- (2004) Volume 5, Issue 4
Annette Fritscher-Ravens*
Department of Gastroenterology - Endoscopy Unit, St. Mary`s Hospital, Imperial College. London, United Kingdom
Diagnosis; Diagnostic Techniques and Procedures; Diagnostic Techniques, Digestive System; Endosonography; Neuroendocrine Tumors; Pancreas
ASVS: arterial stimulation and hepatic venous sampling; EPDU: enhanced power Doppler ultrasound; GHRF: growth hormone releasing factor; MEN: multiple endocrine neoplasia; PNET: pancreatic neuroendocrine tumours; SRS: somatostatin receptor scintigraphy; PTHP: parathyreoid hormone releasing peptide
Neuroendocrine tumours of the pancreas (PNET) - although rare - are the most common endocrine neoplasms of the abdomen. They are heterogeneous regarding hormone production and biological behaviour, hence causing a variety of clinical presentations. Tumours that release ectopic hormones cause distinct clinical syndromes and are commonly detected by biochemical tests. Non-functioning neuroendocrine tumours (nPNET), however, may not present with clinical symptoms until they produce tumour mass effects at a late stage of tumour growth. Because of the lack of symptoms they are much more difficult to diagnose. Even if an early pancreatic lesion were detected accidentally, the differential diagnosis would not necessarily include a non-functional neuroendocrine tumour. Not only are these tumours commonly detected late but they are also more likely to be mistaken for an exocrine pancreatic adenocarcinoma [1].
Complete surgical resection is the only curative treatment for neuroendocrine pancreatic tumours. The type of surgery is dependent on the location, tumour size, infiltration into adjacent organs and tumour type, as different neuroendocrine tumours have different patterns of spread (of the lesion itself, locoregional and metastatic disease) and behaviour. If there is only a single small tumour with no evidence of spread it may be suitable for pancreatic organ preserving surgery such as enucleation or middle segment resection rather than extensive pancreatic resection [2, 3, 4].
A tailored surgical approach requires adequate preoperative planning including the best possible information on the number of lesions, their exact size and location, relation to adjacent vessels and organs and presence of locoregional or distant metastases. Preoperative localisation can, however, be difficult, as these tumours are frequently smaller than 2 cm in diameter.
Traditional imaging methods such as transabdominal ultrasound (US), computed tomography (CT) and magnet resonance imaging (MRI) fail to present the necessary information or to detect the tumour itself in up to half of the patients.
Endoscopic ultrasound (EUS) provides high resolution images of structures within or just beyond the wall of the gastrointestinal tract which allows the detection of lesions down to 0.3-0.5 cm [5]. This ability to image small structures close to the gastrointestinal tract cannot be matched at present by any external imaging method despite continued technical developments and improving resolution. Consequently, EUS has established a role as a powerful tool to detect and stage gastrointestinal cancer or small lesions within 5 cm of the gut wall such as pancreatic malignancies. It allows detailed visualisation of the entire pancreas and is likely to be an effective tool for localisation of neuroendocrine pancreatic tumours. EUS guided fine needle aspiration may provide a cytological diagnosis in cases of doubt or for the diagnosis of non functioning tumours. This review will attempt to evaluate the role of EUS and EUS-FNA in neuroendocrine pancreatic tumours and compare this technique to other preoperative imaging methods in view of the requirements necessary for appropriate management of the disease.
Neuroendocrine tumours are rare entities with a prevalence of 1/100,000 [6]. They are classified into two major groups: hormone producing functioning tumours (pPNET) and non-functioning tumours (nPNET). The frequency of insulinomas, nPNET and gastrinomas is about the same and these are two to eight times as common as VIPomas and 17-30 times as common as glucagonomas [1, 6].
