- (2012) Volume 13, Issue 2
Vasco Eguia1, Tamas Adam Gonda1, Muhammad Wasif Saif2*
Divisions of 1Digestive and Liver Diseases and 2Hematology and Oncology, Columbia University Medical Center. New York, NY, USA
Despite treatment advances pancreatic cancer remains one of the most lethal malignancies. It is expected that early detection and screening of high risk patient population may have the most significant impact on altering overall survival in this disease. Serologic biomarkers may be the most useful in early detection and histology-based markers may have the most significant role in differentiating benign, pre-malignant and malignant lesions. Here we review several serum and tissue-based biomarkers and summarize new data presented at the 2012 ASCO Gastrointestinal Cancers Symposium (Abstracts #151, #164, #188) on the potential role of PAM4 in pancreatic cancer screening and diagnosis.
Antibodies, Neoplasm; Carcinoma, Pancreatic Ductal; Early Detection of Cancer
CA 19-9: carbohydrate antigen 19-9; CAM: cell adhesion molecule; CEACAM: carcinoembryonic antigen-related cell adhesion molecule; MIC-1: macrophage inhibitory cytokine; PanIN: pancreatic intraductal neoplasia; PLEC1: plectin 1; REG4: regenerating islet-derived family, member 4; TSGF, tumorspecific growth factor
The incidence of pancreatic cancer continues to increase every year, making this malignancy the fourth leading cause of cancer related death in the USA [1]. It carries a dismal survival rate of approximately 4% after 5 years [2]. The only potentially curative therapy today is successful surgical resection, which is achievable when the tumor is detected at an early stage. However, even among those patients who have surgically resectable disease at diagnosis, the 5-year survival rate is 15-40%, with the use of surgery and adjuvant chemotherapy, and/or radiation [3].
Unfortunately, pancreatic cancer will generally present with non-specific symptoms at a late stage, and this may be one of the important causes for the lack of improved survival despite treatment advances. It also emphasizes the need for screening strategies and ability to recognize early cancer or precursor lesions in individuals at highest risk. Currently, a combination of imaging modalities is utilized in an attempt to detect lesions in high-risk individuals. These imaging modalities include endoscopic retrograde cholangiopancreatography, endoscopic ultrasound, magnetic resonance imaging, magnetic resonance cholangiopancreatography, computed tomography, and even exploratory laparotomy with partial pancreatic resection in certain high risk groups [4, 5]. Additionally, the use of disease-specific molecular markers could provide a non-invasive and costeffective alternative to aid clinicians in the early detection of these aggressive tumors. Thus far, except for the carbohydrate antigen 19-9 (CA 19-9), most molecular markers have not been implemented to clinical practice. It has a median sensitivity ranging from 41 to 86% and a relatively poor specificity ranging from 33 to 100% [6]. CA 19-9 does not currently qualify as a screening biomarker in the asymptomatic population. It currently is utilized in patients who are symptomatic, and may aid in differentiating patients with pancreatitis from those with pancreatic carcinoma. However, the sensitivity of CA 19-9 is particularly low in patients with early stage cancer or pre-malignant lesions [6]. Newer markers are currently under investigation and preliminary data suggests that some of these could be utilized on their own, or in combination with current screening and diagnostic modalities, in an effort to improve our early tumor detection rate.
A biomarker is generally measured as an indicator of a biologic or pathogenic process. Such a marker should have an improved ability to detect early non-invasive lesions, which may be more amenable to curative therapy. Due to both its cost-efficacy and ease of use a serum (or stool DNA) based biomarker maybe the most desirable. Tissue based markers are important as this line of research can often lead to further testing in blood and these markers may be especially important in understanding the behavior of pre-malignant lesions or distinguishing chronic pancreatitis from neoplasia. Some of these biomarkers have shown superior specificity and sensitivity. A few promising studies and biomarkers are reviewed here with a particular emphasis on their ability to detect early cancer, premalignancy and distinguish inflammatory processes from neoplasia.
