the proportion of children stunted and underweight in the last 15 years and a smaller decline in the prevalence of wasting. Forty percent of children under age five were stunted, 9% were wasted and 25% underweight in 2014. Even though the government health sector developments plan IV (2010/11-2014/15): Enhanced Outreach Strategy (EOS) with Targeted Supplementary Food (TSF) and Transitioning of EOS into the Health Extension Programmed (HEP), Health Facility Nutrition Services, Community Based Nutrition (CBN), and Micronutrient Interventions and Essential Nutrition Actions/Integrated Infant and Young Feeding Counseling Services, continues to improve the nutritional status of mothers and Children through different programs; under nutrition among children is still a common problem in Ethiopia [10,11].
According to EDHS 2011, in Ethiopia 29% of children under age five were underweight, 9% severely underweight and it was highest in SNNPR which was 28.3%. Additionally, its analysis revealed, in Southern Nations Nationalities and People region of Ethiopia the percentage of children who were severely stunted, severely wasted and severely underweight was 22.9%, 1.9% and 9.6%, respectively [11,12].
However, acute malnutrition problem is still a major concern in Ethiopia in general and the study area in particular; no study was conducted before about acute malnutrition status and related factors amongst under-five children; and various associated factors were not clearly known in the study area. Therefore, this study is aimed to determine factors associated with the nutritional status of the children (6-59 months) of under-five age group.
Materials and Methods
Study area
This study was conducted in karat town, Konso Woreda, Southern Ethiopia. Konso Woreda is one of the five Woredas of Segen Area Peoples Zone (SAPZ) in SNNPR. It is located at 640 km south west of Addis Abeba, 365 Km from capital city of SNNPR, Hawassa and 90 km away from Arba Minch. The Woreda comprises two urban and 39 rural kebeles. The total population of the woreda is 258,832 with house hold no of 51, 334. The lively hood of the Konso community is mixed farming; crop cultivation complimented by small live stock holdings.
Study design and period
An institutional based case-control study was conducted in children aged six to fifty nine months in Karat public health facilities. The data collection period was carried out from February 28 to April 13, 2016.
Source and study population
This study was conducted in Karat district general hospital and Karat health center among children age between 6-59 months.
Sampled children aged 6-59 months, who visited Karat district general hospital and Karat health center during the study period were the study population, and all children aged 6-59 months, who were found in Konso district and others who utilize the health facilities, were the source population.
Cases (acute malnutrition)
Includes both MAM and SAM; which defined as children between 6-59 months of age whose WFH<80% and/or their MUAC<12.5 cm (MAM) and WFH<70% and/or MUAC<11.5 cm (SAM) with or without bi-lateral pitting edema were considered as acutely malnourished [6].
Controls
Children between 6-59 months of age whose WFH>80% and/or MUAC>12.5 cm and without pitting nutritional edema attending health facility in under-five OPD.
The data collection period was carried out from February 28 to April 13, 2016.
Inclusion criteria: Children from 6-59 months visited Karat district hospital and Karat health center during the study period. Child’s mother/caregiver present and able to give response.
Exclusion criteria: Children in critical health conditions. Mothers/caregivers who were seriously ill and unable to respond to the questions
Sample size determination and sampling procedures
The required sample size was calculated by taking into account the major associated factor using the statistical program of the Epi Info version 7 using two population proportion formulas. In this regard, a 5% level of significance (two-sided) or the hypothesis of no significant difference, a power of 80% and a two to one allocation ratio of not acute malnourished to acute malnourished (2:1) was assumed. Among associated factors for acute malnutrition taken from a literature, squeeze out of first breast milk (colostrum) (i.e., 43.3% - cases with exposure, and 27.4% - controls exposed, with odd ratio of 2.02) taken as a major associated factor to be studied [13]. Based on the above assumptions, with an additional 10% for non-response rate the total sample size was 343 with 114 cases and 229 controls.
Systematic random sampling technique was applied to select mothers of under-five children visiting to Karat public health facilities (Karat district hospital and the health center) for interview during the study period. The sampling procedure in general was as follows: first of all the last 4 weeks data of underfive children in both public health facilities was taken for the purpose of sample allocation and to determine their sharing’s. Based on this, the number of under-five children obtained from Karat public health facilities under-five log-book in 4 weeks was as follows:
The health center=312 (under-five OPD=272 and from vaccination=40)
The district hospital=176 (under-five OPD=138 and inpatient room=38).
Thus, in order to allocate the sample size to both public health facilities, the following calculation was used:
Total number of under-five children obtained in 4 weeks in both health facilities=312+176=488.
