- (2008) Volume 9, Issue 6
Philip D Hardt1, Nils Ewald1, Kristian Bröckling1, Shoichiro Tanaka2, Toyoshi Endo2, Hans U Kloer1, Reinhard G Bretzel1, Clemens Jaeger1, Hiroki Shimura2, Tetsuro Kobayashi2
1Third Medical Department, University Hospital Giessen and Marburg. Giessen, Germany
2Third Department of Internal Medicine, Interdisciplinary Graduate School of Medicine and Engineering, University of Yamanashi. Yamanashi, Japan
Received July 24th, 2008 - Accepted August 14th, 2008
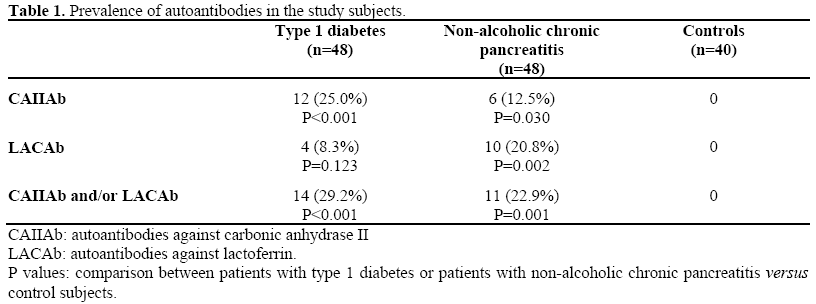
Context Histopathological analysis has demonstrated lymphocytic infiltration in both the endocrine and the exocrine pancreas in some patients with type 1 diabetes and nonalcoholic chronic pancreatitis, suggesting an immune-mediated mechanism which affects both diabetes mellitus and chronic pancreatitis. Objective The examination of exocrine pancreatic humoral markers in Caucasian patients with respect to the interactions between exocrine and endocrine pancreatic diseases. Patients One hundred and thirty-six European Caucasian subjects subdivided into three groups: type 1 diabetes (n=48); non-alcoholic chronic pancreatitis (n=48); controls (n=40). Main outcome measure Autoantibodies against carbonic anhydrase II (CAIIAb) and lactoferrin (LACAb) (both of which are exocrine pancreatic antigens) were analyzed by enzyme-linked immunosorbent assay. Results No positivity for CAIIAb and LACAb were found in the controls. Patients with type 1 diabetes had a significantly higher prevalence of CAIIAb (25.0%) than the controls while the prevalence of LACAb (8.3%) was not significantly higher than the controls. The prevalence of CAIIAb (12.5%) and LACAb (20.8%) in the patients with nonalcoholic chronic pancreatitis was significantly higher than that in the controls. A significantly higher prevalence of CAIIAb and/or LACAb was found in patients with type 1 diabetes (29.2%) and non-alcoholic chronic pancreatitis (22.9%) compared to that in the controls (0%). There was a significant association between CAIIAb and LACAb titers both in patients with type 1 diabetes (P=0.042) and in patients with non-alcoholic chronic pancreatitis (P<0.001). Conclusion We have clearly demonstrated that some European Caucasian patients with type 1 diabetes and non-alcoholic chronic pancreatitis have autoantibodies against the exocrine pancreatic antigens CAIIAb and LACAb.
Autoantibodies; Autoimmunity; Diabetes Mellitus; Pancreatitis, Chronic
CAIIAb: autoantibody against carbonic anhydrase II; GADAb: antibodies against glutamic acid decarboxylase; IA-2Ab: insulinoma-associated antigen 2; ICA: islet cell antibodies; IDFu: Immunology of Diabetes Federation units; LACAb: autoantibody against lactoferrin
Impairment in both pancreatic endocrine and exocrine function has been reported in diabetes mellitus [1, 2, 3, 4, 5]. Histological analysis has demonstrated that patients with type 1 diabetes frequently have lymphocytic infiltration in the exocrine as well as in the endocrine pancreas [6]. Lymphocytic infiltration in the exocrine and the endocrine pancreas has also been reported in patients with autoimmune pancreatitis [7] which is a subtype of non-alcoholic chronic pancreatitis and is frequently associated with diabetes [8, 9]. Furthermore, in Japanese patients with autoimmune pancreatitis and type 1 diabetes, it has been reported that there is the presence of autoantibodies against exocrine pancreatic antigens (i.e., autoantibodies against cytokeratin, carbonic anhydrase II (CAIIAb) and lactoferrin (LACAb)) [9, 10, 11]. These findings suggest that a common autoimmunemediated mechanism involves the exocrine as well as the endocrine pancreas in type 1 diabetes and non-alcoholic chronic pancreatitis.
