Keywords
Monoamniotic twin pregnancy; Single-twin intrauterine demise; Twin-to- twin transfusion syndrome
Introduction
Monoamniotic twin pregnancies are the least common type of twin pregnancy, with overall incidence of 1─5% of all monozygotic twin gestations [1,2]. It has high rates of complications including cord entanglement and foetal demised among others. Although the condition is rare, few studies have reported about the management approach of early second-trimester single-twin intrauterine foetal demise in monoamniotic twin pregnancy. In resource-limited settings, speculation regarding risk of maternal complications (systemic infection and coagulopathy) from the demised-foetus has encouraged termination of pregnancy in women with single-twin intrauterine foetal demise. Additionally, there is also gap in terms of systematic screening of potentially fatal complications associated with monochorionic twin pregnancies. This study describes twin-to-twin transfusion syndrome and management approach of single-twin intrauterine demise in monoamniotic twin pregnancy.
Case Report
A 22-year-old primigravida, presented at antenatal clinic with complaints of vaginal bleeding and low abdominal pain at 13 weeks of gestation by her last menstrual period (LMP). It was her first antenatal clinic visit. The past medical and surgical history was unremarkable. The patient was generally stable. The abdominal showed a gravid uterus with fundal height of 14 cm. The cervix was closed on speculum exam.
Ultrasonography done showed features of 2 viable foetuses, monoamniotic at 14 weeks without structural anomalies. There was no documented information regarding abnormalities on the sharing placenta. Two weeks later, the patient came-back with similar symptoms and was admitted. A repeat ultrasound reported monochorionic monoamniotic twin pregnancy with single-twin intrauterine demise at 16 weeks. The surviving twin had no abnormalities, with foetal heart rates of 157 beat per minute. The time at what ultrasonography diagnosed single-twine foetal demise was recorded as time of foetal death. Laboratory investigations done including coagulation profile, complete blood count (CBC) were unremarkable.
From the date of the diagnosis of single-twin intrauterine demise, the patient was informed, and about further management plan consisted of carry pregnancy up to 34 weeks gestation under follow up. She was counselled with regard to difficult emotional experience of losing one foetus and carrying both dead and alive foetuses. With regard to foetal surveillance, the serial ultrasound was indicated fortnight’s time up to 34th week of gestation. Each scan requested to report about amniotic fluid volume, foetal bladder, biometry, estimated foetal weight, assessment of intracranial anatomy, umbilical artery flow Doppler after 20 weeks gestation and cardiotocogram after 28 weeks. Maternal surveillance included serial complete blood count (CBC) and coagulation profile, blood pressure, vaginal bleeding or discharge. Termination of pregnancy before 34 weeks of gestation was indicated only if preeclampsia/ eclampsia, surviving co-twin intrauterine demise, preterm premature rupture of membranes with severe oligohydramnios, and abnormal umbilical artery Doppler (increase resistive index, absent or reversed end diastolic flow) or intrauterine growth restriction.
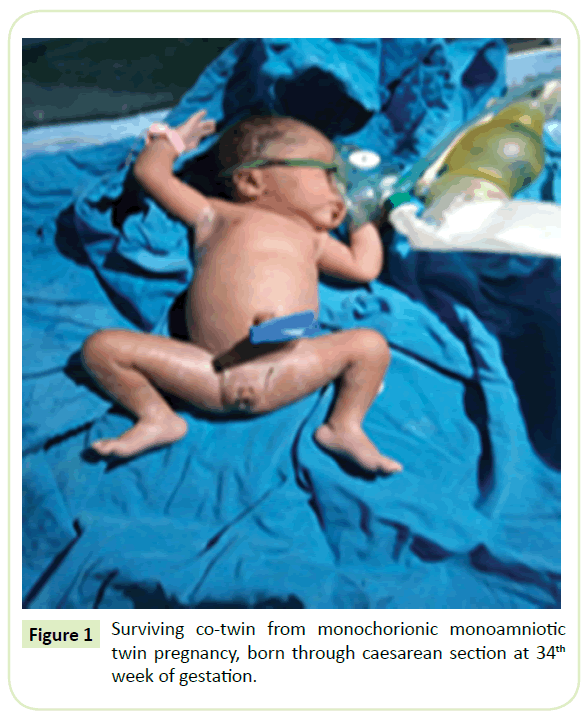
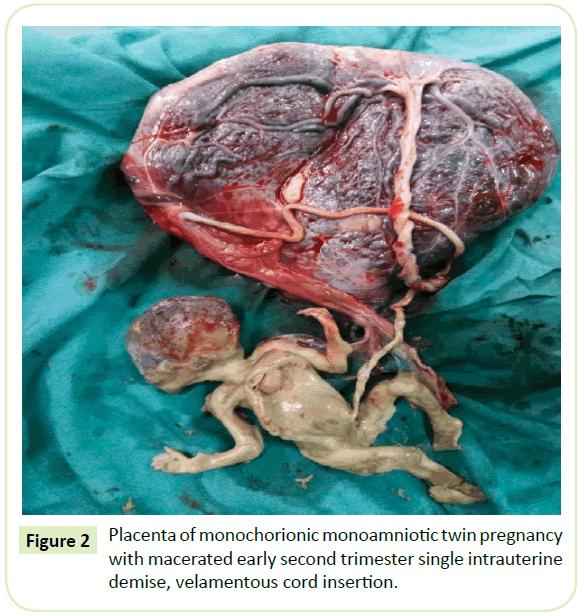