For the health center: (312/488) × 100%=63.9%
Samples sharing to the health center=(63.9/100) × 343=219.2~220=220
From this, Cases=73 and Controls=147
For the district hospital: (176/488) × 100%=36%
Sample sharing to the district hospital=(36/100) × 343=123
From this, Cases=41 and Controls=82
After the sample size was allocated for both public health facilities (Karat health center and district hospital, systematic random sampling technique was used to interview mothers. This is computed as follows:
For the health center: N=343, n=220, K=N/ n=343/220=1.559=2, K=2
Now select “j” between 1 and K=2. Which is either 1 or 2, randomly j=1
1st, 3rd, 5th…continued till the sample allocated to the health center is fulfilled between the intervals (i.e., between 1 and N=343).
In similar fashion for the district hospital: N=343, n=123, K=343/123=2.788=3, K=3.
Now select “j” between 1 and K=3, randomly selected 2, j=2.
2nd>, 5th, 8th…continued till the sample allocated to the district hospital is fulfilled.
Study variables
Acute malnutrition status, child’s sex, child’s age, residence, mother’s occupation, mother education, family size, ethnicity, religion, wealth index, decision on household consumption.
Environmental factors: Water source, availability and utilization of latrine.
Child feeding and caring practices: information on child feeding, duration of breast feeding, dietary diversity, exclusive breast feeding and complementary feeding.
Child morbidity: Malaria, diarrhea, pneumonia.
Health service care: PNC, de-worming, place of delivery, ANC, growth monitoring.
Operational definitions
Wasted (weight-for-height index): Wasting represents the failure to receive adequate nutrition in the period immediately preceding the survey and may be the result of inadequate food intake or a recent episode of illness causing loss of weight and the onset of malnutrition [11].
Describes current nutritional status; includes both MAM and SAM.
Moderate acute malnutrition: WFH<80% and MUAC<12.5 cm with or without edema..
Severe acute malnutrition: WFH< 70% and MUAC<11.5 cm with or without edema [6,11].
Data collection procedures
The source of data for the study was obtained from mothers’ interview and using anthropometric measurements of children aged 6-59 months. Data were collected by using structured questionnaire after pretest interview was conducted. The structured questionnaire was adapted from different literatures in English to enable the comparability of the finding and translated into Amharic language for field work purpose and back to English for checking language consistency. Weight and height of every child were measured using standard technique and calibrated equipment (Salter scale and measuring board instrument).
Sliding board was used to measure the length of children aged less than 2 years (85 cm) in recumbent position and lay on flat surface, head positioned firmly against the fixed hardboard, with the eyes looking vertically.
MUAC was measured on the left arm by using tape mater by taking at the level of the upper arm midpoint mark.
Data quality management
To keep the data quality, supervisor, Nurse (BSc.), three diploma Nurses and one public health officer data collectors were trained for a day on the objective of the study and methods of data collection, anthropometric measurement and data recording. The questionnaire was pre tested on 10% of the sample size at the study area prior to the data collection period. A supervisor and principal investigator were closely following the day to day data collection process and ensure completeness and consistency of the collected questionnaires on a daily basis.
Weight and height of every child were measured using standard technique and calibrated equipment (Salter scale and measuring board instrument). The Weighing scales were calibrated with known weight object (using 2 kg rod) regularly and the measurement was approximated to the nearest 10 g. Children dressed light clothes with no shoes.
Sliding board was used to measure the length of children in recumbent position by four data collectors (each two data collectors together) and taken to the nearest 1 mm. Length was measured by making child lay on flat surface, head positioned firmly against the fixed hardboard, with the eyes looking vertically. The knees extended by applying firm pressure and feet were flexed at right angles to the lower legs on the board. MUAC was measured on the left arm by using tape mater by taking at the level of the upper arm midpoint mark.
Data processing and analysis
Each questionnaire was checked for completeness and consistency by data collectors’ supervisors and lastly the principal investigator. Data were entered into Epi Info version 7 and exported to SPSS version 20 for analysis. Then, cleaned, edited, coded/recoded, categorized and stored to facilitate its analysis. The data analysis was carried out to check the assumptions: model adequacy checking, influential outliers-checked by standard residual (Z residual<2), multi-collinearity, normality-checked by plots histogram, skewness and kurtosis other checking and analysis descriptive statistical outputs.
Logistic regression was used to fit the data to identify factors associated with determinant factors of acute malnutrition. All explanatory variables associated with the outcome variable in bivariate analysis with p-value of 0.25 or less and variables which had public, medical and biological plausibility are including in the initial logistic models of multivariable analysis. P-value<0.05 was considered declaring a result as statistically significant.
