Review Article - (2018) Volume 2, Issue 3
Boquete-Castro A* and Lucero-Sánchez AF
Faculty of Health Sciences, Universidad Católica San Antonio de Murcia, Spain
*Corresponding Author:
Ana Boquete-Castro
Coordinator of Cathedra of Investigation in Clinical Dentistry
Faculty of Health Sciences
Universidad Católica San Antonio de Murcia
Mucia, Spain
Tel: +34950625772
E-mail: ana.boquete@odontologiaucam.es
Received Date: September 22, 2018; Accepted Date: September 29, 2018; Published Date: September 30, 2018
Citation: Boquete-Castro A, Lucero-Sánchez AF (2018) Effect of Low Level Laser Application in Temporomandibular Disorders: An Updated Literature Review. J Ora Med Vol.2 No.3:8
Background: Temporomandibular dysfunction (TMD), which is considered the main cause of non-dental orofacial pain. Therefore, treatment must be focused on the reduction of symptoms. In this sense, low intensity laser therapy is suggested to have bio stimulating and analgesic effects. Methods: A Cochrane and Medline databases search were conducted between June and December of 2017. The terms used for the different searches were “temporomandibular joint”, “laser therapy”, disorders, laser and treatment. Findings: 6 publications were selected from a total of 162. They were stratified using the SORT criteria (Strength of Recommendation Taxonomy). Conclusion: TMD is a complex disorder that can be challenging to diagnose and treat. The efficacy of laser in the treatment of TMD is rather promising. According to the literature reviewed, low level laser seems to have a benefit on patients with TMD, however, it is still difficult to establish a therapeutic protocol for TMD.
Keywords
Temporomandibular joint; Laser therapy; Disorders; Laser and treatment
Abbreviations
TMD: Temporomandibular Dysfunction; VAS: Visual Analogue Score
Background
Temporomandibular dysfunction (TMD) is considered the main cause of non-dental orofacial pain [1-3]. TMD involves problems in the masticatory musculature, the temporomandibular joint and orofacial structures. Pain is the most common consequence but earache and headache can be also present [4,5]. In the great majority of cases it occurs from a convergence of multiple factors such as: inflammatory diseases, degeneration of articular cartilage, dislocation of the articular disc and overloading of the joint due to missing teeth, inadequate prostheses, etc. [6,7].
Many aspects of TMD are still unclear; that is the reason why the main aim of their treatment is to decrease pain and improve function [8,9]. Therefore, treatment should be conservative and must be focused on the reduction of symptoms [10,11].
According to that, light amplification by stimulated emission of radiation (laser) is one of the most recent treatment modalities. Low intensity laser therapy is suggested to have biostimulating and analgesic effects through direct irradiation [1,4,10-13]. The effect on muscular pain caused by the application of a therapeutic laser showed better results with laser therapy than with electrotherapy, according to Medlicott and Harris [14]. In this sense, Kulekcioglu et al. [15] had similar results, using only non-invasive laser therapy as an alternative form of treatment.
Different authors have reported good results in the treatment of temporomandibular joint with laser. Pinheiro et al. [16] concluded that the function of temporomandibular disorders achieved better results after application of the laser. Moreover, the fact of being a non-invasive technique and its low cost makes it more attractive to patients than other treatment possibilities [3].
The purpose of this systematic review was to analyze the use of laser in the treatment of temporomandibular disorders regarding results in pain´s relief in order to establish a protocol to apply on the daily dental practice.
Methods
A Cochrane and Medline databases search of articles was conducted between June and December of 2017. The key words used were: “temporomandibular joint”, disorders, laser, “laser therapy”, treatment. Moreover, those terms were combined using the Boolean operator “AND” in order to obtain articles that included two or more of the search terms.
The inclusion criteria were studies carried out in humans and published in the last 10 years in English. Exclusion criteria were studies published before 2007, non-human studies, language different from English and the treatment of less than 5 patients.
Quality assessment
The quality of the studies was assessed focusing on: bibliography, blindness of examiners, characteristics of study population and outcome evaluations.
The selection of the articles was agreed between two of the authors, after screening of the abstracts to identify those relevant articles that fulfilled the inclusion criteria established.
