Key words
Bangladeshi, client-focused, feeding
advisor, support worker
Introduction
There is increasing recognition that nutrition in the
early years of life is an important contributory factor
to both short- and long-term health. In order to
ensure that nutritional advice is responsive to new
evidence and best practice, the Department of Health
is informed and advised by the Food Standards
Agency (FSA) and the Scientific Advisory Committee
on Nutrition (SACN). In May 2003 the UK issued
guidelines initially recommended by the World
Health Organization that infants should be exclusively
breast-fed for the first six months (26 weeks) of life.
More recently, the Department of Health revised its
guidelines to include delaying the introduction of solids to six months for both breast and formula-fed
babies (Department of Health, 2004).
Communication
A key challenge for health professionals is the communication
of best practice to clients. This challenge
becomes more complex in situations in which clients
and professionals do not share the same language, or
those in which clients may not readily have access to
written sources of information. Many of the British Bangladeshi community living in the UK do not speak
English and are thus disadvantaged in their encounters
with the health service. A significant part of the
community originates from the district of Sylhet in the
north-east corner of Bangladesh close to the hills of the
Indian state of Assam. Many Bangladeshi women
have, at most, received a few years of primary school
education, which enables them to read simple Bengali
but not the equivalent of an English broadsheet, the
form often used for health information. The mother
tongue spoken in the Sylhet district of Bangladesh is
Sylheti, a dialect which has no written form and which
is quite distinct from Bangla. Many members of the
British Bangladeshi community who originate from
Sylhet therefore struggle to understand the educated
Bangla language.
Most Bangladeshi women therefore do not have
ready access to health information in English or their
mother tongue. In their meetings with health professionals
an interpreter can minimise difficulties,
but cannot remove them. Consequently, Bangladeshi
mothers may not be able to find the information and
advice they need, for example, in relation to child
health. A national survey found that Bangladeshi
parents expressed the highest levels of concern of all
groups in relation to their children’s feeding (Thomas
and Avery, 1997).
Weaningpatterns
Studies about weaning from the point of view of
parents are relatively rare, particularly when seeking
parents’ perceptions in the South Asian community.
One such study by Sarwar (2002) investigated feeding
practices by Pakistani women both in the UK and in
Pakistan. However, there is an extensive literature
from the 1970s to the present day that records health
professionals’ concerns and observations relating to
weaning practices and children’s feeding patterns
within the South Asian community in the UK. The
literature often describes feeding practices that result
in an inadequate diet and, by implication, the failure
of health visitors to effect change in the family’s
management of the weaning period (Griffiths, 2000).
The prolonged and excessive use of milk, as well as
dependency on sweetened weaning foods, are consistently
cited as contributory factors to the high levels of
iron deficiency anaemia found in children from South
Asian ethnic backgrounds (Daly et al, 1996; Lawson
et al, 1998). However, such studies, generally, do not
engage with the reasons why health professionals
might be ineffective in their advice, or explore why
families offer their children a diet that relies heavily on
milk and sweetened baby foods extending into the
toddler period. Yaha (2001) provides an exception in writing frankly and sympathetically about her experiences
both as a daughter and mother in a Bangladeshi
family and as a health visitor working in Tower
Hamlets. She mentions the difficult problem of force
feeding, which ‘good’ mothers do to ensure that their
children eat well. Fat children are seen as healthy and a
sign of good parenting. The health professional, however,
may perceive the situation differently as she sees
a child, who is force fed, food aversive and crying at the
sight of a spoon. Yaha (2001) also recognises the effect
of spiritual beliefs on weaning practices, and their
relevance to data analysis will be referred to later.
During the last 20 years, a number of studies have
concluded with fairly general recommendations for
improving weaning practice; for example, the use of
pictorial charts, and the need for cultural sensitivity
and using interpreters. These rather vague observations
give justification to Bhopal and White’s (1993)
identification of the need for research within the field
of health promotion for ethnic minority groups that
has clear measurable objectives. Similarly Randhawa
et al (2000) suggest the advantage of a focused approach
is, ‘to make progress in a handful of target areas
– with the option to evaluate, and the possibility of
identifying workable models for successful action ...’
Two specific areas of interest emerge from this
review. First, there is a dearth of evidence exploring
the experiences of British Bangladeshi families, and
other South Asian families in general, of feeding
their children. Studies are usually from the health
professionals’ perspective, noting the child’s diet and
feeding practices. Second, in the various approaches
that have been adopted in the promotion of healthy
feeding practices, there is a need to identify processes
that make interventions effective, from both the service
provider’s and the service user’s viewpoint. This
paper addresses this second issue by presenting an
evaluative account of a client-centred intervention for
Bangladeshi families with children of weaning age.