Ethical clearance
A letter of ethical approval was taken from Ethical Clearance Committee of Arba Minch University. An official letter of co-operation also taken from the Zonal Health Department and Konso District Health Office. Prior to interview, data collectors were requested mothers for the interviewees' verbal consent and assent after informing them about the confidentiality of the information they provided and that their names or addresses were not recorded, with answered being anonymous. Participants in the study were voluntarily asked and their right was kept even they refuse from interview. Interviewers were told participant their involvement was important to them, to their children health, and health of their community.
Results
Child feeding practice
Majority of children among cases 100 (87.70%) feed breast milk below 12 months; whereas, among controls below half 110 (48.00%) of them feed breast milk less than 12 months. In case of exclusive breast feeding practice, 54 (47.4%) of children among cases and 37 (16.2%) among controls started to early initiation of complementary feeding before six months (Figure 1).
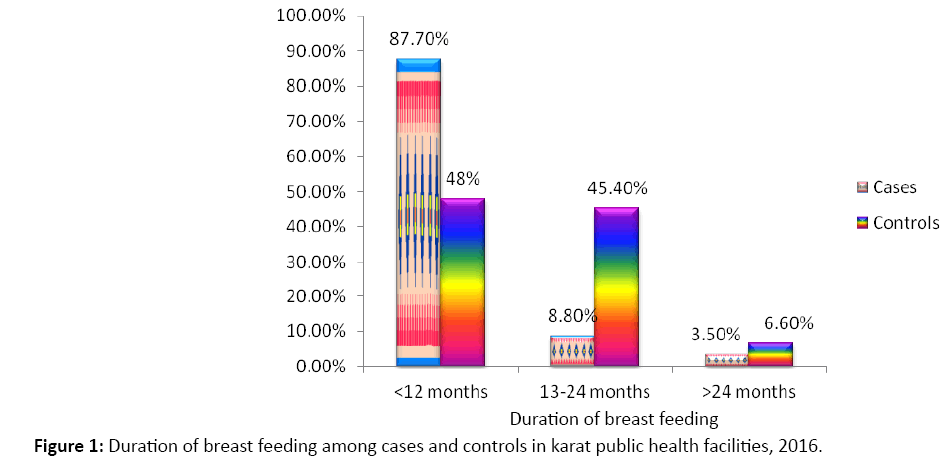
Figure 1: Duration of breast feeding among cases and controls in karat public health facilities, 2016.
In case of dietary diversity, relatively high proportion of children among cases 85 (74.6%) had low dietary diversity feeding practice (<=3 food groups) as compared to controls 80 (34.9%) who consumed low dietary diversity. Almost three fourth children from cases and one third among controls feed below four food groups of dietary diversity. From all food items grains were the commonest food item consumed in both cases and controls in the study area (Figure 2).
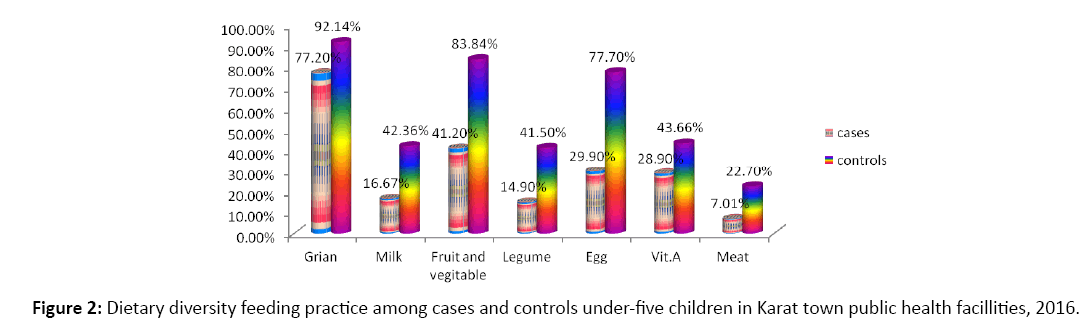
Figure 2: Dietary diversity feeding practice among cases and controls under-five children in Karat town public health facillities, 2016.
In case of child morbidity factors, diarrhea is highest among cases 85 (74.6%) compared to controls 57 (24.9%). Pneumonia is the second; whereas malaria is not as such usual under-five children disease in the study area (Figure 3).
