- (2013) Volume 14, Issue 3
Sarah A Henry, Anna E Prizment, Kristin E Anderson*
Division of Epidemiology and Community Health, School of Public Health, University of Minnesota; University of Minnesota Masonic Cancer Center. Minneapolis, MN, USA
Received December 5th, 2012 – Accepted March 23rd, 2013
Context Studies have shown a relationship between history of diabetes and the risk of pancreatic cancer; however, the temporal relation between diabetes and pancreatic cancer is not clearly established. Objectives Diabetes and diabetes duration were examined in relation to pancreatic cancer in a population-based case-control study and prospective cohort. Methods Case-control study: pancreatic cancer cases (n=200) from the Midwest were frequency matched by age and sex to population controls (n=673). Logistic regression yielded odds ratios (ORs) and 95% confidence intervals (95% CI). Iowa Women’s Health Study (IWHS) cohort: 292 incident pancreatic cancer cases occurred between 1986-2008 among 36,084 post-menopausal, initially cancer-free women. Diabetes status and diagnosis age were ascertained at baseline and follow-ups. Proportional hazards regression yielded hazard ratios (HR, 95% CI) for pancreatic cancer in relation to baseline diabetes. Time-dependent analyses accounted for diabetes diagnosed after baseline. A nested-case control analysis assessed diabetes duration as a risk factor. Results In the case-control study, compared to participants without diabetes, the multivariate ORs (95% CI) for pancreatic cancer were 2.35 (1.24-4.47) for those with diabetes and 4.00 (0.94-16.9), 2.79 (0.97-8.04), and 2.40 (0.97-5.98) for diabetes durations of 2-5 years, 5.1-10 years, and more than 10 years, respectively. In IWHS, compared to no diabetes, multivariate-adjusted HRs for pancreatic cancer were 1.86 (1.23-2.83) for baseline diabetes and 1.94 (1.40-2.69) adding diabetes during follow-up. In an IWHS nested case-control analysis, ORs were 1.70 (0.78- 3.67), 2.62 (1.48-4.65), and 2.10 (1.36-3.24) for diabetes durations of 2-5 years, 5.1-10 years and more than 10 years, respectively, versus no diabetes. Conclusions Diabetes is associated with pancreatic cancer risk and this is similar across different duration categories.
Case-Control Studies; Cohort Studies; Diabetes Mellitus; Pancreatic Neoplasms
Pancreatic cancer is a devastating disease with a 5-year survival rate of just 5% [1, 2] and an average survival rate of five to six months [1]. While only the tenth most common cancer in the United States, pancreatic cancer is the fourth most common cause of cancer death [3]. Currently, little is known about the etiology of pancreatic cancer. The only well-established risk factors are age [4, 5, 6], cigarette smoking [4, 5, 6, 7, 8] and a family history of pancreatic cancer [4, 5, 8].
Another possible risk factor is diabetes. Many studies have investigated the association between pancreatic cancer and diabetes mellitus and most have reported a positive association. Fewer studies have examined duration of diabetes relative to pancreatic cancer risk and the findings are inconsistent; moreover, studying this association is complicated by the fact that cancer in the pancreas often causes diabetes [2, 5, 7, 8, 9, 10]. We investigated the association between diabetes and pancreatic cancer with particular focus on duration of diabetes [4, 7, 9]. A better understanding of the association may yield clues to etiology of cancer of the pancreas or may help in devising early markers for this cancer, which is usually diagnosed at late stages when the prognosis is very poor.
We examined this relationship in two population-based studies: one, a population-based case-control study in the Midwest of the United States and the other, a wellestablished prospective cohort (the Iowa Women’s Health Study (IWHS)).
Case-Control Study Design and Analysis
The design and methods of this case-control study, conducted in 1994-1998, have been described in detail elsewhere [11, 12]. Cases (20 years or older) were subjects with newly diagnosed cancer of the exocrine pancreas according to the code C25 of the International Classification of Disease for Oncology, third edition (ICD-O-3) [13]).