However, the presence of these autoantibodies against exocrine pancreatic antigens is still not clear in Caucasian populations. In this study, we examined the existence of CAIIAb and LACAb in European Caucasian patients with type 1 diabetes and non-alcoholic chronic pancreatitis, and compared it to controls.
One hundred and thirty-six European Caucasian subjects were studied
Patients
Type 1 Diabetes Mellitus
This group was made up of 48 newly diagnosed patients (male/female: 25/23; mean age: 12.7 years, range: 4-56 years) according to the WHO criteria [12]. All patients were ketosis-prone insulin-dependent at the onset.
Non-Alcoholic Chronic Pancreatitis
This group included 48 patients (male/female: 32/16; mean age: 57.3 years, range: 21-82 years; mean duration: 18.9 months) with proven pancreatic duct changes of at least grade II according to the Cambridge classification [13] and/or a reduced exocrine function according to low (<200 μg/g) fecal elastase-1 concentrations [14]. All of them were non-alcohol users and did not have pancreatic ductal calculi
Controls
The control group included 40 subjects without diabetes, pancreatitis, or rheumatic or autoimmune thyroid diseases (male/female: 22/18, mean age: 57.4 years, range: 21-77 years). Gender (P=0.314) was not significantly different among the three groups of subjects,. Age was also not significantly different between the non-alcoholic chronic pancreatitis group and the control group (P=0.970) whereas the type 1 diabetes mellitus group was significantly younger (P=0.001) as compared to both non-alcoholic chronic pancreatitis patients and controls.
Laboratory Methods
Islet Cell Antibodies (ICA), Antibodies Against Glutamic Acid Decarboxylase (GADAb) and Insulinoma-Associated Antigen 2 (IA-2Ab)
ICA was determined by indirect immunfluorescence using pancreatic tissue slides from healthy human donor blood group 0 [15]. After incubation with test sera for 75 minutes, the probes were washed and diluted with PBS buffer. After another incubation of 45 minutes, the different dilution steps were analyzed by immunofluorescence microscope. The titer was converted to Immunology of Diabetes Federation units (IDFu) using an international reference serum of 20 IDFu. Sera with more than 10 IDFu were judged as positive.
The determination of GADAb and IA-2Ab was performed by RIA using the CentAK® anti GAD65 (Medipan Diagnostica, Selchow, Germany) and the CentAK® anti IA2 (Medipan Diagnostica, Selchow, Germany), respectively.
Antibodies Against Carbonic Anhydrase II (CAIIAb) and Lactoferrin (LACAb)
CAIIAb and LACAb were measured using enzyme-linked immunosorbent assays as previously described [9, 11]. The absorbance levels were expressed as optical density (OD) at 450 nm. In the CAIIAb assay, inter- and intra-assay coefficients of variation (CV) were 9.7% and 2.2%, respectively. In the LACAb assay, inter- and intra-assay CV were 10.8% and 4.1%, respectively. Positive results were defined as absorbance values higher than the mean + 2 SD of the control samples.
Plasma Samples
Plasma samples from the subjects were collected prospectively after informed written consent was obtained. The samples were frozen and stored at -80°C until assay
Written informed consent was obtained from each patient. The study protocol was confirmed by the ethical committee of Giessen University Hospital. It conforms to the ethical guidelines of the "World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects" adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964 as revised in Tokyo 2004 and as reflected in a priori approval by the appropriate institutional review committee.