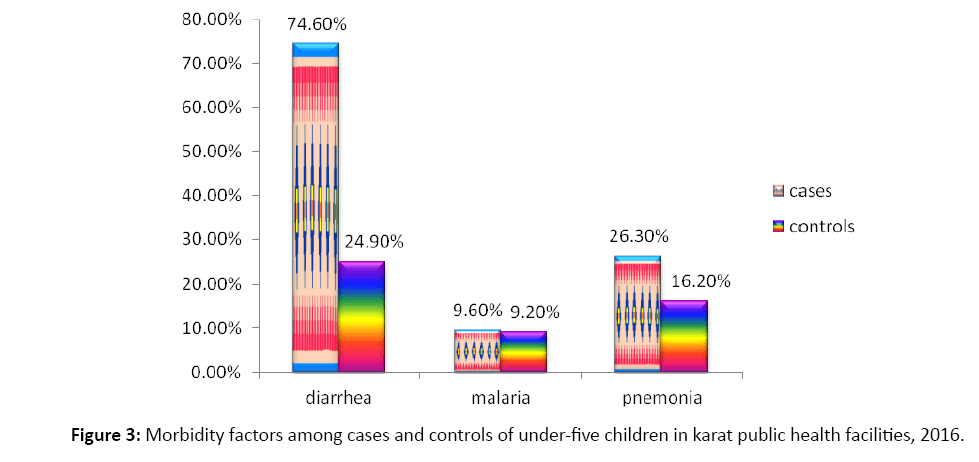
Figure 3: Morbidity factors among cases and controls of under-five children in karat public health facilities, 2016.
Socio-demographic characteristics of the mothers and under-five children
A total of 343 women having young child aged 6 months to 5 years were interviewed in the study. More than 5/6th of respondents (mothers) in both among cases 96 (84.2%) and controls 155 (67.7%) were rural dwellers. Half of children among cases 57 (50%) and around 3/5th among controls 131 (57.2%) were males. Among the study participants, majority of children among cases 99 (86.80) and controls 175 (76.40%) were aged less than 12 months. Around 3/5th of mothers among cases 70 (61.4%) and more than half in controls 126 (55.0%) were farmers. Protestant worshipers were highest number in both cases 66 (57.9%) and controls 140 (61.1%) in the study area and the local ethnic group, Konso were covered maximum proportion with equal coverage in both cases 102 (89.5%) and controls 204 (89.1%) (Table 1).
| Variables | Frequency Among Cases | Frequency Among controls |
|---|---|---|
| Residence Rural Urban |
96 (84.2%) 18 (5.8%) |
155 (67.7%) 74 (32.3%) |
| Sex of child Male Female |
57 (50.0% 57 (50.0%) |
131 (57.2%) 98 (42.8%)) |
| Age of child <12 months 12-24 months > 24 months |
99 (86.80) 12 (10.50%) 3 (2.60%) |
175 (76.40%) 37 (16.20%) 17 (7.40%) |
| Occupational status of mothers Farmer Private Government worker Housewife |
70 (61.4%) 18 (15.8%) 2 (1.8%) 24 (21.1%) |
126 (55.0%) 29 (12.7%) 25 (10.9%) 49 (21.4%) |
| Religion Orthodox Protestant Others |
36 (31.6%) 66 (57.9%) 12 (10.5%) |
77 (33.6%) 140 (61.1%) 12 (5.2%) |
| Ethnicity Konso Amhara Gamo Others |
102 (89.5%) 6 (5.3%) 2 (1.8%) 4 (3.5%) |
204 (89.1%) 8 (3.5%) 12 (5.2%) 5 (2.2%) |
Table 1: Socio-demographic characteristics of mothers and under-five children, in Karat public health facilities,
Health service utilization factors
Almost two third of mothers among cases 72 (63.20%) and almost three fourth among controls 66 (28.8%) were not have ANC follow up history. More than half of mothers among case 65 (57.0%) and less than 1/4th among controls 44 (19.2%) were delivered (give birth) at home. Four fifth of mothers among cases 91 (79.8%) and below half among controls 99 (43.2%) were mothers who had PNC follow up history. Highest number of children among cases 100 (87.7%) and around half of them among controls 110 (48.0%) were children who feed breast milk below 12 months. More than 4/6th of children among cases 79 (69.3%) and 1/4th of them among controls 58 (25.30%) did not have growth monitoring follow up. More than 5/6th children among cases 96 (84.2%) and around 3/5th among controls 132 (57.6%) were got de-worming service (Table 2).
| Variables | Frequency Among Cases | Frequency Among controls |
|---|---|---|
| ANC Yes No |
42 (36.80%) 72 (63.20%) |
163 (71.2%) 66 (28.8%) |
| Place of delivery Home Health facility |
65 (57.0%) 49 (43.0%) |
44 (19.2%) 185 (80.8%) |
| PNC follow up Yes No |
23 (20.2%) 91 (79.8%) |
130 (56.8%) 99 (43.2%) |
| Growth monitoring Yes No |
35 (30.7%) 79 (69.3%) |
171 (74.7%) 58 (25.30%) |
| De-worming Yes No |
18 (15.8%) 96 (84.2%) |
97 (42.4%) 132 (57.6%) |
Table 2: Maternal and child health service utilization factors, in Karat public health facilities, 2016.