Prior to inclusion in the study, pathology reports of potential cases were reviewed by a pathologist or confirmed through the Minnesota Cancer Surveillance System (MCSS, https://www.health.state.mn.us/divs/ hpcd/cdee/mcss/) for eligibility. The cases were ascertained from all hospitals in the metropolitan area of the Twin Cities and a series from the Mayo Clinic. Because half of the patients with pancreatic cancer die within a few months after their diagnosis, a rapid caseascertainment system was used to enroll cases. The median number of days between diagnosis and the first contact for the study was 13 days [11, 12]. Controls were randomly selected from the general population from Minnesota Driver’s License or Health Care Financing Administration (now Centers for Medicare and Medicaid Services; CMS, https://www.cms.gov/) databases and frequency matched to cases by sex and age at diagnosis (within 5 years).
All subjects were interviewed in-person regarding demographic factors, lifestyle behaviors, history of medical conditions, the age of the diabetes onset, and insulin use. Anthropometric characteristics were not measured in participants as cases may have experienced rapid weight loss prior to diagnosis. Omission of questions on previous weight and height in the questionnaire was an oversight. Diabetes was defined as onset at age 30 years or older, thus subjects who self-reported a diabetes onset prior to 30 years of age were excluded from this analysis; those with presumptive type 2 diabetes constituted the majority of diabetes cases. In addition, since diabetes that occurs less than 2 years prior to pancreatic cancer is often considered a symptom of the cancer [14, 15, 16], subjects who had been diagnosed with diabetes less than 2 years before their index dates were treated as not having diabetes. Diabetes duration was calculated by subtracting the age of diabetes diagnosis from the age of pancreatic cancer diagnosis for cases or age at match date (the index date) for controls. To facilitate comparisons to previous reports, three diabetes duration categories were created: 2-5, 5.1-10 and more than 10 years.
In this analysis, there were 200 pancreatic cancer cases and 673 controls. Demographic, lifestyle and other characteristics between pancreatic cancer cases and controls were compared using the t-test for continuous variables and the chi-square test for categorical variables. Unconditional logistic regression was used to estimate multivariate-adjusted odds ratios (ORs) of pancreatic cancer and 95% confidence intervals (95% CI) in relation to history of diabetes and its duration. We also examined ORs for individuals with diabetes, stratified by reported insulin use (yes or no), versus those without diabetes. Multivariate-adjusted models included age, sex, race, education (less than high school, high school, post high school), cigarette smoking (smoking status: current, former and never, and pack-years), and alcohol use (current intake versus no current intake). Further adjustment for physical activity, consumption of total calories, total fat or total fiber did not substantively change the associations and those variables were not included in final models. Further, we tested whether or not sex and smoking status modified associations between diabetes and pancreatic cancer by testing for interactions of smoking status and sex with diabetes. Since all P values for interactions were more than 0.15, interaction terms were not included in final models.
Cohort Study Design and Analysis
A detailed description of the Iowa Women’s Health Study (IWHS) design has been previously presented [17]. Briefly, the IWHS is a prospective cohort study that started in 1986 with 41,836 postmenopausal women from Iowa who were between the ages of 55 and 69 years at baseline. In addition to the original survey, five follow-up surveys were sent to study participants in 1987, 1989, 1992, 1997, and 2004 (response rates were 91%, 90%, 83%, 79%, and 69%, respectively). Through these surveys, information was collected on anthropometric measures, dietary habits, personal and family health history, and demographics. Prevalent and incident cases of diabetes were assessed through self-report on the baseline survey or one of the follow-up surveys (at which the participants reported for the first time being diagnosed with diabetes). Like the case-control study, all women with diabetes diagnoses that preceded a pancreatic cancer diagnosis by less than 2 years were considered not to have diabetes for these analyses. At baseline, in two separate questions, subjects reported whether or not they used insulin and/or other medication for diabetes. Diabetes duration for women reporting diabetes at baseline was calculated by subtracting age at diabetes diagnosis from baseline age. Participants were excluded from analysis if they reported having had cancer at baseline (except non-melanoma skin cancer) (n=3,830), were not menopausal (n=569), or were diagnosed with diabetes before age 30 (n=84). Additionally, participants with missing data for the following variables were excluded: pack-years of cigarette smoking, smoking status, education and baseline diabetes status.
