Case Report - (2017) Volume 18, Issue 6
Lifespring Cancer Treatment Center, United States
Received Date: August 14th, 2017; Accepted Date: November 07th, 2017
Pancreatic cancer is often considered one of the most deadly cancers because it is typically discovered late and there are few effective treatments for advanced stage disease. This is a case report of a 74-year-old woman with pancreatic adenocarcinoma with metastases to the peripancreatic retroperitoneal lymph nodes, liver, lungs, and left supraclavicular lymph node who is now over 11 years out from her original diagnosis of metastatic disease. This report describes the methodology of the patient’s treatment including the use of metronomic chemotherapy, combination chemotherapy, sequential therapies, and immunotherapy with the hope of providing a roadmap toward the successful treatment of this deadly cancer, and perhaps other cancers.
Administration, Metronomic; Antineoplastic Protocols; Drug Therapy, Combination; Immunotherapy; Pancreatic Neoplasms
ALL acute lymphoblastic leukemia; CTL cytotoxic T-cells; DC dendritic cells; GM-CSF granulocyte macrophage colonystimulating factor; HA hyaluronan; IFN interferon alfa-2b; MTD maximum tolerated dose; NaG: nab-paclitaxel and gemcitabine; NOLF nab-paclitaxel, oxaliplatin, folinic acid and 5-fluorouracil; NK cells natural killer cells; PaCT paclitaxel, cisplatin and oral trifluridine/ tipiracil; PaG paclitaxel and gemcitabine; PIC paclitaxel, irinotecan and cisplatin; POLF paclitaxel, oxaliplatin, folinic acid and 5-fluorouracil; Tregs regulatory T-cells
Pancreatic cancer claims the lives of approximately 43,000 people each year and is the third leading cause of cancer-related deaths in the United States. Metastatic disease has an exceptionally poor prognosis, with a 5-year survival of only 3%; the lowest of the cancers reported by the American Cancer Society. Despite a declining mortality rate for most other cancers, the mortality rate for pancreatic cancer has increased in recent years, which may be attributed to an increased disease incidence and lack of new effective treatments for the disease [1]. Current trends suggest that pancreatic cancer will become the second leading cause of cancer-related deaths in the United States by 2030 [2]. Long term survival with nonresectable metastatic pancreatic adenocarcinoma is rare and there are only sparse case reports published showing survival longer than 5 years. To our knowledge, this is the first case report published in a reputable journal of a patient with non-resectable metastatic pancreatic adenocarcinoma who has survived for longer than 10 years. There are two standard treatment regimens indicated for the treatment of metastatic pancreatic cancer: nab-paclitaxel and gemcitabine, and FOLFIRINOX. Median survival after diagnosis of metastatic disease, even with standard treatment, is short in the order of 8.5 to 11.1 months [3, 4]. Pancreatic cancer’s poor prognosis and lack of new therapy options highlight the need for the development of better treatments for this devastating disease. The following case report is of an 11 year survivor of metastatic non-resectable pancreatic adenocarcinoma. Her case is followed by the discussion of the treatment strategy that contributed her exceptionally long survival.
The patient is currently a 74-year-old woman who presented with an enlarged left supraclavicular lymph node at the age of 63 in late 2006. The work-up and diagnosis of this patient was made before the patient came to our clinic for treatment. She underwent a biopsy of her enlarged left supraclavicular lymph node in October 2006 which revealed an adenocarcinoma positive for two GI tract restricted markers and negative for eight markers for carcinomas primary to the lung, breast, and squamous differentiation (Figure 1). The patient’s pathology was most consistent with metastatic adenocarcinoma from the upper GI tract. A CT scan performed after her biopsy revealed peripancreatic retroperitoneal adenopathy at the level of the pancreatic head, dilatation of the main pancreatic duct, and secondary pancreatic duct, with additional lesions in the lungs and the liver (Figure 2). The scan findings combined with the pathology report were felt to be most consistent with the diagnosis of metastatic pancreatic adenocarcinoma. The patient obtained two opinions, including one from the University of Washington Medical Center, who all agreed that the patient’s diagnosis was most consistent with metastatic pancreatic adenocarcinoma. Given her presentation with non-resectable metastatic disease, it was felt at the time that the patient should start treatment sooner rather than later. Further work-up, such as a biopsy of the pancreatic head, could not be justified due to the poor prognosis of her disease and the possibility of complications that could delay starting treatment.