Factors associated with acute malnutrition of under-five children
After conducting Multivariate logistic regression analysis, duration of child breast feeding those who were feed breast milk less than 12 months, AOR 3.02 (1.57,23.04), Dietary diversity of less than or equal to three food groups, AOR 5.13 (1.56,16.84), children who had diarrhea illness for the last two weeks prior to data collection, AOR 8.41 (4.03,27.26) education level of mothers those who had no formal education AOR, 4.70 (1.23, 10.20) and primary education AOR, 3.01 (1.18, 6.74), Marital status of mothers those who were other (single, widowed or divorced), AOR 3.33 (1.52, 14.66), family size of the household having five and above, AOR 2.28 (1.04, 8.22), decision on household consumption in both jointly, AOR 0.26 (0.07,0.96) which is preventable, Water source for drinking those who were utilize from river, AOR 5.61 (2.04,27.03) and from spring AOR 2.63 (1.01,12.22), were significantly associated with acute malnutrition in this study on the study area (Table 3).
| Variables | Cases Controls |
Crude OR (95% CI) | Adjusted OR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Duration of breast feeding ≤ 12 months 13-24 months >24 months |
100 (87.70%) 10 (8.80%) 4 (3.50%) |
110 (48.0%) 104 (45.4%) 15 (6.60%) |
3.41 (1.09,10.61) 0.36 (0.10, 1.30) 1 |
3.02 (1.57,23.04) 0.21 (0.039,1.09) 1 |
0.007* 0.063 |
| Exclusive breast feeding <6 month > 6 month |
54 (47.4%) 60 (52.6%) |
37 (16.2%) 192 (83.8%) |
4.67 (2.81, 7.76) 1 |
0.81 (0.261,2.49) 1 |
0.71 |
| Dietary diversity < 3 food group > 4 food group |
85 (74.6%) 29 (25.4%) |
80 (34.9%) 149 (65.1%) |
5.46 (3.31, 9.01) 1 |
5.13 (1.56,16.84) 1 |
0.007* |
| PNC follow up Yes No |
23 (20.2%) 91 (79.8%) |
130 (56.8%) 99 (43.2%) |
1 5.19 (3.06, 8.79) |
1 2.508 (0.82,7.65) |
0.11 |
| De-worming Yes No |
18 (15.8%) 96 (84.2%) |
97 (42.4%) 132 (57.6%) |
1 3.92 (2.22,6.91) |
1 1.40 (0.43,4.51) |
0.58 |
| Diarrhea within 2 weeks Yes No |
85 (74.6%) 29 (25.4%) |
57 (24.9%) 172 (75.1%) |
8.85 (5.27,14.3) 1 |
8.41 (4.03,27.26) 1 |
0.000* |
| Having information on child feeding Yes No |
100 (87.7%) 14 (12.3%) |
222 (96.9%) 7 (3.10%) |
1 4.44 (1.74, 1.34) |
1 0.35 (0.04,3.23) |
0.36 |
| Colostrums breast milk feeding Yes No |
12 (10.5%) 102 (89.5%) |
107 (46.7%) 122 (53.3%) |
1 7.45 (3.88,14.31) |
1 1.84 (0.59,5.78) |
0.30 |
| Residence Rural Urban |
96 (84.2%) 18 (5.8%) |
155 (67.7%) 74 (32.3%) |
2.54 (1.43,4.52) 1 |
0.79 (0.14,4.65) 1 |
0.80 |
| Sex Male Female |
57 (50.0% 57 (50.0%) |
131 (57.2%) 98 (42.8%) |
1 1.34 (0.852,2.10) |
2.56 (0.88,7.50) 1 |
0.09 |
| Education level of mother No formal Education Primary education Secondary & above |
87 (76.3%) 21 (18.4%) 6 (5.3%) |
118 (64.6%) 52 (14.0%) 49 (21.4%) |
6.02 (1.98,11.67) 3.30 (1.95,14.73) 1 |
4.70 (1.23,10.20) 3.01 (1.18,6.74) 1 |
0.01* 0.04* |
| Marital status Married Others |
103 (90.40%) 11 (9.60%) |
222 (96.90%) 7 (3.10%) |
1 3.39 (1.28, 8.99) |
1 3.33 (1.52,14.66) |
0.003* |
| Occupational status Farmer Private Government worker Housewife |
70 (61.40%) 18 (15.80%) 2 (1.80%) 24 (21.10%) |
126 (55.00%) 29 (12.70%) 25 (10.90%) 49 (21.40%) |
1.13 (0.64,2.00) 1.27 (0.59,2.72) 0.16 (0.03,0.75) 1 |
1.08 (0.26,4.53) 2.12 (0.42,10.68) 1.19 (0.11,12.43) 1 |
0.91 0.36 0.88 |
| Family size <3 3-4 >5 |
11 (9.6%) 19 (16.7%) 84 (73.7%) |
48 (21.0%) 50 (21.8%) 131 (57.2%) |
1 1.66 (0.71, 3.85) 2.80 (1.38, 5.69) |
1 0.90 (0.25,3.20) 2.28 (1.04,8.22) |
0.87 0.01* |
| Wealth index Poor Medium Rich |
87 (76.3%) 20 (17.5%) 7 (6.1%) |
124 (54.1%) 44 (19.2%) 61 (26.6%) |
6.12 (2.67,14.00) 3.96 (1.54,10.18) 1 |
1.33 (0.19,9.32) 0.65 (0.08,5.06) 1 |
0.77 0.68 |
| Decision on Money Mostly by husband Both Mostly by wife |