Incident cancers and dates of diagnosis were obtained through the Iowa State Health Registry, which is a part of the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER, https://www.seer.cancer.gov/) program. ICD-O-3 codes [13] were used to establish eligibility of cases. Only subjects with exocrine pancreatic cancers, which comprise 95% of pancreatic malignancies, were included into the analysis. All other pancreatic tumors, including islet cell tumors, sarcomas, and lymphomas, were excluded. After exclusions, the analytic cohort was n=36,084 with 292 cases of pancreatic cancer.
The association between baseline diabetes and pancreatic cancer was assessed using a proportional hazards regression model. Hazard ratios (HRs) and their corresponding 95% CIs were computed in multivariate-adjusted analyses. To assess the association between diabetes and pancreatic cancer while accounting for diabetes diagnosed both before and after baseline, a time dependent analysis was conducted. Baseline variables that were tested as potential confounders in this study included age, body mass index (BMI: weight/height2, kg/m2), smoking status (current, former, never), continuous pack-years, diabetes diagnosis date, education status (less than high school graduate, high school graduate, and post high school graduate), multivitamin use, and alcohol consumption (current intake versus no current intake). The final model included age, smoking status, packyears, education, and BMI. A potential effect of diabetes treatment (either oral medication or insulin) on the risk of pancreatic cancer was assessed by stratifying those with diabetes as ever- or never-treated and compared to those without diabetes.
Associations between duration of diabetes and pancreatic cancer were analyzed with a nested-case control design in the IWHS cohort using conditional logistic regression with multivariate adjustment. Ten controls were matched to each case on year of birth and vital status on the year of the cancer diagnosis resulting in a sample size of 3,212 (292 cases and 2,920 controls). If more than ten controls were available for matching to a case, controls were randomly chosen from all eligible non-cases. Controls were assigned an index year matching the year of the cancer diagnosis for their case. For women with diabetes, total diabetes duration was calculated by subtracting each individual’s diabetes diagnosis year from their pancreatic cancer diagnosis year for cases or index dates for controls.
Frequencies and mean±SD were used as descriptive statistics and the Fisher’s exact, the chi-square and the Student-t tests were used to compare characteristics between pancreatic cancer cases and controls/noncases. Unconditional multivariate logistic regression was used to estimate the association of cancer with history of diabetes and its duration in the case-control study by computing ORs and their corresponding 95% CIs. The association between baseline diabetes and pancreatic cancer was assessed using a multivariate proportional hazards regression model in the cohort study (IWHS) by computing HRs and their corresponding 95% CIs. To assess the association between diabetes and pancreatic cancer while accounting for diabetes diagnosed both before and after baseline, a time dependent analysis was conducted. Associations between duration of diabetes and pancreatic cancer were analyzed with a nested-case control design in the IWHS cohort using conditional logistic regression. The statistical software SAS 9.2 (SAS Institute Inc., Cary, NC, USA) was used to conduct analyses in both studies. Two tailed P values less than 0.05 were considered significant.
The case-control study was reviewed and approved by the University of Minnesota and the Mayo Clinic Institutional Review Boards (IRB). The IWHS has been approved by the University of Minnesota’s IRB. In both studies, written informed consent was obtained from each participant.
In the Midwestern case-control study, there were 97.1% Caucasians; 61.5% of the 200 cases and 56.3% of the 673 controls were males (Table 1). The mean ages of cases and controls were 65.4 years and 66.1 years, respectively. Compared to controls, pancreatic cancer cases were more likely to smoke, to report a history of diabetes and a low physical activity level. Cases were less likely to be Caucasian, to report that they consumed alcohol and to have had post high school education (Table 1).