Figure 1. Slides from original biopsy specimen. An analysis of the original biopsy specimen of the left supraclavicular lymph node in October 2006 revealed an adenocarcinoma. Immunohistochemistry showed two GI tract restricted markers, CDX-2 and villin. These markers indicated that the primary site of the metastatic adenocarcinoma was most likely in the upper GI tract, as the markers of carcinomas primary to the lung (TTF-1, surfactant apoA), breast (estrogen receptor, progesterone receptor, GCDFP-15, mammaglobin), and squamous differentiation (p63, CK5/6) were negative.
The patient started on weekly paclitaxel and gemcitabine (PaG) in December 2006 (Table 1) with a significant clinical reduction in the size of her left supraclavicular lymph node. During this and all subsequent treatments, the patient received granulocyte macrophage colony-stimulating factor (GM-CSF) for chemotherapyinduced neutropenia and immune stimulation. The patient switched to daily erlotinib in March 2007 and continued on erlotinib for one month until she restarted weekly chemotherapy treatment with paclitaxel, oxaliplatin, folinic acid and 5-fluorouracil (POLF). She continued treatment with POLF until late-July 2007. A PET/CT scan in July 2007 showed a substantial decrease in her retroperitoneal adenopathy, significant improvement in the hepatic metastatic lesions and shrinkage of pulmonary nodules. The patient was switched back to daily erlotinib in July 2007 and started on low-dose interferon alfa-2b (IFN) for its immunostimulatory effects. In August 2007, the patient restarted on weekly chemotherapy treatment with POLF for an additional 3 months in combination with daily erlotinib. The patient later switched to every other day erlotinib for better tolerance. In December 2007, the patient changed treatment to weekly paclitaxel, ifosfamide, mesna, and bi-weekly doxorubicin liposome chemotherapy and continued until mid-March 2008. Her treatment was then switched in April 2008 to weekly paclitaxel, irinotecan, and cisplatin (PIC) which she continued until mid-July 2008. A repeat CT scan of the chest, abdomen, and pelvis in July 2008 showed an interval decrease in the size and number of multiple liver metastases with the residual lesions representing probable small liver cysts and a stable right upper lobe pulmonary nodule with no new nodules seen. The patient switched back to erlotinib and continued this treatment until late-September 2008. The patient then started on lenalidomide, an immunomodulatory drug for maintenance therapy. A CT scan of the chest, abdomen, and pelvis in October 2008 showed no evidence of recurrent or persistent pancreatic cancer (Figure 3); although, there were residual nodular infiltrates in the upper lobes of the lungs thought to be the result of an infection. The lesions in the liver were stable and most likely indicative of cysts. The patient was considered to be in complete remission and remained free of her disease for almost 6 years. A repeat scan in October 2010 and a PET/CT scan from skull base to mid-thigh in July 2011 showed no new pulmonary nodules, no definite pancreatic mass, no new hepatic lesions and no activity of progressive cancer. The patient discontinued lenalidomide in late-August 2012 due to intolerance.