90 (78.9%) 13 (11.4%) 11 (9.6%) |
28 (12.20%) 177 (77.3%) 24 (10.5%) |
7.01 (3.06,16.09) 0.16 (0.07,0.40) 1 |
1.54 (0.40,5.85) 0.26 (0.07,0.96) 1 |
0.53 0.04* |
| Latrine Yes No |
96 (84.20%) 18 (15.8%) |
217 (94.8%) 12 (5.2%) |
1 3.39 (1.57,7.32) |
1 2.92 (0.58,14.56) |
0.19 |
| Water sources From pipe From spring From river |
49 (43.0%) 15 (13.2%) 50 (43.9%) |
175 (76.4%) 28 (12.2%) 26 (11.4%) |
1 1.91 (0.95, 3.86) 6.88 (3.88,12.14) |
1 2.63 (1.01,12.22) 5.61 (2.04,27.03) |
0.048* 0.001* |
*Statistically Significant factors
Table 3: Determinants of acute malnutrition among under-five children in Karat public health facilities in 2016.
Discussion
Determinants which significantly associated with acute malnutrition in this finding were; duration of child breast feeding, dietary diversity, diarrheal infection, educational status of mothers, marital status of mothers, family size of household, decision on consumption of household and water source for drinking.
Among child feeding practice factors children whose mothers feed breast milk less than one year were 3.02 times more likely to develop acute malnutrition as compared to those feed breast milk above 24 months. But children feed breast milk from 13-24 months were not significantly associated with acute malnutrition. This result is consistent with a study done in Tigray, Northern Ethiopia and Shire Indaselassie Zone, Northern Ethiopia that reveals duration of breastfeeding were significantly associated with wasting of children and mothers who stop breast feeding early expose their child for acute malnutrition due lack sufficient nutrients as well as more likely to risk for infection [2,14]. This is also agreed with a study done in Karnataka, India: a case control study revealed that breast feeding for more than one year is a protective effect on child under nutrition and have shown that early cessation of breastfeeding is a risk factor for acute under nutrition [15].
However, the study conducted in East Wollega zone, western Ethiopia did not consistent to the above findings even if breast feeding less than 12 months were shown with high odds of ratio. This non significance value (the absence of association) might be due to chance as the study itself explained [16].
Mothers who feed their child less than or equal to 3 food groups were 5.13 times more likely to develop acute malnutrition as compared to who feed greater than three food groups. This finding is in lined with a study conducted in rural area of Sidama, South Ethiopia, which stated that dietary diversity score had positively associated with children under nutrition [17].
Dietary diversity has been recognized early by nutritionists as a key element of high quality diets. It is associated with overall quality and nutrient adequacy of the diet in low-income countries including Ethiopia. Therefore, mothers who have poor practice of dietary diversity feeding expose their child for infection due to poor immunity.
A Child breast feeding practice like squeezed out first birth breast milk did not have significant association with acute malnutrition in this study. This result is contradicted with study conducted in Machakel Woreda, Northwest Ethiopia [13], Which revealed that children whose mothers squeezed out of first breast milk following delivery were more likely to have malnutrition as compared to those children’s whose mothers not Squeezed out of first breast milk just following delivery. This difference may appear due to the habit of the community in the study area, Karat town. Since, in the study area mothers have the habit of feeding first breast milk (colostrum) to their infant immediately after birth without squeezed out of their first milk (colostrum).