At 28th week of gestation, patient was readmitted for vaginal discharge, querying preterm premature rupture of membranes. A repeat ultrasound showed amniotic fluid index of 18 cm. Coagulation profile and full haemogram were reported to be normal. Indirect coombs test was negative. The patient was given anti-D 300 μg at 28th week of gestation based on her rhesus blood group O negative. She was also treated with Nitrofurantoin 100 mg twice for 7 days for urinary tract infection. The caesarean section was successfully performed at 34th week of gestation. Alive female infant weighted 1800grams was born, with Apgar score of 8 at 1 and 5- minutes. The new-born developed respiratory distress and was admitted at new-born unit. The full haemogram of surviving co-twin was within normal range. The demised foetus was female, weighted 200grams, macerated without congenital anomalies according to the autopsy result; however, with features of a large heart. Macroscopically, the placenta showed velamentous insertion of the 2 umbilical cords and superficial arterio-arterial vascular anastomoses. These findings were consistent for acute twin-to-twin transfusion syndrome, adding the gestation age of single-twin foetal event and growth restriction to the surviving co-twin. Follow up was scheduled at 2nd and 6th weeks post-delivery, then after 1 year to assess infant neurological impairment.
Discussion
Monoamniotic twin pregnancies are the least common type of twin pregnancy; however, with higher intrauterine foetal demise rates than diamniotic twin pregnancy [2]. Despite the high rates of perinatal death in monoamniotic twin pregnancies, there is paucity of data regarding the incidence of cause of foetal deaths in this category. Although, perinatal death has been attributed frequently to umbilical cord entanglement, twin-to-twin transfusion syndrome (TTTS), discordant foetal growth abnormality [2]. To date, studies are in agreement that placental angio-architecture has in important role to play in pathogenesis of events. This [angioarchitecture] consists of individual placental territory size, cord insertion location, and direction of inter-twin vascular anastomoses [3]. In monochorionic diamniotic twins, vascular anastomoses are arterio-venous (AV), unidirectional and are referred to be "deep" since they proceed through a shared placental cotyledon [4]. Evidence shows that such kind of anastomosis predisposes to TTTS, selective foetal growth restricted (sFGR), and twin anaemia polycythaemia sequence (TAPS) [5]. In contrast, in monoamniotic twins’ placenta vascular anastomoses are large, numerous, superficial and arterial to arterial (AA) or venous to venous (VV) with a short distance between the cords, and bi-directional [5]. This type of anastomosis protects against the development of chronic TTTS and TAPS by compensating for the circulatory imbalance caused by the uni-directional AV anastomoses [5]. In addition, The TTTS, which accounts 10-15%, predominantly occurs from 16th week of gestation to prior 26 weeks; whereas TAPS is predominantly found after 26 weeks [4]. The single-twin intrauterine demise occurs when there is a drop-in blood pressure from the donor to the recipient twin [6]. If the drop of blood pressure is acute and serious, studies have reported up to 15% of deaths of survivor co-twin soon after [6,7]. If the drop is acute and less serious, the survivor may sustain ischemic injury in about 26% of the cases [6,7]. If the drop-in blood pressure is subtle, the survivor will be intact [6]. Authors in the current study though that this should be the scenario in this case.