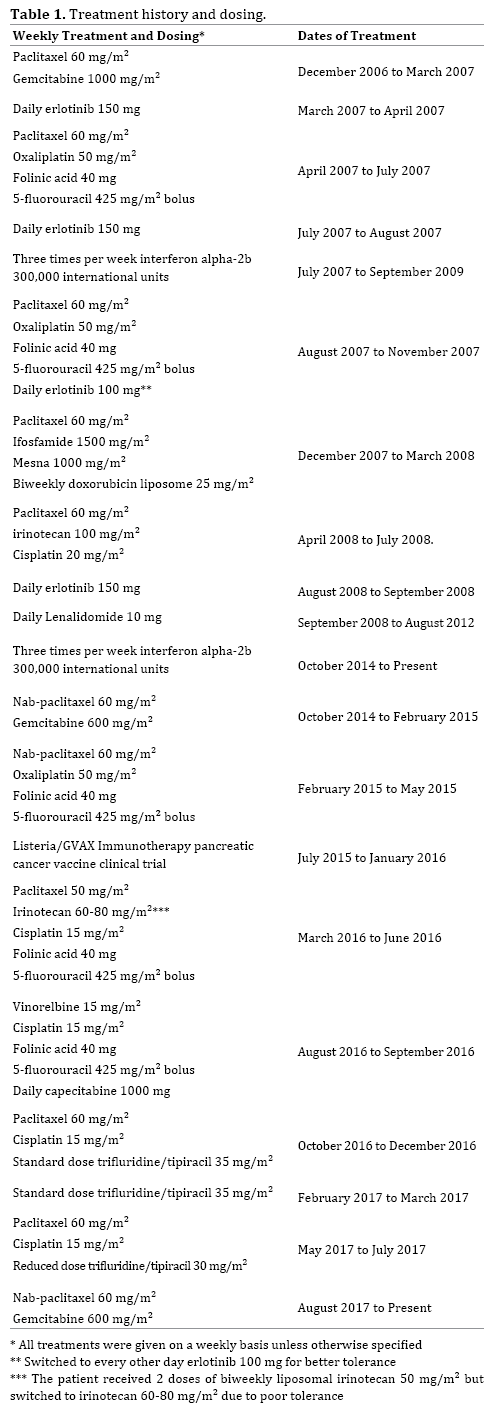
Unfortunately, in October 2014 the patient was under considerable stress and developed right abdominal discomfort. Blood work later revealed an elevated CA 19-9 of 322 (normal range: <37 units/mL). She underwent a PET/CT scan in October 2014 which revealed multiple new hypermetabolic liver lesions. A core liver biopsy showed an adenocarcinoma consistent with a metastasis from the patient’s original pancreatic primary.
The patient then restarted chemotherapy treatment with weekly nab-paclitaxel and gemcitabine (NaG) along with low-dose IFN in late-October 2014. The patient’s disease responded to treatment with a drop in CA 19-9, and a repeat CT scan in February 2015 showed a decrease in the size of the patient’s hepatic metastases. The patient switched treatments to weekly nab-paclitaxel, oxaliplatin, folinic acid and 5-fluorouracil (NOLF) in February 2015 and continued this treatment for approximately 3 months. A repeat CT scan in June 2015 showed stable disease, and the patient’s CA 19-9 decreased to within normal range. The patient then enrolled in a phase 2B clinical trial (NCT02004262) in early-July 2015 that investigated if the efficacy of a GVAX pancreatic cancer vaccine given with low-dose cyclophosphamide and live attenuated Listeria monocytogenes engineered to express mesothelin in previously treated patients with a histologically proven malignant adenocarcinoma of the pancreas. The patient was in the treatment arm that received 6 doses of modified Listeria alone. She participated in this clinical trial until a repeat CT scan in February 2016 revealed an increased size and number of hepatic lesions. Corresponding blood work showed her CA 19-9 had increased to 16,311.
The patient restarted chemotherapy treatment with weekly paclitaxel, irinotecan, cisplatin, folinic acid, and 5-fluorouracil in March 2016 and continued treatment until mid-June 2016. The patient originally started treatment with paclitaxel, liposomal irinotecan, folinic acid and 5-fluorouracil but did not tolerate liposomal irinotecan due to persistent nausea and vomiting and her liposomal irinotecan was switched to irinotecan after two doses. She then switched chemotherapy treatment to weekly vinorelbine, cisplatin, folinic acid and 5-fluorouracil in addition to daily low-dose capecitabine in mid-August 2016 and continued on this regimen until mid-September 2016. A CT scan in October 2016 showed overall stable disease except for an interval increase in the size of one liver lesion.