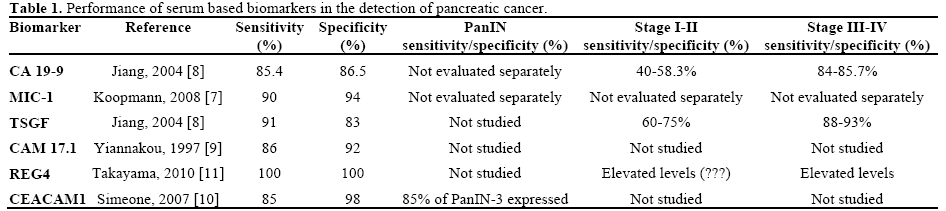
In Table 1 we summarize some of the results of serum based biomarkers. One of the serum biomarkers that has shown to have a high sensitivity and specificity is macrophage inhibitory cytokine (MIC-1) [7]. Koopmann et al. revealed MIC-1 to have 90% sensitivity and 94% specificity in a blind study comparing MIC-1 and CA 19-9 in patient cohorts with pancreatic carcinoma, chronic pancreatitis and healthy controls. The authors concluded that MIC-1 was both sensitive and specific for pancreatic cancer; furthermore, that in differentiating pancreatic cancer from controls, MIC-1 outperformed CA 19-9 [7]. Another serum based marker which has shown promising results is tumor-specific growth factor (TSGF) [8]. Jiang et al. tested TSGF showing this marker to have 91% sensitivity and 83% specificity. Interestingly there was a significant difference in serum levels based on the location of the cancer in the pancreas (head of pancreas lesions had a much higher level than tail or body lesions). The authors also evaluated TSGF in terms of pancreatic cancer stage. The sensitivity gradually increased with stage, where TSGF had a sensitivity of 60% for stage I cancer [8]. Another promising biomarker is an anti-mucin antibody, cell adhesion molecule 17.1 (CAM 17.1), which was examined by Yiannakou et al. [9]. In this study this marker was found to have a sensitivity of 86% and a specificity of 92%; however, no correlation was found between tumor size and the results of the CAM 17.1 assay [9]. Furthermore, Simeone et al. studied carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1), achieving a sensitivity of 85% and a specificity of 98%, when comparing cancer to controls [10]. Also, when considering pancreatic intraductal neoplasia (PanIN), the authors found CEACAM1 to be expressed by 85% of the PanIN-3 lesions [10]. Also, a study by Takayama et al., evaluated the usefulness of another marker, named regenerating islet-derived family, member 4 (REG4) [11]. The study revealed the sensitivity, specificity and accuracy of REG4 to be 94.9%, 64% and 77.5%, respectively, when compared to healthy controls. The authors also stratified REG4 levels by cancer stage, and saw that REG4 levels were markedly elevated even in patients with stage I and II cancer, when compared to healthy controls. REG4 also performed better than serum CA 19-9 for differentiating patients with pancreatic cancer from healthy individuals [11]. Therefore, according to these findings, REG4 has the potential to be a useful indicator of early pancreatic cancer, and to help distinguish patients with pancreatic cancer and healthy individuals. These data are represented in Table 1.
Similarly to serum biomarkers, tissue based markers have also been thoroughly studied. A highly sensitive and specific tissue biomarker would be very useful in differentiating cancerous tissue from chronic pancreatitis and/or normal pancreatic tissue. However, many of the studied tissue biomarkers have proven to lack enough sensitivity and specificity in order to become clinically useful. A promising tissue biomarker for pancreatic cancer is human trophoblast cell-surface antigen TROP2. This biomarker is strongly expressed by a variety of human epithelial cancers, and correlates with aggressiveness and poor prognosis [12, 13]. In a study by Fong et al., TROP2 was found to be overexpressed by 55% of pancreatic cancer patients and was also significantly associated with a decreased survival [14]. In addition in the same study the overexpression of TROP2 was shown to be correlated with a poor post-operative progression-free survival, and was found to be an independent prognosticator in pancreatic cancer [14]. These findings are particularly important because TROP2 could be utilized both as a prognostic marker and to tailor treatment. Additionally, plectin 1 (PLEC1) is another novel tissue biomarker for pancreatic cancer. In a study by Bausch et al., PLEC1 was found to be expressed by human pancreatic ductal adenocarcinoma, but negative in benign tissues (e.g., chronic pancreatitis and normal pancreatic tissue) [15]. It was found to be misexpressed in 60% on PanIN III lesions, as well as in metastatic foci. Therefore, PLEC1 has been shown to be a potential identifier of preinvasive PanIN III lesions, which would certainly be useful in the effort of diagnosing early pancreatic cancer. Finally PAM4 is another biomarker with great potential in the detection of early pancreatic cancer [16].
PAM4 is a monoclonal antibody, IgG1 immunoglobulin, which is produced from immunizations of mice with mucin purified from xenografted RIP1 human pancreatic carcinoma. In immunohistochemical studies, PAM4 has shown to be reactive with a biomarker expressed by 87% of pancreatic malignancies, including early stage I disease (PanIN), and generally non-reactive with pancreatitis specimens [17, 18]. Its sensitivity to detect pancreatic adenocarcinoma has been shown to be 82%, with a false positive rate of 5%. These results imply that such a molecular marker could be utilized effectively not only as an adjunctive tool in the diagnosis of pancreatic cancer, but also as a screening tool to detect early stage disease. Also, immunohistochemical findings suggest the PAM4 antigen is not produced by normal or inflamed pancreatic tissue [16]. Abstracts reviewed below and presented at the 2012 ASCO Gastrointestinal Cancers Symposium present important data about the utility of this biomarker in the early detection of cancer and its ability to differentiate inflammation from neoplasia.
