Original Article - (2017) Volume 18, Issue 2
1Department of Medicine, Albany Stratton VA Medical Center, USA
2Department of Gastroenterology, SUNY Downstate Medical Center, USA
3Department of Gastroenterology, Columbia University Medical Center, USA
4Department of Infectious Disease, Memorial Sloan-Kettering Cancer Center, USA
5Department of Gastroenterology, New York University Langone Medical Center, USA
Received November 13th, 2016 - Accepted January 07th, 2017
Background Endotherapy is a treatment modality that can be used to manage the pain associated with chronic pancreatitis. The aim of this systematic review and meta-analysis is to evaluate the efficacy of endotherapy in the management of pain associated with chronic pancreatitis. Methods A search of Medline, Pubmed, and Embase databases between 1988 to December 2014 was conducted to evaluate the use of endotherapy for pain relief in patients with chronic pancreatitis. We included large prospective studies, randomized controlled trials and retrospective analyses. Exclusion criteria included studies not written in the English language, small studies with less than 10 patients, case series/case reports and studies that enrolled patients treated with dual therapies including surgery or celiac plexus neurolysis. In addition, a subgroup analysis was conducted to evaluate studies that included patients with pancreatic duct strictures. A meta-analysis was performed and the data on pain relief was subsequently extracted, pooled, and analyzed. I2 index estimates were calculated to test for variability and heterogeneity across the included studies. Results Our final analysis included sixteen studies, comprising 1498 patients. Eleven studies presented data on immediate pain relief after endotherapy and twelve studies presented data on both immediate and long term pain relief (mean follow up was 47.4 months). The compiled result of the sixteen studies for immediate pain relief demonstrated 88% efficacy (95% NT CI [81.0%, 94%]) of endotherapy. Similarly, analysis of pain relief on long term follow-up showed a 67% efficacy of endotherapy (95% NT CI [58%, 76%]). The compiled complication rate for endotherapy in this review was 7.85% per ERCP/endotherapeutic procedure and the most common complications were acute pancreatitis, stent occlusion and stent migration. Conclusions Endotherapy is beneficial for both immediate and long term management of pain associated with chronic pancreatitis. The efficacy of endotherapy decreases over time as assessed by evaluating pain relief on long term follow up. Given the considerable heterogeneity of reported data, additional prospective and standardized multicenter studies need to be conducted to evaluate the efficacy of this modality in controlling pain associated with chronic pancreatitis.
Pancreatitis; Chronic
RCT randomized controlled trials
Chronic pancreatitis (CP) affects between 0.4% and 5% of the adult population throughout the world [1]. In the United States, chronic pancreatitis results in more than 122,000 outpatient visits and more than 56,000 hospitalizations per year [2]. The etiology of CP is often related to excess chronic alcohol and tobacco consumption and in western countries, CP is typically observed in young men between 36 and 55 years of age [3, 4]. The pathogenesis of chronic pancreatitis is not well understood and it is thought that chronic pancreatitis is due to multiple predisposing factors including – toxic metabolic, idiopathic, genetic and autoimmune - and therefore CP is a difficult condition to manage. It is characterized by progressive inflammation of the pancreas leading to destruction of pancreatic parenchyma and pancreatic ducts with subsequent development of fibrosis of the main pancreatic duct [5]. The morphologic changes in the pancreas are best visualized by endoscopic retrograde cholangiopancreatography (ERCP) and Endoscopic Ultrasound (EUS) [5]. However, with improvements in the sensitivity and specificity of noninvasive imaging modalities including CT and MRI, these modalities are increasingly being used to make the diagnosis.
Clinically, the most common symptom associated with chronic pancreatitis is recurrent or continuous pain. Pain is believed to be associated with increased pancreatic duct pressure secondary to proximal ductal stenosis with distal duct dilatation [6]. Other theories believed to associate with the pain in chronic pancreatitis include pancreatic ischemia, fibrosis, pseudocyst formation, and inflammation [6]. Pancreatic duct stones contribute to ductal hypertension by impeding pancreatic juice outflow, and thus leading to continual pain.