Results
Out of the 162 articles found in the initial electronic search, the complete text of 17 articles was deeply analyzed. Ten of these articles were excluded due to the lack of direct relationship with the subject, and another one was excluded because it was a study carried out in healthy patients (Figure 1).
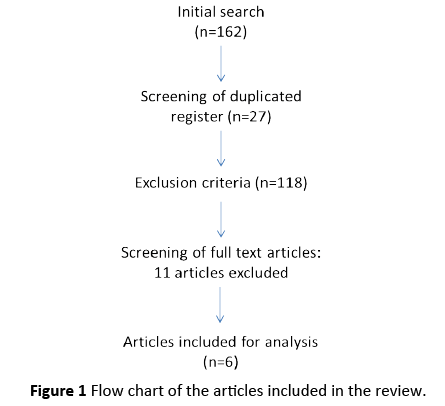
Figure 1: Flow chart of the articles included in the review.
Characteristics of included studies
Finally six articles were included in this systematic review: 3 randomized double-blinded clinical trials, 2 case series and 1 case-control study.
The articles were stratified according to their level of evidence using the SORT criteria (Tables 1 and 2). All articles had a scientific level evidence of 2.
Table 1 Strength-of-Recommendation Taxonomy (SORT): *Patient-oriented evidence measures outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction, and quality of life. **Disease-oriented evidence measures immediate, physiological surrogate end points that may or may not reflect improvements in patient outcomes (e.g. blood pressure).
| Code | Definition |
|---|---|
| A | Good-quality Patient-oriented evidence (*) |
| B | Inconsistent or limited quality patient-oriented evidence (**) |
| C | Consensus, disease-oriented evidence (*) |
Table 2 Level of scientific evidence Strength-of-Recommendation Taxonomy (SORT).
| Type of study | |||
|---|---|---|---|
| Diagnosis | Treatment/Prevention/ Screening | Prognosis | |
| Study Quality | |||
| A (Good evidence) |
-SR/meta-analysis of high quality studies. -High quality diagnostic cohort study. |
-SR/meta-analysis of RCTs with consistent findings. -High quality RCTs. |
-SR/meta-analysis of good quality cohort studies -Prospective cohort studies with good follow-up. |
| B (Limited evidence) |
-SR/meta-analysis of lower quality studies or studies with inconsistent findings -Lower quality diagnostic cohort study or diagnostic case-control study. |
-SR/meta-analysis of lower quality clinical trials or of studies with inconsistent findings -Lower quality clinical trial+ -Cohort study -Case-control study |
-SR/meta-analysis of lower quality cohort studies or inconsistent results. -Retrospective cohort study or prospective cohort study with poor follow-up period. -Case-control study -Case series |
| C (Other evidence) |
Consensus guidelines, opinion, disease-oriented evidence, case series. | ||
The studies included in this revision analyzed the effect of low intensity laser on:
- Pain of the temporomandibular joint: Visual Analogue Score (VAS) was used in all studies to measure the level of pain. It consists of a 10 cm straight line on which the patients marked their pain intensity, where 0 corresponds to no pain and 10 to the worst unimaginable pain.
- Mouth opening: to assess improvement of mouth opening, the distance between the edge of the lower and upper incisor was measured in millimeters.
Results of individual studies
Comparison of the findings of the selected studies is difficult due to the heterogeneity of the data, the intensity of the lasers applied, and the time of application. Therefore, it was decided to report individually the intervention of each study.
Results of the articles included are summarized in chronological order in Table 3. A more extensive explanation of each one is as follows:
Table 3 Summary of the articles finally included in this systematic review (* Statistical differences p<0.05).