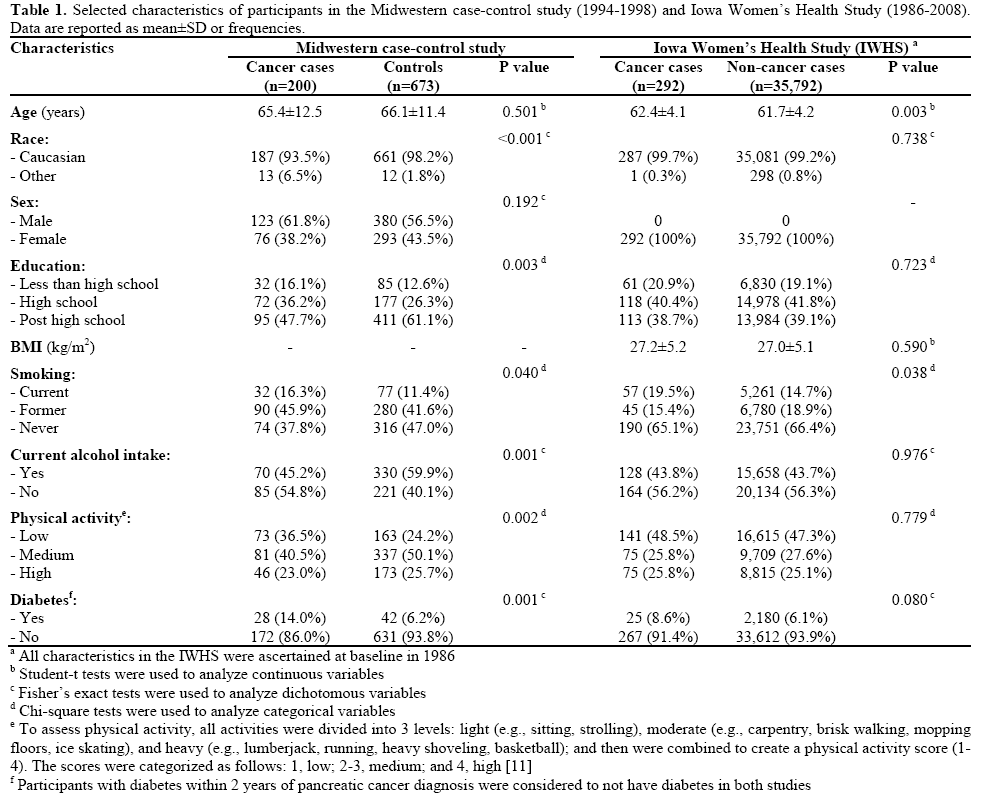
In the IWHS, 99.2% of the women were Caucasian; there were 2,205 women with diabetes at baseline. The incidence rate of pancreatic cancer among participants who were non-diabetic at baseline was 41.3 cases per 100,000 person-years of observation. For participants who were diabetic at baseline, the incidence rate of pancreatic cancer was 75.0 cases per 100,000 personyears of observation (Table 2). On average, women who had diabetes at baseline were older, had a higher BMI, and were less educated, as compared to women who did not have diabetes (data not shown). More detailed information about risk factors for pancreatic cancer among women in the IWHS has been published previously [18]. The baseline demographic characteristics for the 292 women who developed pancreatic cancer between 1986 and 2008, compared to those who did not, were very similar with the exception of age and smoking status while the difference in history of diabetes was near the level of significance (Table 1). In contrast to the findings from the Midwestern case-control study, cases and non-cases did not differ by ethnicity, educational status, alcohol intake, or physical activity level.

In the Midwestern case-control study the multivariateadjusted OR for pancreatic cancer was 2.35 (95% CI: 1.24-4.47) for those with versus those without diabetes (Table 2). When compared to subjects without diabetes, for those with diabetes who were using insulin, the OR was 3.34 (95% CI: 1.35-8.12) (Table 2), while those with diabetes who did not receive treatment had an OR of 1.50 (95% CI: 0.60, 3.81), but there were only 14 and 11 pancreatic cancer cases among the diabetic patients with and without treatment, respectively.