Data are reported as mean±SD. The Mann- Whitney U and Fisher's exact tests were used to determine the differences in the titers and the prevalence of antibodies between the different subjects groups, respectively. The Spearman correlation was used to describe the relationship between the different antibodies. The Pearson chi-squared and the Mann- Whitney tests were used to compare age and gender among the three groups of subjects. The data were analyzed by means of the JMP software (version 5). Two-tailed P values of less than 0.05 were considered statistically significant.
The Absorbance Levels of CAIIAb and LACAb
The absorbance levels of CAIIAb in type 1 diabetic patients (0.283±0.026 OD) were significantly higher when compared to those in patients with non-alcoholic chronic pancreatitis (0.265±0.029 OD, P=0.003) and the control subjects (0.260±0.016 OD, P<0.001) (Figure 1a). The absorbance levels in CAIIAb in non-alcoholic chronic pancreatitis did not significantly differ from those in the control group (P=0.315). The absorbance levels of LACAb in type 1 diabetic patients (0.246±0.035 OD) and nonalcoholic chronic pancreatitis (0.253±0.059 OD) were significantly higher when compared to those in the controls (0.229±0.036 OD, P=0.040 and P=0.039, respectively) (Figure 1b). There was no significant difference of LACAb levels between type 1 diabetes and non-alcoholic chronic pancreatitis (P=0.611). A significant positive correlation between the levels of CAIIAb and LACAb was recognized both in patients with type 1 diabetes (rs=0.295, P=0.042) and in those with non-alcoholic chronic pancreatitis (rs=0.734, P<0.001) (Figure 2).
The Prevalence of Positive Findings of CAIIAb and LACAb
The prevalence of CAIIAb in type 1 diabetic patients (25.0%, 12/48) was significantly higher (P<0.001) when compared to that in the control subjects (0%, 0/40) while the prevalence of LACAb in type 1 diabetic patients (8.3%, 4/48) did not significantly differ (P=0.123) from that found in the controls (0%, 0/40) (Table 1). The frequencies of CAIIAb (12.5%, 6/48) and LACAb (20.8%, 10/48) in non-alcoholic chronic pancreatitis patients were significantly higher than those in the control group (P=0.030 and P=0.002, respectively) (Table 1). The prevalence of CAIIAb and/or LACAb in type 1 diabetic patients (29.2%, 14/48) and non-alcoholic chronic pancreatitis patients (22.9%, 11/48) was significantly higher than that in the controls (0%, 0/40, P<0.001 and P=0.001, respectively) (Table 1).
Prevalence of Islet-Related Autoantibodies (ICA, GADAb and IA-2Ab) in Patients with CAIIAb and/or LACAb and Patients without CAIIAb or LACAb
All patients in the type 1 diabetes group were positive for ICA while no control subjects were positive for ICA (P<0.001) (Table 2). Significantly higher prevalences of GADAb (22.9%, 11/48; P=0.005) and IA-2Ab (12.5%, 6/48; P=0.030) were found in type 1 diabetic patients when compared to the control subjects (GADAb: 2.5%, 1/40; IA-2Ab: 0%, 0/40). Out of 14 type 1 diabetic patients with CAIIAb and/or LACAb, 2 patients had GADAb (14.3%) and one (7.1%) had IA-2Ab (Table 2). The prevalence of GADAb and IA- 2Ab in type 1 diabetic patients without CAIIAb and LACAb was 26.5% (9/34) and 14.7% (5/34), respectively.
In patients with non-alcoholic chronic pancreatitis having neither CAIIAb nor LACAb, the prevalence of ICA, GADAb and IA-2Ab was 2.7% (1/37), 8.1% (3/37) and 2.7% (1/37), respectively (Table 2). In the 11
patients with non-alcoholic chronic pancreatitis having CAIIAb and/or LACAb, one patient had GADAb (9.1%). There was no significant difference of prevalence of islet-related autoantibodies (ICA, GADAb and IA-2Ab) between those with CAIIAb and/or LACAb and those without CAIIAb or LACAb both in patients with type 1 diabetes and in patients with non-alcoholic chronic pancreatitis (Table 2).