The diagnosis criteria of TTTS seems exclusively applied on monochorionic diamniotic pregnancies. These [criteria] include oligohydramnios in donor sac with deep vertical pocket (DVP) of ≤ 2 cm or polyhydramnios in recipient sac with DVP ≥ 6 cm; sFGR (≥ 25%); and abnormal umbilical artery Doppler study (increased resistive index, absent or reverse end diastolic flow, abnormal middle cerebral artery or ductus venosus) in the smaller twin; and distended bladder with/without abnormal foetal Dopplers with/without tricuspid regurgitation or cardiomegaly and with a DVP of 6–8 cm in the larger twin depending on the gestational age [8]. To date, these findings have helped to stage the severity of TTTS, known as Quintero’s stage of the disease.
Stage I: Bladder of donor twin still visible;
Stage II: ANURIA of donor twin;
Stage III: Critically abnormal Doppler studies;
Stage IV: Hydrops;
Stage V: Demise of one or both twins [2].
The specific strategies of management of TTTS depend upon the stage of the disease and chorionicity.
There are several ways to manage TTTS, including specific strategies (selective foetoscopic laser coagulation of placental anastomoses, SFLP) and non-specific strategies such as expectant management, amnioreduction, septostomy and selective reduction [2]. The success of one or the other strategy depends on timely diagnosis and obstetrical surveillance. The screening associated with early detection and management have contributed to reduced perinatal mortality among affected pregnancies. To date, most studies are in agreement that screening for risk of TTTS starts at 16 weeks. However, an abnormal nuchal translucency and crown-rump length) recorded in the first trimester (10-13 weeks) is also accurate to predict severe TTTS later in pregnancy [7]. In this case, ultrasound was done in second trimester (at first antenatal care clinic). This is not surprising because most women in developing areas present to antenatal clinic when they are sick. In addition, the routine screening of monochorionic related complications at 16th week should not be achieved because single-twin intrauterine event approximately occurred at that period. Regarding the specific strategies of management of TTTS, SFLP is a preferred option because it has shown better outcomes compared to serial amnioreduction or non-specific strategies [7].
Unfortunately, in most resource-limited settings [if not all], this technology [SFLP] is out of reach of many of affected pregnancies. The most accessible strategy in resource-limited settings is expectant management. Moreover, the Society for Maternal-Foetal Medicine for management of TTTS in monochorionic diamniotic still suggests to consider expectant management in stage II, III and IV disease [2]. In monoamniotic twins with TTTS or single-twin intrauterine demise, the authors of current study recommend expectant management under maternal and surviving co-twin surveillance. This works only, in absence of comorbidities such as pre-eclampsia or eclampsia and absence of abnormal umbilical artery Doppler study of the surviving co-twin. We discourage termination of pregnancy based on speculation of risk of maternal systemic infection and coagulopathy. Evidence has shown that maternal infection and coagulopathy are uncommon in single-twin intrauterine demise. It is [coagulopathy] about null when single-twin foetal demise occurs within fi rst [vanishing twin syndrome] or second trimester [foetal papyraceous] [9]. This is because the dead foetus or fluid of the dead tissue is gradually absorbed [9,10]. Moreover, one study recently found no relationship between observed coagulopathy and high grade macerated intrauterine demise in affected women in absence of comorbidity such as hypertensive disorders or predisposed risk factors such as anticoagulation treatment or genetic factors [11]. Although, coagulation profile is recommended at fortnightly intervals [9].