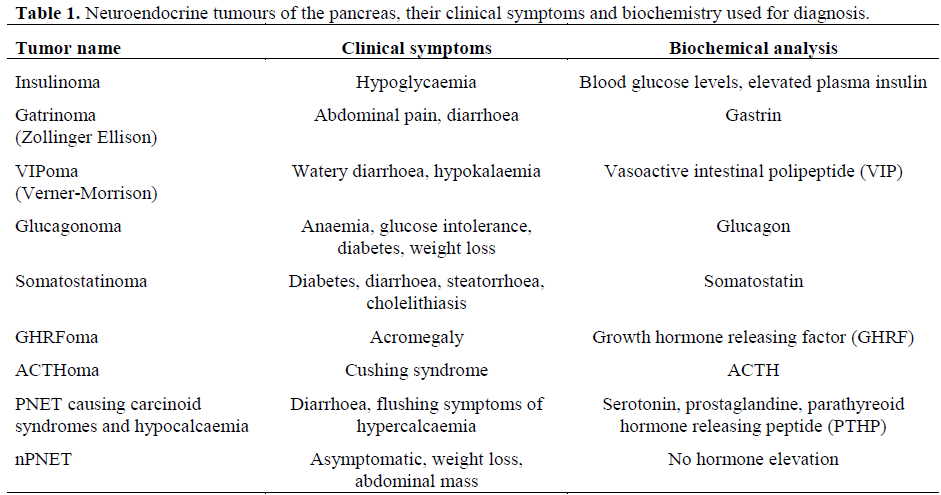
More than 50% of pPNET produce more than one hormone, when analysed by immunocytochemistry [7, 8, 9]. Although multiple peptides may be produced, only one is usually biologically active and released in sufficient quantity to cause symptoms [1]. Because multiple hormones may be present in PNET it can be difficult - if not impossible - to determine by immunocytochemistry which of the hormones is clinically relevant. The diagnosis should be made from the clinical symptoms and measurement of secretory products (Table 1). Even nPNET, which make up 15-30% of cases, may elaborate hormones [10]. The lack of clinical symptoms is due to insufficient peptide production, insufficient release, or concurrent secretion of inhibitory peptides by the tumour.
It is difficult to classify PNET into benign or malignant disease in all cases except insulinomas which usually remain benign. The histological classification has failed to predict the growth pattern or malignancy [9]. Malignancy can only reliably be defined by the presence of metastatic disease while benign disease can only be defined by long term clinical follow-up [8, 9].
There is a correlation between size and malignancy, whereas size is not relevant for the severity of hormonal symptoms [9, 11]. Insulinomas and gastrinomas tend to present as small tumours but may be multifocal (Figures 1 and 2) [12, 13]. Other than pancreatic adenocarcinomas (Figure 3) or focal chronic pancreatitis all of these tumours are hypervascular which may be used for differential diagnosis (Figure 4).
As the tumours may be very small, it can be difficult to detect their exact location. Appropriate treatment, however, is only possible when sufficient information about the primary tumour location and tumour extent is available. As surgery is the only curative treatment possible locoregional or liver metastases need to be defined preoperatively. Various conventional imaging modalities are used to achieve this goal.
Most of the insulinomas and gastrinomas are 0.5-2 cm in diameter and are frequently missed by US, CT or MRI (Figures 1 and 2). In recent studies results of all three imaging techniques vary from 9 to 48% in the detection of these tumours [14, 15, 16]. Although most reports of US, CT and MRI are discouraging with a sensitivity of 29-60% for all pancreatic neuroendocrine tumours [1, 14, 15, 16], there are some reports of more promising results in detecting PNET.
Enhanced power Doppler ultrasound (EPDU) after injection of levovist (Schering, Berlin, Germany) has been used in 104 patients with suspected neuroendocrine tumours and compared to somatostatin receptor scintigraphy (SRS). Sensitivity for the differentiation of hypervascular neuroendocrine tumours and other pancreatic masses was 94% for EPDU and 54% for SRS [17].
Gouya et al. showed that it might be important which kind of CT is used for tumour detection [18]. Thirty-two pancreatic insulinomas underwent preoperative CT with dual-phase thin-section multidetector CT (group 1), dual-phase multidetector CT without thin sections (group 2), or sequential CT (group 3). The diagnostic sensitivity for group 1 was 94%, 57% for group 2, and 29% for group 3 [18], while Fidler et al. were able to prospectively detect only 63% of 30 patients with insulinomas using multiphase helical CT [19].