Treatment modalities for chronic pancreatitis include conservative therapy with analgesia, lifestyle and dietary modifications, endotherapy, and surgery. Pain management using analgesia is the mainstay of treatment for chronic pancreatitis and can be combined with other treatment modalities. Recently, published data suggests that early surgical treatment for intractable pain in patients with chronic pancreatitis helps preserve endocrine function and improve pain control [7]. Alternative therapies including celiac plexus block have also been used to alleviate pain with limited success [8].
Endoscopic therapy and specifically endotherapy (combined medical and endoscopic therapy) is a treatment modality that utilizes ERCP with pancreatic sphincterotomy, followed by extraction of stones with or without the use of extracorporeal shockwave lithotripsy (ESWL), placement of a pancreatic duct stent, and dilation of pancreatic duct strictures [9]. Endotherapy works by reducing intraductal hypertension, bypassing obstructed stones, restoring lumen patency in symptomatic strictures, and sealing main pancreatic duct disruption [9]. The aim of endotherapy is to decompress the main pancreatic duct (MPD) by performing complete stone clearance and ductal drainage, leading to MPD diameter reduction.
Several studies have reported on the efficacy of endotherapy as a first line treatment for CP pain but to date there are limited well-controlled studies. The results of the studies published on the use of endotherapy for chronic pancreatitis pain report variable long-term pain relief ranging between 32-92% [10, 11]. The wide range of reported long term pain relief is likely due to a lack of welldesigned studies and the heterogeneity of reported data.
The purpose of this systematic review and meta-analysis is to evaluate the utility of endotherapy in the management of pain associated with chronic pancreatitis. Specifically, we seek to elucidate and determine effect of endotherapy on pain relief associated with CP both immediately after treatment and on long-term follow-up. We then compare the results to published literature that evaluates the efficacy of alternative treatment modalities such as surgery. We hope that this systematic review and meta-analysis will help physicians develop a better treatment algorithm that can be used to treat patients suffering from persistent pain secondary to chronic pancreatitis.
A literature search of Medline with the PubMed interface from January 1988 to December 2014 and EMBASE from 1980 to December 2014 with the Ovid technologies interface was performed. Studies were then analyzed for the use of endotherapy for pain relief in chronic pancreatitis. We searched reference lists and published abstracts from conference proceedings to identify relevant trials.
We included large prospective studies, randomized controlled trials (RCT) and retrospective analyses. We included studied that reported immediate as well as longterm benefits associated with endotherapy and its role in pain management. Via a hand search, we also included abstracts or unpublished data if sufficient information on study design, characteristics of participants, interventions and outcomes were available and if full information, as well as final results, could be confirmed by contacting the first author. The search was performed using keywords: "Endotherapy in Chronic Pancreatitis Pain" [MeSH], "Stent Therapy in Chronic Pancreatitis Pain" [MeSH], and "Endoscopic Treatment in Chronic Pancreatitis Pain" [MeSH]. The search results including the title and abstract and all abstracts and manuscripts were reviewed by two independent investigators (MJ, and JS).
Exclusion criteria in our analysis included studies not written in the English language, small studies with less than 10 patients, and case series/case reports. Additionally, studies that simultaneously enrolled patients in multiple modalities of treatment such as endotherapy as well as subsequent surgery or celiac plexus neurolysis were also excluded. Each study was then carefully evaluated for appropriate randomization, number of patients enrolled, and method of diagnosis used to assess chronic pancreatitis.
Exact binomial confidence intervals were calculated individually for each endpoint within each study. Forest plots were constructed for each endpoint. We employed a random-effects model meta-analysis in order to calculate a pooled estimate of the proportion of patients experiencing short-term and long-term pain relief following endoscopic intervention. Heterogeneity was measured using I2 estimates. Funnel plots were also constructed in order to assess for the possibility of publication bias. The statistical analysis software used was Stata (version 12.0 College Station, TX: StataCorp LP).
Overview of Included Studies and Details
Our initial search produced 420 potential articles. After extensive review, 16 articles met our study criteria and were selected (Figure 1). Of these 16 studies, eleven were prospective and 4 were retrospective studies. Two studies were randomized controlled trials comparing surgery with endotherapy, while the remaining studies included observational analyses.