| Author | Year | Level of evidence | Type of study | Number of patients | Laser device | Power of laser | Duration | Mean pain (VAS) before and after laser application | Mean mouth opening before and after laser application |
|---|---|---|---|---|---|---|---|---|---|
| Carrasco et al. | 2017 | 2 | Double-blinded | 14 | GaA1As Twin Laser | 70mW | Twice a Week, 4 Weeks | Not reported | Not reported |
| Navratil et al. | 2014 | 2 | Case series | 24 | BTL 4100 | 200mW | 10 sessions at an interval of 14 days | Pain persists only in 1 patient* | Before: 34 mm |
| After: 41, 96 mm* | |||||||||
| De Carli et al. | 2013 | 2 | Double-blinded randomised clinical trial | 32 | GaA1As Diode Laser | 100mW | Twice a week, 10 days | Before: 3,6 | Before:49, 36 mm |
| After: 0,42* | After: 47, 7 mm | ||||||||
| Marini et al. | 2010 | 2 | Double-blinded | 99 | Lumix 2 HFPL | 400mW | 10 days | Before: 7,72 | Before: 36,28 mm |
| After: 0,24* | After: 43, 24 mm* | ||||||||
| Hotta et al. | 2010 | 2 | Case-control | 10 | GaA1As Diode Laser | 70mW | Once a week, 10 weeks | Before: 5,5 | Before: 33 mm |
| After: 3,1* | After: 36 mm | ||||||||
| Yoshida et al. | 2007 | 2 | Case series | 55 | Ho:YAG | Not reported | Not reported | Before: 6,3 | Before: 26 mm |
| After: 1,6 | After: 41, 2 mm |
Carrasco et al. [4] carried out a double-blind study in which 14 patients were treated. Patients were randomly divided in two groups: placebo and active. A continuous laser beam of 70 mw was applied in active group for 60 seconds, twice a week, during 4 weeks. Pain level was valuated using VAS before the treatment, immediately after the treatment, and 30 days after the last application. Authors obtained a significant pain relief after the application of low-intensity laser therapy.
Navratil et al. [7] treated 24 patients with 200 Mw diode laser, combined with physiotherapy and individual exercises. The average duration of the treatment was 123 days. Authors did not report any complication during the therapy. Moreover, they obtained statistically significant analgesic effects after the treatment and a significant improvement in ability to open mouth was found after laser treatment (p<0.0001).
In the study of De Carli et al. [6] a total of 32 patients were treated in 3 groups: laser, piroxicam, laser+piroxicam. Laser was applied during 28 seconds with a power of 100 Mw. This is the only article that reported a significant worsening of pain values after 30 days of the treatment. Moreover, authors did not find statistical differences in mouth opening measurements before and after the treatment in the different groups.
Marini et al. [3] measured VAS scores and mouth opening before and after treatment with gallium-arsenide diode super pulsed laser, with a mean power of 400 mw, in a total of 39 patients. Results of this treatment were compared to 30 patients treated with anti-inflammatory drugs and 30 patients with no treatment. Authors obtained statistically significant differences (p=0.0001) for laser group in relation to values of mouth opening before and after the treatment.
Hotta et al. [17] applied laser with 70 mW power in 10 patients, once a week, during 10 weeks. Authors concluded that statistical significant improvement was obtained in relation to pain. Mandibular movements were also increased after the treatment, however, in this aspect, the differences before and after the treatment were no statistically significant.
Yoshida et al. [18] analyzed the effect of laser combined with arthroscopy in 55 patients. After the treatment, patients had reduced their pain scores. Moreover, an improvement of maximum interincisal measurement was obtained in all cases. Only 3 patients did not get better after treatment; authors concluded that was due to the fact that they were severe cases with perforated discs.
Discussion
TMD is a complex disorder that can be challenging to diagnose and treat. According to the literature reviewed, low level laser seems to have a benefit on patients with TMD, due to its analgesic properties, anti-inflammatory effect and biostimulation of the tissues.
Pain of the temporomandibular joint
VAS values before and after low level laser application were significantly reduced in 4 of the 8 studies, thus increasing life quality of patients after the treatment [6,17,18]. Of the 325 patients treated, only 1 of them did not diminished the level of pain at the temporomandibular joint after the low-level laser therapy [18,19].
Carrasco et al. [4] concluded that painful symptoms are always reduced after the application of low-level laser in comparison to those who received placebo. However, De Carli et al. [6] reported a worsening in pain levels after 30 days of the laser application. Authors assessed that it could be due to the elevation of temperature in the area.
Mouth opening
All studies reported an improvement of the mouth opening, but only 2 of them obtained statistically significant differences between groups.
Conclusion
The efficacy of low-level laser in the treatment of TMD is rather promising. However, due to the variability of types, frequencies, and duration of laser radiation in the studies analyzed, it is difficult to establish a therapeutic protocol.
Conflicting Interests
The authors declare they have no conflict of interests.