Although in some studies MRI does not seem to achieve better results in localising PNET than US and CT [14], Thoeni et al. [20] report of 28 patients with clinically suspected islet cell tumours. T1- and T2-weighted spin-echo MR demonstrated these tumours in 85% of patients [20].
However, in all these imaging modalities neuroendocrine tumours may only be detectable once they have grown to a certain size.
As all neuroendocrine tumours are hypervascular, angiography may be more efficient in the demonstration of those tumours. Studies reporting sensitivities of 17- 55% do not suggest an advantage over other less invasive imaging modalities [21, 22, 23, 24]. Selective arterial stimulation and hepatic venous sampling (ASVS) technique using intra-arterial calcium as the insulin secretagogue may be more precise in the diagnosis of insulinomas [23].
Somatostatin receptor scintigraphy (SRS) has been advocated to localise neuroendocrine tumours in a number of studies. It has been shown that for all neuroendocrine tumours, except insulinomas, SRS has a high sensitivity of up to 86% [14, 17, 25] but may suffer from up to 12% false positive results. In a study by Gibril et al. in 122 patients the results of SRS changed management in 47% of patients [25]. Comparing helical CT and SRS Kumbasar et al. found similar sensitivity and accuracy in detecting primary neuroendocrine tumour for both of the methods [26].
As neuroendocrine tumours may occur as tiny multiple endocrine neoplasia (MEN) [27] standard imaging techniques such as US, CT and MRI tend to be less reliable in their detection. For this reason the use of endoscopic ultrasound for the localisation of these tumours within the pancreas has been evaluated since the very early days of this technique (Table 2). It has increasingly become a routine procedure in the diagnostic work-up of neuroendocrine tumours.

An early study by Roesch et al. [28] included 37 patients with 39 neuroendocrine tumours measuring 0.5-2.5 cm (mean 1.5 cm). None of the lesions was detected on US and CT. Using EUS 82% of the tumours could be localised. In 22 of these patients angiography was also performed but was able to find the tumour in only 27% [28].
Palazzo et al. [29] demonstrated the accuracy for localising small endocrine pancreatic tumours. Thirteen suspected insulinomas up to 15 mm (in 79% of lesions) and 17 gastrinomas were imaged by US, CT and EUS. Accuracy for EUS was 79%, US 7% and CT 14% [29]. Zimmer et al. performed EUS in 20 patients, 10 of which had gastrinomas with a mean diameter of 2.1 cm [14]. They were able to detect 79% of the gastrinomas. In the same group of patients SRS detected 86%, and 29% were detected with US, CT and MRI. The other 10 patients had insulinomas with a mean diameter of 1.5 cm. EUS was able to localise 93% of these tumours, while SRS identified only 14%, CT 21% and US and MRI were able to detect only 7% [14]. A similarly encouraging result especially in the localisation of insulinomas was reported by De Angelis et al. in 1999 [22]. Eleven out of 12 insulinomas were detected by EUS (91.6%) with an overall sensitivity for various pancreatic neuroendocrine lesions of 87%. In the same group of patients US was able to localise only 17% of the tumours, CT 30.4%, MRI 25%, angiography 26.5% and SRS 15.4% [22]. The same group evaluated unselected PNET of 14 patients and compared the results to surgery [30]. The overall EUS ability to localise the endocrine pancreatic tumours was 83%, while US achieved 11%, CT 28%, MRI 27%, angiography 29% and SRS 11% within the same group of patients [30]. Out of 36 gastrinomas, Anderson et al. [21] have been able to localise 100% correctly, while this was possible in 88% of 36 insulinomas. Angiography was performed in 14 of those patients and detected 44% of the lesions [21]. Gress et al. [31] were able to tattoo an otherwise undetected insulinoma with India ink under EUS guidance using a 22 gauge needle, which is mainly used for fine-needle aspiration. At laparotomy, performed 5 hr later, the surgeons were able to readily recognise the tattooed area and tumour for resection [31].