Our final data set included sixteen studies with a total of 1498 patients (Table 1). This data was pooled and aggregated. The primary endpoint assessed was pain relief immediately after endotherapy and pain relief at variable long-term follow-up periods (range 1.5-162 months). The most common scales used to assess pain included visual analogue scale, Melzack and the Izbicki pain scale [10, 12]. Two studies used secondary endpoints, which included weight gain and decreased use of narcotics, to gauge therapeutic success [6, 11].
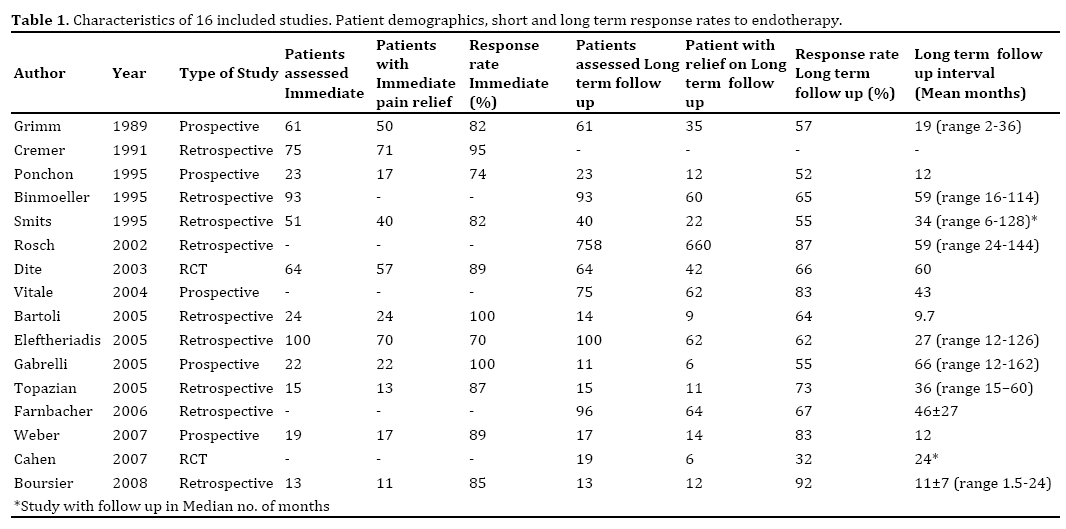
The procedural methods and materials used in endotherapy were similar across the selected studies (Table 2). Endotherapeutic procedures utilized in the studies included pancreatic duct cannulation after which a guide wire was maneuvered across the stricture. A pancreatic sphincterotomy was frequently performed to allow better drainage and easier instrumentation and stent placement. There was variation in the type of sphincterotomy performed, with some endoscopists using the standard pull type and other using the needle knife sphincterotomy and this was not reported in many of the studies. Stricture dilatation with a graduated dilating catheter or balloon dilator was utilized as needed. Pancreatic stents were advanced over a guidewire across the stricture using currently accepted methods. Extracorporeal shockwave lithotripsy (ESWL) was variably performed if large pancreatic stones were detected, via externally-applied, focused, high-intensity acoustic pulse to breakdown stones (Table 2) [9, 11, 12, 13, 14, 15, 16, 17].