The patient then switched treatment to weekly paclitaxel, cisplatin and oral trifluridine/tipiracil (PaCT) in late-October, 2016 which she discontinued in late- December 2016 due to severe diarrhea secondary to Clostridium difficile. Her CA 19-9 had decreased in response to treatment and a repeat CT scan in January 2017 showed an interval decrease in multiple hepatic lesions to approximately one third of their previous size. After regaining strength from her C. difficile infection, the patient resumed oral trifluridine/ tipiracil alone in early-February 2017. Weekly paclitaxel and cisplatin were again added to the patient’s regimen in early- May 2017. The patient then switched treatment back to NaG in early-August 2017, which she continues on to try and control her disease.
The patient’s case of metastatic non-resectable pancreatic adenocarcinoma is one of remarkably long survival. We believe this patient’s unusually long survival is due to our treatment strategy which includes using a weekly metronomic dosing of chemotherapy, synergistic combinations of chemotherapy, switching chemotherapy regimens before disease progression, and using immune therapies. Two other patients treated with a similar strategy, although they were not treated exactly the same, also had survivals of over 5 years, with one case previously described in detail [5, 6]. Our strategy is as follows:
Metronomic Chemotherapy
Typically, a standard chemotherapy dosing schedule calls for a maximum tolerated dose (MTD) that is administered every 2 to 3 weeks. This break in treatment is necessary to allow patients to recover from acute toxicities associated with a MTD. In contrast, a metronomic chemotherapy dosing schedule utilizes lower doses of chemotherapy agents that are administered more frequently, without any prolonged drug-free breaks. Metronomic chemotherapy dosing allows for an increased dose density, or, frequency of chemotherapy administration. Dose-dense chemotherapy schedules are often more tolerable and can increase the efficacy of chemotherapy treatment [7, 8, 9, 10]. These chemotherapy regimens follow in line with the Norton-Simon hypothesis which suggests that tumor cell death is not maximized by administering high doses of chemotherapy, but instead by administering an effective dose of chemotherapy more frequently [11].
A dose-dense chemotherapy regimen can also increase dose-intensity, or, the total dose of chemotherapy administered per unit time. For example, our POLF and NOLF combinations use oxaliplatin at a dose of 50 mg/m² once per week, and our PIC combination uses irinotecan at a dose of 100 mg/m² once per week. In contrast, the standard FOLFIRINOX regimen uses oxaliplatin at a dose of 85 mg/m² and irinotecan at a dose of 180 mg/m² every 2 weeks. Therefore, our POLF/NOLF and PIC regimens have an increased dose-intensity of oxaliplatin (100 mg/ m² vs. 85 mg/m²) and irinotecan (200 mg/m² vs. 180 mg/ m²) when compared to the FOLFIRINOX regimen, and may consequently be more effective.
Although the dose-intensity of metronomic chemotherapy regimens can be greater, they are generally better tolerated as chemotherapy agents are given at a lower dose during each administration. This allows for better continuation of treatment without interruptions due to intolerable side-effects. For example, the FOLFIRINOX regimen is known to cause harsh sideeffects which can result in lapses in treatment. The poor tolerability of FOLFIRINOX results in a poorer quality of life for patients, and breaks in treatment can also allow for tumor cells to proliferate and mutate, resulting in disease progression. In contrast, the patient’s weekly metronomic chemotherapy regimens were generally well tolerated with the usual side effects associated with the chemotherapy agents involved, although all side effects were decreased in severity. The patient had an average ECOG score ranging between 1-2 throughout her treatment, which allowed her to continue treatment for the majority of each planned treatment cycle in addition to maintaining a good quality of life.