Similarly, women with diabetes were at increased risk of pancreatic cancer in the IWHS; after multivariate adjustment, women with diabetes at baseline had 1.86 times the hazard for pancreatic cancer (95% CI: 1.23- 2.83) than women without diabetes at baseline (Table 2). Adjusting for duration of diabetes before baseline did not substantively change the result (data not shown). HRs were also similar when diabetes was modeled as a time-dependent variable (HR=1.94; 95% CI: 1.40-2.69). Diabetic women who self-reported treatment for diabetes were 1.87 (95% CI: 1.10-3.18) times more likely than those without diabetes to develop pancreatic cancer. Diabetic women who did not receive treatment compared to those without diabetes had a HR=1.44 (95% CI: 0.64-3.25), but it was not statistically significant (Table 2).
Although BMI was not associated with pancreatic cancer risk in the IWHS (HR=1.01; 95% CI: 0.98- 1.03), other studies indicate that it is a probable causal factor for pancreatic cancer with relative risk estimates of about 1.3 [19]. To determine whether or not the association of diabetes with pancreatic cancer is independent of BMI in our cohort, we stratified by BMI categories of normal (less than 25 kg/m2), overweight (equal to, or greater than, 25 and less than 30 kg/m2) and obese (equal to, or greater than, 30 kg/m²). In a multivariate model, with additional adjustment for BMI as a continuous variable, the HR was elevated in all categories: 1.67 (95% CI: 0.68, 4.11); 2.80 (95% CI: 1.49, 5.26), and 1.32 (95% CI: 0.65, 2.67), in normal, overweight, and obese women, respectively; but it reached the significance level in overweight women only. The differences in cancer risk between BMI categories were not statistically significant (P=0.493).
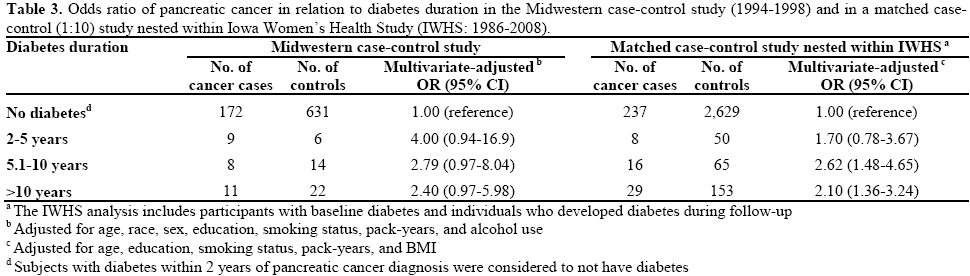
Finally, we investigated duration of diabetes in relation to pancreatic cancer risk. In the Midwestern casecontrol study, associations were elevated across all duration categories (Table 3). When compared to individuals without diabetes, the ORs for pancreatic cancer were 4.00 times higher for subjects who had diabetes for 2-5 years (95% CI: 0.94-16.9), 2.79 times higher for subjects who had diabetes for 5.1-10 years (95% CI: 0.97-8.04) and 2.40 times higher for subjects who had diabetes for more than 10 years (95% CI: 0.97-5.98) although none of them reached the significance level. The ORs for pancreatic cancer by categories of diabetes duration in the IWHS nested case-control analysis followed a similar pattern (Table 3); the comparable ORs were: 1.70 (95% CI: 0.78- 3.67), 2.62 (95% CI: 1.48-4.65), and 2.10 (95% CI: 1.36-3.24), respectively. In this study the HRs were significant both in women with a duration of diabetes of 5.1-10 years and in those with a duration longer than 10 years. Of note, although our main focus was on diabetes as a risk factor for cancer, it is of clinical interest to estimate the cancer risk associated with short-term diabetes. We estimated this in the casecontrol study: in a multivariate-adjusted model, the odds ratio of pancreatic cancer was 13.8 (95% CI: 4.8- 39.4) for those who had diabetes for less than 2 years before the index date in comparison to non-diabetic women.