Detection of Early-Stage Pancreatic Adenocarcinoma: Sensitivity, Specificity, and Discriminatory Properties of the Serum-Based PAM4-Immunoassay. (Abstract #151 [19])
This study evaluated a serum-based enzyme immunoassay to detect PAM4 antibody. Serum from both malignant and benign disease of the pancreas and surrounding tissues were utilized. It revealed an overall sensitivity for detection of pancreatic ductal adenocarcinoma to be 76%, with a sensitivity of 64% in stage I patients and a higher sensitivity of 85% for advanced disease. For the most part, sera from patients with neuroendocrine tumors of the pancreas or cancers of other origin (squamous, GIST, etc.) did not have elevated levels of the PAM4 antigen. Approximately half of the patients with ampullary (48%) and extrahepatic biliary (50%) adenocarcinomas had positive levels of circulating PAM4 antigen. Of 126 patients diagnosed with benign conditions of the pancreas, only 24 (19%) were positive and, in particular, 18 of 80 (23%) patients with chronic pancreatitis were positive. Also, when considering patients with benign pancreatic disease and chronic pancreatitis, PAM4 was positive in 19% and 24% of patients, respectively. The positive and negative likelihood ratios for differentiating pancreatic ductal adenocarcinoma from benign conditions of the pancreas were 4.00 and 0.30, respectively. The PAM4 immunoassay detects nearly two-thirds of stage I pancreatic ductal adenocarcinoma patients, and does so with high discriminatory power with respect to benign pancreatic disease. These results provide a rationale for longitudinal surveillance of patients considered at highrisk for pancreatic ductal adenocarcinoma (e.g., familial pancreatic cancer, new-onset diabetes, etc.) with the PAM4 assay.
Combination of the PAM4 and CA 19-9 Biomarkers to Improve the Detection of Pancreatic Adenocarcinoma (Abstract #164 [20])
Another study which compared PAM4 and CA 19-9 in patients with confirmed pancreatic carcinoma, other cancers, benign disease of the pancreas and healthy adults. The results revealed that the sensitivity for detecting pancreatic ductal adenocarcinoma, including early-stage disease, was statistically similar for both immunoassays (e.g., PAM4 and CA 19-9). However, specificity was significantly lower for CA 19-9, particularly with respect to chronic pancreatitis, 68% vs. 86% for the PAM4 assay (P=0.014). Finally, a combined biomarker analysis was shown to improve the overall pancreatic ductal adenocarcinoma detection rate (84%), without a significant decrease in specificity (83%). These results reveal that not only PAM4 provides a high sensitivity and specificity in the detection and diagnosis of pancreatic cancer but also the addition of CA 19-9 provides enhanced positive identification of pancreatic cancer.
Use of the Monoclonal Antibody PAM4 to Differentiate Pancreatic Ductal Adenocarcinoma (PDAC) from Chronic Pancreatitis and Benign Nonmucinous Cysts of the Pancreas. (Abstract #188 [21])
A different study evaluated tissue microarrays of chronic pancreatitis, pancreatic ductal adenocarcinoma and benign non-mucinous cystic lesions of pancreas tissue with immunohistochemical assay for expression of PAM4 reactive mucin, and compared it to that of MUC1 (mAb-MA5), MUC4 (mAb-8G7) and CEACAM6 (mAb-MN-15). PAM4-reactive mucin, MUC1, MUC4 and CEACAM6 were expressed in 79% (11/14), 100% (14/14), 86% (12/14) and 100% (14/14) of invasive pancreatic adenocarcinoma. PAM4 only weakly labeled 1 out of 19 benign non-mucinous cystic lesions, 1 of 15 serous cystadenomas and 0 of 4 cysts with squamous epithelial lining (2 lymphoepithelial cysts, and 2 retention cysts with squamous metaplasia). However, the expression of MUC1, MUC4 and CEACAM6 was detected in 53% (8/15), 0% (0/15) and 13% (2/15) of serous cystadenomas. MUC1 was detected also in all 4 cysts, and MUC4 and CEACAM6 was detected in 3 of the 4 cysts (75%). PAM4 labeled 19% (6/32) of chronic pancreatitis specimens; however, this PAM4 reactivity was restricted to the PanIN precursor lesions associated with chronic pancreatitis. Inflamed tissue was negative. The expression of MUC1, MUC4 and CEACAM6 was detected in 90% (27/30), 78% (25/32), and 97% (31/32) of chronic pancreatitis. In all of the positively-labeled specimens, the reactivity was present in non-neoplastic inflamed pancreatic tissue in addition to PanIN. The expression of PAM4 was detected in only 6% of benign non-mucinous cystic lesions and in the precursor lesions associated with chronic pancreatitis. Whereas, the other markers studied were expressed in 78-97% of chronic pancreatitis specimens. These results suggest that PAM4, in contrast to MUC1, MUC4, and CEACAM6, may be useful to differentiate benign non-mucinous cystic lesions of the pancreas and chronic pancreatitis from pancreatic ductal adenocarcinoma or PanIN lesions.
Overall these studies further suggest a need to evaluate the use of serum PAM4 levels combined with CA 19-9 testing in both serum based screening and immunohistochemical differentiation of neoplastic and benign lesions.
The authors declare no conflicts of interest