The primary mechanism of action of metronomic chemotherapy is thought to be its ability to enhance the antiangiogenic properties of certain chemotherapy agents [12]. In particular, there is preclinical evidence suggesting that paclitaxel and nab-paclitaxel have antiangiogenic effects when administered in low doses [13, 14, 15]. The increased vascularity of a tumor can decrease the effectiveness of chemotherapy delivery by diverting chemotherapy agents away from the tumor bed [16, 17]. By blocking angiogenesis, more chemotherapy may reach the tumor bed, thereby improving the efficacy of the cytotoxic chemotherapy agents. This is a major reason why paclitaxel and nab-paclitaxel were used in the majority of the patient’s treatment regimens.
In pancreatic cancer, another mechanism may also impair drug delivery in addition to, or in place of, angiogenesis. Stromal layers composed of hyaluronan (HA) are commonly found surrounding pancreatic cancers and are thought to decrease intratumoral chemotherapy delivery [18, 19]. In a recent clinical trial, the survival of patients expressing high levels of tissue HA improved when PEGPH20, a hyaluronidase, was administered with chemotherapy [20]. This finding highlights the importance of including an anti-stromal agent in a chemotherapy regimen when treating pancreatic cancer. Nab-paclitaxel has also been shown to decrease cancer-associated fibroblasts, which are thought to contribute to and promote the formation of the stromal layer [21, 22]. Paclitaxel may also have a similar effect since the patient responded to treatment when paclitaxel or nab-paclitaxel was used in her chemotherapy treatment regimens.
Combination Chemotherapy
A combination approach can be more effective than a single-agent therapy due to synergy between treatment agents. For example, the combination of nabpaclitaxel and gemcitabine has been shown to improve overall survival versus gemcitabine alone [3]. An ideal combination chemotherapy regimen is one where the chemotherapy agents are synergistic in efficacy against the disease while not being overly additive in their sideeffects. When one examines the side-effect profiles of the agents within the patient’s regimens, one can see that the major potential side effects of each agent generally differs from the other agents in each regimen. For example, the POLF regimen followed by the PIC regimen contains similar agents as in the FOLFIRINOX regimen; however, the main agents causing diarrhea (5-fluorouracil and irinotecan) and neutropenia (oxaliplatin and irinotecan) are kept separate between the POLF and PIC regimens. This method of selecting chemotherapy agents allows for better tolerability which in turn allows for more consistent and continuous treatment.
Sequential Therapy
Currently, the standard treatment protocol for metastatic pancreatic cancer generally involves continuing treatment until there is obvious disease progression. Drug resistance in tumor cells is seen as the primary cause of failure of chemotherapy treatment for cancer. The Goldie-Coldman hypothesis suggests that drug resistance mutations develop spontaneously over time, which can result in the selection of drug-resistant populations of cancer cells with treatment. Thus, the probability of a tumor cell developing resistance to a single chemotherapeutic agent increases in a short period of time [23]. The rationale behind sequential chemotherapy regimens is to decrease the chance of drug resistance and maximize efficacy of the treatment.
The idea of sequential therapy has been introduced successfully in maintenance therapy in advanced non-small cell lung carcinoma [24]. Sequential therapy has also found major success in acute lymphoblastic leukemia (ALL). A diagnosis of ALL was fatal for children in the 1950s. Today, this disease has a cure rate of more than 80 percent in children. The current clinical treatment for ALL involves sequential combination chemotherapy regimens in the remission-induction phase, intensification or consolidation phase, and maintenance phase. The treatment results from ALL have been considered one of the greatest achievements in oncology to this date [25]. In this case, chemotherapy regimens were purposely switched before obvious disease progression due to the concern of cancer cell resistance and to prevent the accumulation of chemotoxicity to a single chemotherapy regimen, approximately every 12 weeks (Table 1). Continuing chemotherapy and implementing sequential therapy may be more effective at reducing the total number of cancer cells over time, therefore allowing for optimal disease control [26].