The next section explains the intervention. This explanation
is followed by an account of the evaluation
of this intervention and the outcomes achieved. The
paper closes with a discussion of the need for health
services that are client centred, and suggests that the
weaning intervention shows some evidence for increasing
access to health services for a particular client
group.
The intervention
Earlier studies involving South Asian communities
tended to refer to Asians and South Asians as a
homogenous unit; for example, Jivani (1978) discusses
feeding practices in relation to ‘Asian infants’, while
Duggan et al (1991) refer to ‘young Asian children’. However, more recent studies have attempted to distinguish
between different ethnic groups within the
South Asiancommunity (Khan and Randhawa, 1999).
This study sought to make a contribution to the literature
concerning weaning by focusing on the experiences
of the Bangladeshi community living in one UK
town. A number of local health visitors working with
Bangladeshi families had acknowledged the limitations
of the weaning advice they were able to offer,
due to the challenges of communication that arose
despite the use of interpreters. The health visitors
identified an urgent need to develop an intervention
that enabled the Bangladeshi families to access and
utilise weaning information in a culturally competent
manner. The key aim of the intervention was to
employ the skills of specially trained support workers,
infant feeding advisors, in offering a client-centred
weaning service to Bangladeshi families.
Recruitingand trainingthe infant
feedingadvisors
The proposed intervention was based on work carried
out with Pakistani families (Smith and Randhawa,
2004). It aimed to be sensitive to the specific needs of
the community, attempting to overcome the challenges
of communication described earlier. The infant
feeding advisors were integral to this intervention, and
therefore careful thought was given to personal
characteristics of individuals who were to be recruited
to these posts. The infant feeding advisors were
specially trained support workers who shared a similar
linguistic and ethnic background with the clients they
visited. The criteria for selection were community
work experience, fluency in the relevant South Asian
languages, as well as English, and empathy with their
ethnic community. The infant feeding advisors had all
been employed as linkworkers in the primary care
trust andwere therefore accustomed to workingwith a
wide range of health professionals. The infant feeding
advisor role involved managing a caseload of families,
delegated by the family health visitor, and undertaking
home visits independently of other health professionals.
The work required up-to-date knowledge
of current weaning advice, including the ability to
support the maintenance of breast-feeding during the
weaning period. The infant feeding advisors undertook
training courses to prepare them for home visiting and
offering weaning advice and support. These courses,
each of 30 hours’ length, were accredited by the Open
College Network (www.ocnotc.com). The subject
areas covered included topics such as working alone,
confidentiality, accountability and communication
skills, as well as an in-depth examination of the
weaning process.
Key components of the intervention
The intervention provided for continuity of information
giving by offering visits to the client’s home at
monthly intervals during the weaning period (Box 1).
The frequency of visits enabled the infant feeding
advisor and the family to build a relationship, which
was considered essential to the success of the intervention.
The initial visit was made when the baby was
three months old, and the intervention was completed
following the baby’s first birthday. The infant feeding
advisor’s role was to support, to encourage and to
provide evidence-based information. At each visit the
feeding advisor completed a questionnaire, which was
designed to enable the mother to articulate her experience
of feeding her child before the infant feeding
advisor formulated her advice. This was considered
pivotal to the intervention as it ensured that the
client’s needs were heard and addressed. Although
the intervention allowed for monthly visits to the
client’s home, the frequency of visits was flexible
depending on the individual client’s needs and circumstances,
and visits were initiated by either the
client or the infant feeding advisor.
Box 1 :Core components of weaning
intervention
The importance of building a rapport with the client as
well as offering evidence-based weaning information
was fundamental to the weaning intervention. The
focus of this intervention was always concerned with
effective communication. From other studies that
describe health visiting interventions to improve
weaning practices (Childs et al, 1997; Griffiths,
2002), and our experience locally, it was apparent
that health visitors had often been unsuccessful in
providing appropriate feeding advice. Crucially this
was not simply an issue of speaking the same language
as the client. The importance of rapport and relationship
between the client and the caregiver was
fundamental to offering support and advice that was
personal and sensitive to the individual’s situation
(Randhawa et al, 2003). Rapport and relationship
were recurrent themes throughout the training of
the infant feeding advisors, and during their ongoing
mentorship and supervision. Effective communication
using evidence-based weaning information was core to the intervention. A part of this process was the use
of the written word. Weaning information provided
by the infant feeding advisors, who were able to speak
with the families in their preferred language, was
supported by double-sided A5 leaflets written in plain
English. The development and use of audiotapes was
not considered to be particularly advantageous. The
results of a study undertaken in Birmingham, in which
the use of audiotapes was incorporated into a dietary
health education programme, did not appear to demonstrate
their effectiveness (Childs et al, 1997).