Morbidity factors of children by diarrheal disease were 8.41times more likely to develop acute malnutrition as compared to their counterpart. This consistent with a study conducted in West Gojjam, Addis Ababa and Oromia region [18-20]. Diarrhea is the leading cause of morbidity and mortality of children through dehydration and malnutrition. High magnitude of malnutrition observed among children who had diarrhea. This is clear because there is a reciprocal relationship with diarrhea leading to malnutrition and malnutrition predispose to diarrhea. Diarrheal diseases in children under the age of five are an indicator of lack of basic sanitation and its existence of episode between 4 up to 7 times in Ethiopia. Another study conducted in Sub Saharan African countries also stated that diarrhea is a major factor contributes to malnutrition [18,21]. Infections play a major role in the etiology of under nutrition because they result in increased needs and high energy expenditure, lower appetite, nutrient losses due to vomiting, diarrhea, poor digestion, mal-absorption and the utilization of nutrients and disruption of metabolic equilibrium [22]. As current studies conducted in different countries, presence of diarrheal morbidity two weeks prior to data collection was the major contributing factor for acute malnutrition [23,24].
Among socio demographic factors children of mothers who had no formal education 4.7 times and those who were elementary education 3.01 times more likely their child to develop acute malnutrition as compared to those children of mothers who had educational status secondary and above secondary, respectively. This finding in lined with different studies which were conducted in Kenya, at Lalibela town, which revealed, children of mothers with a higher education were less likely their child to acute malnourished than children of mothers with no education, and those children whose mothers’ had no formal education were 4 times more likely to be acute malnourished [25,26]. The other study conducted in Southern Ethiopia, Shashogo Woreda: a case control study which revealed that children of illiterate mothers were 8.67 times more likely to be their child acute malnourished [4], which consistent with this finding even though the odd ratio is higher in ShashogoWoreda. Furthermore, the other study conducted in Nepalese agreed with this finding and interrelated the maternal education with dietary diversity feeding practice of their children; as mothers more educated they feed their children more diversified foods; that it says, children whose mothers were well educated and had a secondary level education 2.6, or higher education 3.25 times more likely to meet the minimum dietary diversity compared to children whose mothers did not have any formal education, indicating an increase in the odds of providing a diversity of foods with an increase in education level [27].
This shows that improved maternal education enhances mother’s knowledge and practice towards child feeding practice, and empowers them to involve in better economic status than their counterpart. Thus, this can be hypothesized as the maternal education may simply be a proxy for child under nutrition factors such as childrearing practice, health seeking behavior or feeding practice which directly affects the children’s health.
Children whose parents’ currently not together (other than married) were 3.33 times more likely to develop acute malnutrition as compared with those who live currently together (married). This finding is in lined with a study done in North Wollo zone, Northern Ethiopia, which states the odds of under nutrition for children born to mothers who were not married were 8.6 higher than those who were currently live together [26]. This finding also supported by a recent study conducted in Bule Hora district, Southern Ethiopia, which showed that children of mothers who were not currently live with their husband were significantly associated with acute malnutrition of children [23]. This is the fact that mothers who had responsibility of child caring do not get sufficient income to fulfill child feeding demand. As a result of this low economic status, their child may develop acute malnutrition.
Children who live in family size greater than five were 2.28 times more likely to develop acute malnutrition as compared with family size of less than three. This is consistent with studies conducted in North Rural Nigeria, Rural Village of North Wollo and Gondar University Hospital. The effect of a large family size with overcrowding and inadequate spacing has been implicated as a risk factor for acute malnutrition in different studies as well [28,29]. This is also in lined with a study done in Tigray, Northern Ethiopia, stated children in high number of family size in a single household were associated with in a high odd ratio of under nutrition of children [2]. This supports the notion that nonnutritional factors should be essential components in the effort to reduce acute malnutrition in Ethiopia. This is due to the fact that mothers who had more Children may not have appropriate child feeding care and nearby mother intimacy. However, this finding contradict with a study done in Bangladesh which reveals that number of children in the household appeared to have no significant effect on nutritional status of children [30]. This difference might be due to population life style, level of development and economical variation.
Both husband and wife joint decision on house hold consumption was 74% less likely to develop acute malnutrition as compared to wife decision alone. This result supported by a study conducted in Shashogo Woreda, Southern Ethiopia, Machakel Woreda, Northwest Ethiopia [4,9]. As explained from these studies, individual decision making on household consumptions was significantly associated with acute malnutrition. However, in this study father decision alone on household did not have statistical association. But a study conducted in north part Ethiopia did not agreed, and revealed children whose fathers mostly made decision on household consumption were 5.7 times more likely to have acute malnutrition as compared to those children’s whose both parents made decision jointly [4,13,14]. This may due to cultural difference and study design. Lack of joint decision-making strategy on the care or treatment of the child has significantly affected children’s nutritional status. Based on the extensively reviewed literatures of this study the role of parental decision making pattern was found to be the first of its kind in affecting acute child under nutrition. The odds of acute under nutrition were higher among children from families who made decision individually on the care or treatment of their sick children compared with the children whose families have made decision jointly on the issue. This could be explained by the fact that the provision of joint care by biological parents requires joint decision on the care or treatment of their children in order to improve children’s nutritional status. Such decision might also require women’s autonomy to participate in the decision making process of the household equally with the men [31].