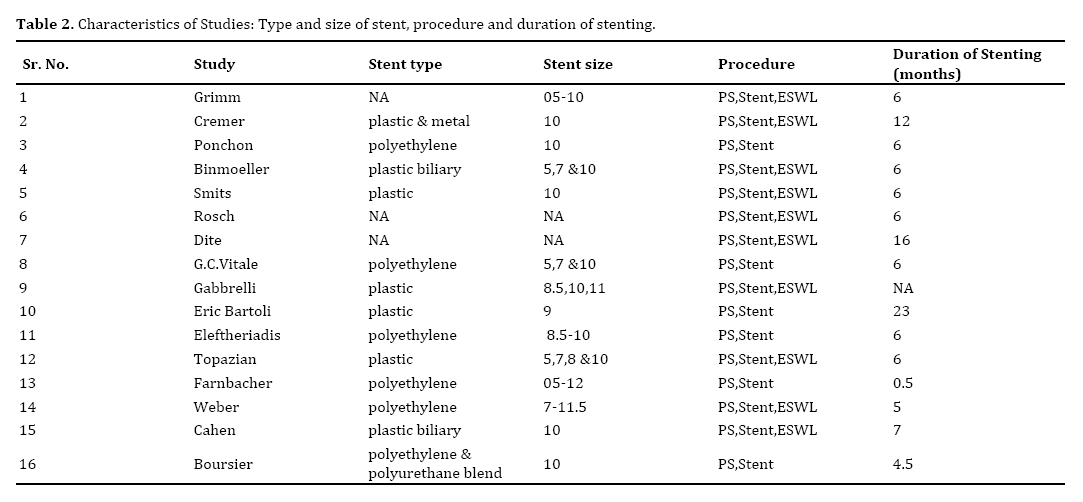
The characteristics of the stent used in the included studies depended on the size and location of the pancreatic duct stricture. The width of the stent placed varied across studies. If the pancreatic duct was small, typically a 4-7 Fr stent was used, whereas if the pancreatic duct was dilated a 10-11.5 Fr stent was used. Types of stents used included Teflon [10, 12], polyethylene [6, 11, 13, 14, 15, 16, 17, 18, 19, 20, 21] and metallic stents [11] (Table 2).
The exchange schedule utilized included an on-demand stent exchange schedule [13, 17, 20] and fixed exchange schedule [4, 7, 8, 9, 18, 21, 22]. The on-demand stent exchanges were based on symptomatic assessment of the patients and stents were exchanged at the initial onset of pain. While the fixed exchange schedule followed a fixed, pre-determined interval, irrespective of symptoms. Data regarding the number of stents placed during each procedure was not included in the majority of the included studies. The data regarding use of ERCP, EUS or both, was lacking in the individual studies.
In this meta-analysis, the pooled estimate of the proportion of subjects experiencing immediate pain relief was 88% (95% CI [81.0%, 94.0%]) and the pooled estimate of those with long-term relief was 67% (95% NT CI [58%, 76%]) (Figure 2). In the subgroup analysis of patients with pancreatic duct strictures, we included nine studies, comprising 536 patients. Seven studies included data for immediate pain relief and eight studies reported data evaluating sustained pain relief on follow-up. The compiled results for the efficacy in immediate pain relief is 74.7 % (95 NT CI [62.4%, 84.0%] while the results for sustained pain relief is 67.5% (95 NT CI [51.5%, 80.2%]).
Additionally, the compiled complication rate for endotherapy in this review was 7.85% per ERCP/ endotherapeutic procedure and the most common complications were acute pancreatitis, stent occlusion and stent migration (Table 3).

A Subgroup analysis for 5 prospective studies and 2 randomized trials was also conducted. The prospective studies showed a weighted mean for immediate pain relief of 84.76% (95% NT CI [77%, 90%]) and weighted long term pain relief of 68.9% (95% NT CI [61%, 74%]). The results for the RCT subgroup revealed a weighted long term pain relief of 58.2% (95% NT CI [47%, 68%]). Immediate pain relief was not calculated in the RCT subgroup as there was only one study that revealed this data.
The I² analysis was consistent with highly heterogeneous data for both the immediate and long-term follow-up intervals (I²=75.6% p<0.01, I²=88.1 p<0.01 respectively). In respect to the bias analysis, the Funnel plot for pain relief on immediate follow-up (Figure 3) does not demonstrate any obvious publication bias.
The data for variable long term follow-up (Figure 4) does show evidence of some publication bias, with the smaller studies showing less efficacy than the larger studies.
Chronic pancreatitis is characterized by an ongoing inflammatory proves, leading to morphological changes and pain within the pancreas. Although medical and lifestyle modification is beneficial, including analgesics, enzyme supplementation and antioxidant therapies, better therapeutic approaches are needed to manage symptomatic patients. Endotherapy is increasingly being used to manage pain associated with chronic pancreatitis. It provides a less invasive alternative to surgery. Endotherapy is becoming an increasingly utilized option for the management of CPP. This is in part due to technological advances and its less invasive nature in comparison to alternate modalities of treatment such as surgery.