Methodology
The intervention was introduced as a pilot scheme in
2003/2004 and was offered to Bangladeshi families
with children aged three months, who were registered
with identified general practitioners (GPs). Premature
babies and families with complex medical and social
needs were excluded from the study. There were no
other inclusion or exclusion criteria.
Formal evaluation of the pilot was undertaken
using a broadly qualitative methodology. Following
the child’s first birthday the intervention was completed,
with the infant feeding advisor undertaking her
final visit. She reminded each family that the project
health visitor would contact them in order to arrange a
mutually convenient time to complete a questionnaire
about the intervention. A linkworker, who worked
independently of the intervention, was appointed to
undertake joint visits with the project health visitor to
those families whose preferred language was Sylheti or
Bangla. The linkworker was prepared for this role by
discussion regarding the purpose of the evaluation,
and in particular the translation of the questionnaire
into Sylheti or Bangla as appropriate. Without a
written translation, this process was especially important,
as the linkworker needed to familiarise herself
with the questionnaire, ensuring that she was able to
offer conceptually equivalent questions, in a consistent
form. The semi-structured questionnaire was
therefore administered verbally by the project health
visitor. Families’ answers were written down at the
time of the interview, with simultaneous translation
by the linkworker where necessary. Quantitative data
were recorded using Excel, and the remaining data
themed.
The evaluation sought the women’s perspective on
their children’s feeding. Their responses indicated the
extent to which the intervention had achieved its
objectives. In addition the questionnaire asked the
parent/carer’s views on the intervention. Questions
were designed as recommended by Bowling (1997) to
elicit the study’s effectiveness, enabling an assessment
to be made of the child’s feeding, and its appropriateness, in this instance, the receiving of advice from a support
worker in their own home.
Ethical approval for the study was sought and given
by the chairperson of the local research ethics committee
(LREC). Additional to the issues that govern all
ethical research was the challenge of working in a
cross-cultural setting, where some of the participants
did not speak English. Enabling the clients to give
informed consent was of particular concern.
Obtainingconsent for the
intervention
A staged process was developed to obtaining consent.
This enabled the participants to have at least three
opportunities to seek information regarding the
study, and to decide to accept or decline participation
in the intervention. Initially, the family health visitor
discussed the proposed intervention with the family at
the child’s six-week development check and offered
written information regarding the study. When the
child was three months of age, the infant feeding
advisor contacted the family by phone to discuss
participation in the weaning intervention, and, if the
family were still interested, an appointment for a
home visit was made. At this visit, undertaken by
both the project health visitor and the infant feeding
advisor, participation in the intervention was discussed
again and written consent sought. At this point
four families, for various reasons, ranging from a
planned trip to Bangladesh to feeling the family did
not require this level of intervention, declined to
participate.
Evaluatingthe intervention
Following the child’s first birthday the project health
visitor visited the families to evaluate the intervention
(Box 2). Parental and professional concerns around
feeding were grouped around certain themes, and
these informed the basis for choosing the objectives.
Parents frequently reported that ‘my child doesn’t eat’.
The reason for the concerns often stemmed from an
excessive milk intake, resulting in a lack of appetite for
food. Typically such a child will be fed sweetened baby
foods and possibly some cereal. In consultation with a
dietitian, it was decided to make the first objective
family food, the five food groups as appropriate to a
one year old, and milk intake not exceeding 750 ml in
24 h. Families were offered a feeding cup when their
child was six months old, and as part of promoting
good oral health the use of a cup or beaker was
encouraged. Many families offered water from a glass
but followedUKculture in using a baby bottle for milk
and other drinks. Drinking froma cup or beaker tends
to prevent the overfeeding of milk in the older child. Long-term health concerns that may result from
prolonged bottle-feeding are discussed in a Briefing
Paper from the Community Nutrition Group of
the British Dietetic Association (1997). Traditional
Bangladeshi food is easily adaptable to enable young
children to self-feed using their hands. Parents who
reported feeding problems in older toddlers often said
they did not allow self-feeding because of the amount
of mess this created. In order to encourage the development
of self-feeding skills, a child finger feeding at
one year formed the final objective.
Box 2:Objectives for a child aged one year.