In this study, Among socio demographic factors sex and wealth index of the household of the children did not significantly associated with acute malnutrition which is consistent to the study done in Shashogo Woreda, Southern Ethiopia; case control study. But a study done in northern Uganda, contradict with the above finding regarding to sex, which revealed male child is 2 times more likely to suffer from acute malnutrition compared to females [4,32]. This may be due to population dynamics and demographic setup.
Among environmental factors children who consume water from unprotected source (river 5.61and spring water 2.63 times more likely to develop acute malnutrition as compared to who use protected (pipe water) source. This is supported by study done in Democratic Republic of Congo, Iran, Nigeria (Kwara state) and Amhara region northwest Ethiopia and rural Ethiopia [13,18,33,34]. In the rural population of Ethiopia, there is lack access of safe drinking water is the major environmental problems for the transmission of common diseases. Lack of access to safe drinking water and unprotected drinking water is closely related to incidence or episode of water borne diseases like diarrhea which contribute malnutrition. In addition to this lack of access to drinking water (it estimated that more than two thirds of the population has no access to drinking water) is a direct causes of malnutrition [18]. This is also consistent to the study done in Tigray, Northern Ethiopia, which revealed, using unprotected sources of water in the household of children were 2 times more likely under nutrition as compared with those who consumed protected water [2].
Strength and limitation of the study
It is possible that selection bias may occur since controls were selected from institutions, but efforts were made to differentiate cases and controls through clinical assessment (child history and physical examination) and additionally, made two controls for a single case to minimize such type of selection bias.
Recall bias tried to minimize through
Data collectors: who were experienced nurses and public health officers who know local languages and community practices (using different techniques: mix long and short questionnaire, detailed respondent instructions, feedback-inform respondent how well performed and commitment techniques-sign of agreement to respondents conscientiously). Data collectors helped mothers try to recall by local event recalls (local holidays). By keeping recall questions to minimum.
Conclusion
This study identifies different determinants of acute malnutrition; the determinant factors that significantly affect acute malnutrition in this study area were almost consistent with research findings conducted from developing countries and other study areas in our country. In this finding the major determinants associated with acute malnutrition of under-five children classified as child characters and maternal related factors; children characteristics related factors were: total duration of breast feeding of children less than a year, children consumed dietary diversity less than or equal to three food groups and children who were exposed to diarrhea. Whereas, the maternal related factors were: children of mothers who had no formal education and primary education, children of household who consumed water from unprotected source (river and spring water), family size>5 and lack of joint decision of parents on the household consumptions of goods were the major determinates that significantly associated with acute malnutrition of under-five children in Karat public health facilities. The most interesting determinant from this finding was children morbidity of diarrheal disease, source of drinking water of the household and dietary diversity feeding practice of the children. However, among the important factors, wealth index did not significantly associated with acute malnutrition in this finding. This may be due to the data collection period, which carried on February 28 to April 13, 2016, which were the times that in which most household were secured for food.
Recommendations
Based on the findingsof the study the following recommendations are made:
Mothers should feed breast milk to their children more than a year and after six months she ought to give to her children more than three food group types. Drinking water should be treated by using local accessible material before utilize. Mothers and fathers should be jointly decided on consumptions of the household.
Health professional should give counseling to mothers about family planning in order to utilize it.
Health professionals should give health education to mothers about child feeding and breast feeding practice.
Develop protected water source accessibility and improving water quality by using different filtration.
Focus on developing and well integrating on nutrition programs for acute malnourished children of under-five to improve their nutritional status and dietary quality based on local context; to reduce burden of acute malnutrition of under-five children on community
Further study should be carried out in prospective longitudinal survey to see deeply the cause-effect relationship of factors with AMN integrating with qualitative study design to understand deeply socio-cultural and behavioral related factors towards acute malnutrition of under-five children which is consistent in the study area.
Acknowledgement
Our deepest gratitude goes through the data collectors for their devotion and patience during the data collection period.
Funding
The work was funded by College of Medicine and Health Sciences, Arba Minch University.
Authors’ Contribution
PI- Initiated the research, wrote the research proposal, conducted the research, did the data entry and analysis and wrote the manuscript. The Co-authors- edition made, advising, cooperatively tool prepared with PI and prepared the manuscript.