In addition, maternal psychological effect of carrying both a dead and surviving foetuses was a major concern. However, psychosocial support was carried out up to delivery. Regarding mode and time of delivery, evidence supports elective caesarean birth as the preferred mode of delivery at 32–34 weeks of gestation for monoamniotic twins to prevent intrapartum cord complications [12] . In postpartum period, full haemogram of new-born is routinely recommended to rule out anaemia of new-born [7]. Furthermore, neurological assessment of infant is important because TTTS is associated with neurological complications such as intraventricular haemorrhage, periventricular leukomalacia, cerebral white matter cysts, ventricular dilatation, and cerebral atrophy [7]. The long-term neurodevelopmental complications vary between 3 and 12% for cerebral palsy and 4 and 18% for neurodevelopmental impairment [7]. In this case, the infant is 1-year-old with no neuro-development impairment. Probably the subtle nature of the event left the survivor intact as demonstrated by previous studies. However, evidence has shown that neurological complications are mostly observed in the neonatal period following laser procedures [7]. The risk factors include advanced gestational age at laser surgery (≥ 26 weeks), low gestational age at birth, low birthweight, and high Quintero stage [7] (Figures 1 and 2).
Figure 1: Surviving co-twin from monochorionic monoamniotic twin pregnancy, born through caesarean section at 34th week of gestation.
Figure 2: Placenta of monochorionic monoamniotic twin pregnancy with macerated early second trimester single intrauterine demise, velamentous cord insertion.
Conclusion
Twin-to-twin transfusion syndrome is uncommon complication in monoamniotic twin pregnancies. If single-twin intrauterine demise occurs, expectant management under maternal and surviving co-twin surveillance is recommended. This works only, in case of absence of comorbidities such as pre-eclampsia or eclampsia and absence of abnormal umbilical artery Doppler study of the surviving co-twin. Single-twin foetal demise does not increase the risk of systemic infection and coagulopathy. However, maternal psychological impact is a concern. A planned caesarean delivery at 32-34 weeks is a gold standard of obstetric care in monoamniotic twin pregnancy.
Ethics Approval and Consent to Participate
We obtained a formal approval from Moi University-Moi Teaching and Referral Hospital Institutional Research and Ethics Committee (IREC).
Consent to Publish
A written informed consent for publication was sought from the patient and IREC.
Availability of Data and Materials
We used our own materials and data.
Competing Interests
The authors declare that they have no competing interests
Funding
The study was entirely supported by our own financial contributions.
Acknowledgements
We acknowledge all contributors, the team who participated on the management of the patient, and the patient for her collaboration and informed consent of publishing information related to her condition.
References
- DeCarolis MP, Salvi S, Bersani P, Corsello M, De Carolis S (2017) Single-twin demise in monochorionic pregnancy: Looking beyond the placental inter-twin anastomoses. Ann Clin Case Rep 2: 1312.
- Julio E, Eduardo FMS, Gustavo NC (2015) Monochorionic twin pregnancy-Potential risks and perinatal outcomes.
- Toneto BR (2018) Complications in monochorionic pregnancies. IntechOpen 2: 1.
- Enrico L, Femke S, Johanna M, Middeldorp, Frans JK, et al. (2011) Accurate and simple evaluation of vascular anastomoses in monochorionic placenta using colored dye. J Vis Exp. e3208.
- Fitzgerald B (2018) Histopathological examination of the placenta in twin pregnancies. APMIS 126: 626-637.
- Blickstein P (2017) Single fetal demise in monochorionic twins. Harefuah. 156: 377-379.
- Gratacos E, Ortiz JU, Martinez JM (2012) A systematic approach to the differential diagnosis and management of the complications of Monochorionic twin pregnancies. Foetal Diagn Ther 32: 145-155.
- Khalil A (2017) Modified diagnostic criteria for twin-to-twin transfusion syndrome prior to 18 weeks’ gestation: time to change? Ultrasound Obstet Gynecol 49: 803-808.
- Jain D, Purohit RC (2014) Review of twin pregnancies with single fetal death: Management, maternal and fetal outcome. J Obs Gyn Ind 64: 180-183.
- Bozkurt M, Kara D (2013) Foetus papyraceous in a twin pregnancy: A case report without any maternal and foetal complications. Proc Obstet Gynecol 3: 4.
- Muin DA, Haslacher H, Koller V (2018) Impact of fetal maceration grade on risk of maternal disseminated intravascular coagulation after intrauterine fetal death – A retrospective cohort study. Scientific Reports p. 8.
- Dias T, Thilaganathan B, Bhide A (2012) Monoamniotic twin pregnancy. The Obstetrician & Gynaecologist 14: 71–78.