The questionnaire, including a 24-h food recall
diary, consisted of three broad topic areas, namely
the parent’s perception as to how the child was
feeding; the family’s, usually the parent’s, opinion of
weaning support as offered through the weaning
intervention; and lastly their use of the written information
on weaning that had been given to them. The
questionnaire allowed the collection of qualitative
data, particularly in relation to the parent’s perceptions
of their child’s eating. In addition, numerical
data, for example about the number of children
drinking from a cup rather than a bottle, were
measured. The information obtained from the food
diary, supported by the response to a question eliciting
the range of foods eaten, indicated whether each
child’s diet included the five food groups, appropriate
to the needs of a one year old. The possible effect of
cultural beliefs was recognised in the analysis of the
data. For example, one of the linkworkers suggested
that the parents would be reluctant to say their child
was feeding very well, because of nazar or the evil eye,
‘otherwise he’ll stop eating, he’ll lose weight’. This
phenomenon is not unique to this study population,
and has been discussed previously by Yaha (2001).
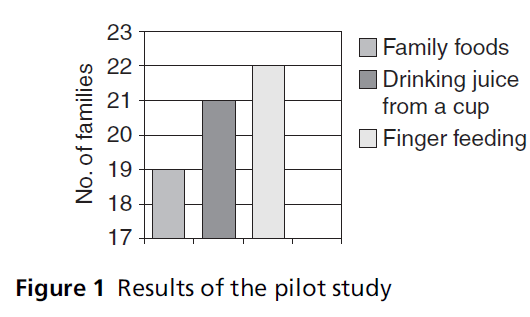
Outcomes of the evaluation
Twenty-four families completed the intervention,
twenty-two of whom were visited for the evaluation
(Figure 1). Four mothers thought their children fed
very well, with an equal number who considered that their children did not feed well. The remainder were
satisfied with how their child was eating. The use of
cups/beakers for drinks other than milk had been
encouraged throughout the intervention, and with
the exception of one child, everyone was using a cup
for drinks other than milk. However, all the children
continued to drink milk from a bottle although one
child sometimes drank milk froma cup. Two children
were breast-fed. All the families reported that the
children were finger feeding.
Figure 1 :Results of the pilot study
Theweaning intervention waswell received by clients.
They reported increased knowledge about the weaning
process and often used this knowledge to inform
their friends and relatives. Clients suggested the service
should be expanded beyond the pilot, and also
asked for leaflets to be available in Bangla as well as in
English. The women spoke confidently about their
own knowledge and how their children were feeding.
English-speaking mothers appeared to gain as much
benefit from the intervention as those who were non-
English speaking. A mother who was also a nursery
nurse said:
‘I didn’t know what to feed him but with [the infant
feeding advisor’s] help I knew exactly what to do.’
Similar views were expressed by many of the women
and are reflected by this Sylheti-speaking mother:
‘She has everything on time, everything she is given. When
I first started weaning I gave her food without salt. With
my three other children I didn’t know what to do, no
feeding advisors were available. I wasn’t aware what foods
to give or not to give like rice pudding. This time I didn’t
buy jars, I bought the fresh vegetables and boiled them.
She hasn’t fallen ill since I’ve been boiling vegetables. I was
advised not to give sugary drinks. I cut down on sugar and
salt. You can obviously feed the child anything, but what is
right for the child it’s crucial to know. If I went into the
chemist before I’d buy egg custard and rice pudding, I
never gave fresh vegetable. It’s good for other mothers
especially if it’s the first or second child. If a woman is on
her own she doesn’t know what to do. I suffered a lot with
the eldest.’ Over 80% of the women preferred to speak Sylheti, a
factor that demonstrated this client group’s vulnerability
to missing key health messages. Repeatedly,
women, including English-speaking mothers who had
had previous children, indicated that the weaning
knowledge they had gained was new information.
The parents’ responses in this small study appear to
indicate that one of the benefits of employing feeding
advisors who are empathetic and knowledgeable of
the culture, as well as possessing the relevant language
skills, is a more effective exchange of health information
and improved dialogue between the client and
practitioner.Women, both mothers and grandmothers,
showed an increased acceptance and use of health
information, suggesting that the encouragement of a
client-centred approach should be given priority in
the development of new services. The infant feeding
advisor was reported to be a key person who intuitively
knew what advice and support were acceptable in
certain situations. She was able to break down barriers
that were independent of language. The acknowledgement
by a number of the mothers that they had gained
new knowledge was associated with a rise in confidence
because they knew what to give their children.
One mother commented that she looked forward to
the infant feeding advisor’s visit each month, and liked
being praised for the way she weaned her child.