Immunotherapy
The immune system is thought to play a major role in the treatment of pancreatic cancer. However, immune suppression from regulatory T-cells (Tregs) and the secretion of immunosuppressive factors in the tumor microenvironment can inhibit cytotoxic T-cells (CTL), natural killer cells (NK cells) and dendritic cells (DC) that are crucial to the body’s anti-tumor immune response [27]. The metronomic dosing of chemotherapy may decrease immunosuppressive cells, such as Tregs, allowing for an anti-tumor immune response [28, 29]. Using lower doses of chemotherapy also generally results in a less profound drop in blood counts, which allows for the preservation of the immune system. Moreover, aberrant blood vessels from angiogenesis may serve as a protective mechanism, diverting immune cells away from the tumor bed. The metronomic dosing of chemotherapy can also normalize aberrant blood vessels caused by angiogenesis and thus allow the immune system to better reach the tumor bed. In addition to the possible immunostimulatory effects of metronomic chemotherapy, the patient received 3 other immunostimulatory agents.
To stimulate the immune system and prevent neutropenia, 250-500 mcg of GM-CSF was administered intradermally and subcutaneously 2 to 5 times per week during the patient’s treatment. Typically GM-CSF is only administered subcutaneously, but the intradermal route of administration was also used because of the abundance of DCs found in the intradermal area. This immunostimulatory agent has been shown to produce the most potent anti-tumor immune response in comparison to other immunostimulatory agents such as interleukins and interferon gamma [30]. GM-CSF’s anti-tumor properties have also been used to enhance potential vaccines for several cancers, including pancreatic cancer [31].
To further stimulate the patient’s immune system, 300,000 international units of IFN was injected intradermally 3 times per week. Typically, IFN is not tolerated well, but the patient had no side effects secondary to this medication likely due to its low dose. IFN has known anti-tumor properties and has shown efficacy in the treatment of several types of cancer [32]. IFN’s antitumor properties may be related to its ability to stimulate DCs and NK cells. CTL cell stimulation is also thought to occur indirectly by the abolishment of tolerogenic DCs which prevents the induction of Tregs [33].
Lenalidomide was also used in the treatment of this patient as maintenance therapy post-chemotherapy treatment, which may have played a role in her 6 year period of remission. This drug has been used in the treatment of multiple myeloma and has antiangiogenic effects and immunomodulatory properties, such as stimulating CTLs and NK cells. Lenalidomide has also been shown to have anti-tumor effects in some solid tumors such as renal cell carcinoma [34]. The anti-tumor and antiangiogenic properties of this drug may be more efficacious in patients with minimal tumor burden.
We believe that weekly metronomic chemotherapy, combination chemotherapy, sequential therapy and the incorporation of immune therapies in this patient’s case each contributed to her long-term survival. We hope that this case report helps provide a roadmap for treatment of this devastating disease and perhaps a framework for the treatment of other types of cancers. Given that most patients with metastatic pancreatic cancer are given a prognosis on the order of months, the enduring survival of this patient of 11 years can provide a ray of hope for others with this disease. The treatment strategy used in this patient’s case should be further researched due to the potential significant medical, psychological, and economic implications.
We would like to thank Dr. Udo Schmiedl, M.D. Ph.D, Dr. Kathrin Ahl, M.D., and Dr. Kristin Manning, M.D., for their help with analyzing CT scan images, Dr. Jennifer LaPoint, M.D., for her help providing pathology slides, Matti Niemisto and Kin Lai for drafting earlier versions of this paper, and Chi Rho, without whom none of this work could have been done.
No source of funding was used to conduct this research or write this case report.
The authors have declared that no conflicts of interest exist.
Informed consent was obtained from the patient in the study for publication of this case report and any accompanying images. A copy of the written consent is available for review upon request.