We examined associations between duration of diabetes and pancreatic cancer in two population-based studies (a case-control study and a prospective cohort) and the results were relatively consistent.
In the case-control study, the OR for pancreatic cancer was 2.35 (95% CI: 1.24-4.47) for those with diabetes versus those without diabetes. The point estimates were elevated for all diabetes duration categories. Although the ORs were of borderline statistical significance in these subcategories, likely due to smaller numbers of subjects, these data are consistent with the view that the risk remains elevated over time.
Results were similar in the prospective analysis in the IWHS, where we accounted for incident diabetes over 22 years of follow up. Women diagnosed with diabetes had almost double the risk of developing pancreatic cancer compared to women without diabetes. In the nested case-control analysis within the cohort, all duration categories showed increased ORs of pancreatic cancer.
Of note, although the IWHS study included only women, whereas the case-control study included both men and women, we believe that the findings from the two studies may be compared given that there was no interaction between sex and diabetes in the case-control study (the ORs for pancreatic cancer were 2.42 for males and 1.65 for females; P=0.46). This is in line with the meta analysis by Huxley et al. who in 2005 found no effect modification, by sex, of a diabetespancreatic cancer association: 1.70 (95% CI: 1.52-1.91) for male and 1.57 (95% CI: 1.30-1.89) for females (P of interaction equal to 0.48) [7].
The 2-fold overall increased risk of pancreatic cancer for diabetic individuals diagnosed 2 or more years before cancer in both of our analyses is consistent with the results from published cohort and case-control studies [4, 7, 9, 20, 21]. Similar to our findings, in the meta-analysis published by Huxley et al. in 2005, most, but not all, of 36 studies reported an increased risk of pancreatic cancer for diabetic participants [7]. The overall estimate for the association between diabetes and pancreatic cancer (including both case-control and cohort studies) was 1.82 (95% CI: 1.66-1.99). For casecontrol studies alone (n=17), the estimate was 1.94 (95% CI: 1.53-2.46) while for cohort (or nested casecontrol) studies (n=19) it was 1.73 (95% CI: 1.59- 1.88). A large Swedish cohort, not included in the meta-analysis, also found a statistically significant risk estimate close to 2 for diabetes [9].
With respect to diabetes duration, results from previous studies are inconsistent. A meta-analysis of 9 studies with the same diabetes duration cut points, reported an inverse association between pancreatic cancer and the duration of diabetes (P<0.01) [7]. In contrast, in the Swedish cohort, risks were elevated across duration categories even after ten or more years, which is in agreement with our findings [9]. Although several other studies have reported changes in risk by diabetes duration, the data do not make a strong case for such differences. Two recent case-control studies found that the elevation in risk of cancer decreased, though not significantly, the longer people had diabetes. A large case-control study by Silverman et al. published in 1999 reported that having diabetes for a longer period of time increased a person’s risk of pancreatic cancer (P=0.02) [8]. However, the ORs for different duration categories were very similar: compared to participants without diabetes, ORs were 1.4 (95% CI: 0.7-2.4), 1.7 (95% CI: 1.0-2.9), and 1.5 (95% CI: 1.01-2.2), for 2-4, 5-9, and more than 10 years, respectively.
Our analyses did not reveal strong evidence for differences in cancer risk by diabetes treatment. In our case-control study, when compared to individuals without diabetes, the OR for diabetic individuals using insulin was 3.34 (95% CI: 1.35-8.26), whereas the OR was 1.50 (95% CI: 0.60-3.81) for diabetic individuals not using insulin. In the IWHS cohort, the risk of pancreatic cancer for women with diabetes who reported that they were ever-treated and never-treated, compared to those without diabetes, were both elevated: HR=1.87 (95% CI: 1.10-3.18) and HR=1.44 (95% CI: 0.64-3.25), respectively. Our results from the IWHS are not completely comparable to those from other studies since women who used either diabetes pills or insulin were combined into one treatment group in order to increase the power of the analysis. Yet, the overall effect is similar to the results from previous studies. In a pooled analysis of three large pancreatic case-control studies, Li et al. in 2011 found that participants with diabetes who used insulin compared to those with diabetes who did not use insulin had an OR=2.2 (95% CI: 1.6-3.0) [21]; findings from our Midwestern case-control study are in line with these results.