Conclusion
The importance of nutrition in the first year of life and
its effect on health and development of children and
in later life are increasingly recognised (Subgroup on
Maternal and Child Nutrition of the Scientific Advisory
Committee on Nutrition: www.sacn.gov.uk). The
current study showed that, notwithstanding a primary
healthcare system that offers a universal health visiting
service, mothers often expressed their lack of knowledge
concerning weaning. The majority of mothers
would have received routine feeding advice through
child health clinics and at developmental checks but,
for many, this information seems not to be transferred
into practice. This appears to be supported by the
continued interest of health professionals in relation
to the weaning diet in the South Asian community
(Yaha, 2001; Griffiths, 2002; Sarwar, 2002). Uncertainty
about which commercially produced baby foods are
halal, or lawful in terms of Islam, means that there has
traditionally been a greater use of sweetened baby
foods as well as an apparent lack of confidence in the
use of family foods (Sarwar, 2002).
The need for a culturally competent client-based
service that ensures that families are able to access and
utilise weaning information is clearly apparent. Within
the intervention described, the emphasis on relationship building, as well as offering staged advice through
visits to the client’s home by support workers from a
similar ethnic and linguistic background, seemed to
demonstrate that the manner in which information
was offered through the weaning intervention enabled
most of the mothers to assimilate and put it into
practice. This reflects the evidence for the role of care
in nutrition programmes recognising the importance
of the interaction between carer and child (Engle,
2000). Engle (2000) describes nutrition programmes
that focus only on advice, without care.
It is not known whether families will be able to
maintain healthy feeding practices, particularly when
their children want greater independence and choice.
It is possible that dependency on milk will increase,
particularly if children are not encouraged to use
beakers or cups. However, a long-term evaluation is
planned for when the children are two years old.
CONFLICTS OF INTEREST
None.
References
- Bhopal R and WhiteM(1993) Health promotion for ethnic minorities: past, present and future. In: Ahmad W (ed). ‘Race’ and Health in Contemporary Britain. Buckingham: Open University Press, pp. 137–66.
- Bowling A (1997) Research Methods in Health. Buckingham: Open University Press.
- British Dietetic Association (1997) From Bottle to Cup. A Briefing Paper from the Community Nutrition Group. www.s125758931.websitehome.co.uk/news_page.htm# bottletocup (accessed 9 May 2006).
- Childs F, Aukett A, Darbyshire P, Ilett S and Livera LN (1997) Dietary education and iron deficiency anaemia in the inner city. Archives of Disease in Childhood 76:144–7.
- Daly A, MacDonald A, Aukett A et al (1996) Prevention of anaemia in inner city toddlers by an iron supplemented cows’ milk formula. Archives of Disease in Childhood 75: 9–16.
- Department of Health (2004) Infant FeedingRecommendation. London: Department of Health.
- Duggan M, Steel G, Elwys G, Harbottle L and NobleC(1991) Iron status, energy intake, and nutritional status of healthy young Asian children. Archives of Disease in Childhood 66:1386–9.
- Engle P, Bentley M and Pelto G (2000) The role of care in nutrition programmes: current research and a research agenda. Proceedings of the Nutrition Society 59:25–35.
- Griffiths B (2000) Improving infant nutrition: a health visiting intervention. Community Practitioner 73:432–4.
- Griffiths B (2002) A health visiting intervention to improve the outcome of weaning. Community Practitioner 75: 420–3.
- Jivani S (1978) The practice of infant feeding among Asian immigrants. Archives of Disease in Childhood 53:69–73.
- Khan Z and Randhawa G (1999) Informing the UK’s South Asian communities on organ donation and transplantation. EDTNA/ERCA Journal xxvi:12–14.
- Lawson MS, ThomasMandHardimanA (1998) Iron status of Asian children aged 2 years living in England. Archives of Disease in Childhood 78:420–6.
- Randhawa G, Owens A, Fitches R and Khan Z (2003) The role of communication in developing culturally competent palliative care services in the UK. International Journal of Palliative Nursing 9:24–31.
- Sarwar T (2002) Infant feeding practices of Pakistani mothers in England and Pakistan. Journal of Human Nutrition and Dietetics 15:419–28.
- Smith S and Randhawa G (2004) Extending the role of the linkworker in weaning support. Community Practitioner 77:146–9.
- Thomas M and Avery V (1997) Infant Feedingin Asian Families. London: The Stationery Office, p. 80.
- Yaha H (2001) Weaning in the Bangladeshi community: problems observed. Community Practitioner 74:299–301.