We demonstrated a significantly higher prevalence of serum autoantibodies against exocrine antigens (CAIIAb and/or LACAb) in Caucasian patients with type 1 diabetes and non-alcoholic chronic pancreatitis as compared to controls. The prevalence of both CAIIAb and LACAb were similar to the observations of another recently published European study in patients with type 1 diabetes [16]. Surprisingly, this study found that the prevalence of autoantibodies against carbonic anhydrase in children was much lower as compared to adults. This observation could be explained if autoimmunity against exocrine tissue was a secondary phenomenon, developing during the time course of type 1 diabetes. On the other hand, in the present study, the frequency of islet-related autoantibodies did not significantly differ between patients with autoantibodies against exocrine antigens and those without autoantibodies against exocrine antigens in both type 1 diabetes and non-alcoholic chronic pancreatitis patients, suggesting that exocrine involvement caused by an immunemediated mechanism exists in some patients with type 1 diabetes and non-alcoholic chronic pancreatitis independently of endocrine involvement.
This immune-mediated involvement against pancreatic exocrine antigens may be an epiphenomenon secondary to damage of the exocrine pancreas and destruction of the pancreatic islets. However, this involvement of the exocrine pancreas might be related to the pathophysiology of type 1 diabetes and non-alcoholic chronic pancreatitis. Furthermore, the possibility that this autoimmunity against exocrine pancreatic tissue might be a primary cause of type 1 diabetes and non-alcoholic chronic pancreatitis and that the difference of genetic and/or environmental factors in each patient determines the course of the disease thereafter cannot be ruled out.
In this study, we recognized the close correlation between CAIIAb levels and LACAb levels (Figure 2); the prevalence of CAIIAb and LACAb in non-alcoholic chronic pancreatitis patients was also significantly higher than that in the control group. However, patients with type 1 diabetes had a significantly higher prevalence of CAIIAb than the control group while the prevalence of LACAb was not significantly higher than in the control group. Carbonic anhydrase II is localized in pancreatic ductal cells while lactoferrin is localized in pancreatic acinal cells [17]. It is known that islet precursor cells are also localized in the pancreatic ducts [18]. The discrepancy in the prevalence of autoantibodies against pancreatic exocrine antigens in patients with type 1 diabetes suggests an immune-mediated mechanism directed towards the islet precursor cells located in the pancreatic ducts. The inhibition and/or destruction of neogenetic islets from pancreatic ducts caused by an immunemediated mechanism might be related to the progression of beta-cell failure in patients with type 1 diabetes.
Autoimmune pancreatitis, a subtype of chronic pancreatitis, characterized by diffuse/focal pancreatic swelling, irregular narrowing of a main pancreatic duct and lymphocytic infiltration of the exocrine pancreas frequently has autoantibodies against an exocrine pancreas [8, 9]. We have reported that patients with this subtype of non-alcoholic chronic pancreatitis frequently have diabetes mellitus, and that lymphocytic infiltration into and around the pancreatic islets was observed in autoimmune pancreatitis [9]. Surprisingly, steroid treatment recovered or improved diabetes mellitus associated with autoimmune pancreatitis [8]. In this study, no patient met with the criteria of autoimmune pancreatitis as suggested by the Japan Pancreas Society [19]. However, patients with type 1 diabetes having autoantibodies against exocrine pancreatic antigens might nevertheless improve their glucose intolerance using steroid treatment.
We demonstrated that some patients with type 1 diabetes and non-alcoholic chronic pancreatitis had autoantibodies against an exocrine pancreas. Patients with type 1 diabetes and exocrine antibodies might belong to the group that Taniguchi et al. have recently described [11]. The presence of exocrine autoantibodies in patients with nonalcoholic pancreatitis might be related to some type of autoimmune process different from classical autoimmune pancreatitis as they do not fulfill the criteria [19]. Further studies are needed to clarify the meaning of autoantibodies against an exocrine pancreas in these patient groups.
We thank Mr. T. Hughes for his editorial assistance
The authors have no potential conflicts of interest