Both of the studies we present here have some limitations. BMI was not assessed in the pancreatic cancer case-control study as cases may have experienced rapid weight loss prior to diagnosis. Omission of questions on previous weight and height in the questionnaire was an oversight. Despite this, our findings were very similar to those from the IWHS that accounted for BMI. Of note, although BMI was selfreported in the IWHS, previous validation studies in the IWHS indicated that the self-reported measures of weight and height (used to calculate BMI) were reliable and accurate [22].
An additional limitation is self-report of diabetes. Various studies, including a recent study in elderly women, have found that self-reporting of diabetes is fairly accurate [23, 24, 25]. A small IWHS validation study of 44 self-reported diabetes cases at baseline suggested some over-reporting of diabetes since only 28 (63.6%) cases were confirmed by a physician [26]. This misclassification could result in bias towards the null. There is also the possibility of under diagnosis of diabetes. It is estimated that there are 7 million people in the United States who have diabetes, but have not been diagnosed [27]. Thus, in our studies, participants may be misclassified as not having diabetes. If either under- or over-reporting of diabetes diagnosis occurred, our results may be altered, with underreporting generally leading to attenuation of risk estimates. Finally, relatively low numbers of cases in some subgroup categories limited the power to look at differences by duration and treatment.
While both of these studies have limitations, they have important strengths. The IWHS is a large populationbased cohort with follow-up of 22 years. Through the use of SEER and the National Death Index (NDI), this study has excellent case ascertainment. Additionally, the prospective study allows for the inclusion of incident diabetes and pancreatic cancer cases. This is especially important for rapidly fatal diseases such as pancreatic cancer. Information is collected prior to pancreatic cancer diagnosis on virtually all subjects subsequently diagnosed, regardless of survival time. This is generally an advantage over case-control studies that may have selection bias by only including pancreatic cancer cases with relatively long survival. Of note, in our population-based case-control study the results were very similar to the cohort results, perhaps because we reduced the potential for selection bias by using rapid case ascertainment with subsequent confirmation of case eligibility by a pathologist who reviewed the medical reports.
Studies of diabetes and pancreatic cancer are challenging. Apart from diabetes that arises as a consequence of a pancreatic tumor, the relationship between the two conditions is ambiguous. Diabetes may increase surveillance for cancer, it may increase risk of cancer, or there may be an unidentified cause that is common to both diabetes and cancer [4, 7, 8, 9, 10, 21, 28, 29, 30, 31]. It is difficult to establish a temporal sequence when the precise onset of each condition is not clear, diabetes is under diagnosed in the population and individuals who are pre-diabetic may also be at risk of cancer [27]. In addition, onset of pancreatic cancer may precede clinical detection for up to 18 years [32]; it is possible that during carcinogenesis, but well in advance of detectable cancer, there is disruption of pancreatic function that leads to diabetes.
The results from the analyses presented here are consistent with the hypothesis that diabetes is associated with increased risk of subsequent pancreatic cancer and this increased risk is evident even when the diabetes precedes the diagnosis of cancer by 10 or more years. Whether a cause, consequence or correlate with common antecedent, diabetes could be useful as a component of risk models for cancer of the pancreas. Such models may help identify the cancer at a stage where intervention could improve survival.
The authors thank the staff of these studies for consultation and assistance in data analysis and to the participants in the research for their contributions
None were declared for all authors
Grants from the National Institutes of Health/National Cancer Institute supported these studies: The IWHS (R01 CA39742) and the Midwestern case-control study of pancreatic cancer (R01 CA58697)