According to the results in our systematic review and meta-analysis, the compiled pain relief with endotherapy was 88% on immediate follow-up and 67% on long-term follow-up. The results of our study shows that the pain relief in our cohort is better than surgery, which has a reported pain relief of 57-75% at long term follow-up [6, 7, 15, 16, 17]. Our results reinforce the use of endotherapy as a viable first line therapeutic modality for CPP and our pooled results are similar to that reported by other studies [10, 12, 13, 14, 23, 24, 25, 26, 27, 28].
Endotherapy is becoming an increasingly utilized option for the management of CPP. This is in part due to technological advances and its less invasive nature in comparison to alternate modalities of treatment such as surgery.
pooled complication rate for endotherapy is 7.85% which is lower than that reported for surgical management. It has been reported that surgical intervention frequently has major complications associated with it, and these complications requires further surgical intervention in up to 10.9% of patients and that there are minor complications in up to 28.3% of patients who undergo surgery [22]. Because the high morbidity and mortality and complication rate associated with surgery, endotherapy is a suitable alternative. Studies have also shown that endotherapy is associated with decreased anxiety and is better tolerated especially in patients with additional comorbidities including older age that make them poor surgical candidates and preclude them from surgery [28].
Limitations of this meta-analysis include the small number of published studies and the heterogeneous nature of the published data. There are few well-designed studies and less than five published randomized control trials compare surgery versus endotherapy. Furthermore, the majorities of the published studies are observational in nature and vary in their methodological design. Amongst these studies, there is also variation in pain assessment, selection of patients/ subjects, and differences in the size and type of stents used. In addition, the published RCTs in the literature do not mention if the statistical analyses used an intention to treat analysis to correct for non-compliant patients, such as those who continued to consume alcohol or when there was a nonrandom loss of study participants. Finally, the studies vary in their exchange rates for stent replacement (i.e. some studies use an on-demand schedule vs planned exchange schedule), which may offer some explanation for the range in pain relief on long-term follow-up.
Due to the heterogeneous nature of published studies, we suggest that future studies be conducted to evaluate the utility of endotherapy. Based on our analysis, we suggest that these studies use similar analgesic regimens and quantify the daily dose and specific the narcotic used by individuals before and after procedures (e.g. mg/day), as this is not clearly stated in the current literature. With the appropriate documentation, equianalgesic doses could be calculated to assess the amount of pain medication needed for pain resolution and allow for a more objective means of grading the severity of pain. Additionally, subsequent studies should attempt to use one standard method to grade pain. The subjective nature of pain scales makes comparing scales such as VAS and Izbicki pain scales difficult and this is also a limitation of our analysis. Furthermore, secondary parameters such as weight-gain, hospital visits, and decreased analgesic use should be universally adopted in future studies to help gather more objective data to assess clinical improvement. Another consideration that may be of benefit is intermittent ethanol levels and continued counseling being incorporated into each study, since the major cause of CP in this cohort is alcohol abuse. This would help assess if failed treatment was due to procedural failure or a lack of lifestyle modifications on the part of the patient. Furthermore, stent type and duration of placement are all confounding variables that can be resolved in subsequent studies by using the same type and size (Fr) of stent if possible (polyethylene vs. metal) as well as following the same exchange schedule (on-demand vs. scheduled). Assessment of efficacy vis-a-vis pain relief at long-term follow-up should be consistent. The range at which patients were followed up varied across the studies with a mean range from 9.7 months to 66 months. For long-term studies, more frequent follow-up intervals can be used to analyze intermediate-term efficacy [29, 30].
In conclusion, endotherapy is a safe and effective therapeutic modality for the treatment of CPP. Its utility appears to be best in the immediate period, but is reduced on long-term follow up. It is less invasive and has fewer complications, as compared to surgery which makes it a viable primary treatment of choice. In patients who have persistent CPP, endotherapy may act as a bridge to surgery as it does not preclude any further interventions. The significance of endotherapy is highlighted in patients who respond initially to treatment and are saved from undergoing unnecessary invasive procedures. This may result in preserved endocrine function and lower morbidity for the patient and ultimately reduce the overall burden of expense on the healthcare system.
The authors declare that they have no conflict of interest.