In addition to localising these tumours EUS may be used to obtain a tissue diagnosis. This may be particularly useful with nonfunctioning neuroendocrine lesions, which are otherwise difficult to diagnose preoperatively. Especially if the lesions are small, knowledge of the neuroendocrine nature of the tumour might lead to enucleation rather than extended pancreatic resection [32]. EUS with fine needle aspiration (EUS-FNA) can provide cytology diagnosis of most of the pancreatic masses, even if they are as small as 5-8 mm [32]. Neuroendocrine tumours, however, make up only a small proportion of focal pancreatic lesions detected on EUS. In a large single centre study Fritscher-Ravens et al. diagnosed only 5 neuroendocrine tumours out of a total of 200 patients with focal pancreatic lesions of unknown origin using EUS-FNA [33]. Voss et al. [34] biopsied 15 neuroendocrine tumours out of a total of 99 patients. It is not clear how many of these tumours were known to be neuroendocrine hormone producing and how many nonfunctioning prior to EUS. They found the results of EUS-FNA for neuroendocrine masses less accurate (47%) than for adenocarcinomas (81%) [34].
In a multicentre study it was shown, that the accuracy of EUS in the detection of PNET was significantly increased with the addition of EUS-FNA [35]. In some cases it may be beneficial to have additional histology proof of the suspected nature of the tumour although biochemical tests have shown the presence of neuroendocrine hormones. On ultrasound some of these tumours may resemble a peripancreatic node (Figure 5) as they may be attached to the pancreas just by a small vascular stalk [21, 36]. EUS-FNA can help to prove the nature of these lesions. Gines et al. [36] retrospectively analysed 10 such patients who underwent EUS-FNA for tissue proof. Sensitivity was 90% with 90% accuracy. There were no false positive results [36].
The cost effectiveness of EUS compared to other imaging modalities has also been accessed. Bansal et al. [37] compared 26 patients who underwent EUS first with 36 patients investigated before EUS became available to this hospital. The EUS group had significantly reduced charges for preoperative localisation of the tumours in relation to the non-EUS group (2,620 US$ vs. 4,846 US$). The major cost contributor in the non-EUS group was for angiography or venous sampling procedures [37]. The overall advantages of endoscopic ultrasound are that it is safe and minimally invasive. It does not require general anaesthesia or hospitalisation. The complication rate including that of fine needle aspiration is extremely low. One of the shortcomings of EUS and EUS-FNA is that the technique is time consuming, technically demanding, potentially difficult and highly operator dependent. An essential prerequisite for performing this technique - especially in the area of the pancreas - is familiarity with and training in the use of radial and/or linear array echoendoscopy. With its limited endoscopic view and its 2-3 cm long tip on top of the endoscope, the endoscope is not easy to manoeuvre. As neuroendocrine tumours of the pancreas can be very small it may be difficult for physicians less experienced in endoscopic ultrasound to detect them, resulting in futile examinations.
Recent studies demonstrated that operator experience was the essential factor in EUSFNA sensitivity and accuracy [38, 39]. To enhance the chances of success in the detection of these lesions it may be necessary to decide for every hospital individually which imaging modality should be used on the basis of the available imaging techniques and the expertise of the individuals. EUS expertise, so far, is not readily available even throughout the western world and training opportunities are still limited, even if interested physicians would be willing to invest time and effort [39].
Despite the long learning curve for examiners and other adversities, the effectiveness of endoscopic ultrasound for the location and diagnosis of neuroendocrine tumours and locoregional lymph node metastases has been well proven as has it’s cost effectiveness. If liver lesions are present it may even be able to detect those, if located in parts of the liver visible on EUS. If there is doubt, EUS-FNA can provide a cytological diagnosis of these lesions and demonstrate their neuroendocrine nature. Distant metastases, however, are not accessible with this technique. For that reason, some studies suggest, that EUS in combination with SRS might be more effective than either of these methods alone [25, 40].
SRS has the advantage of being able to examine the whole of the body and therefore might detect multifocal disease. EUS on the other hand might detect the tumour itself and clarify false positive SRS results in the duodenum, the pancreas or in the peripancreatic region.
Gastrointestinal neuroendocrine tumours are rare neoplasms that cause classic clinical syndromes because of the excess secretion of specific gastrointestinal hormones. The two most important tumours clinically are insulinomas and gastrinomas. In the management of these patients CT and ultrasound are the most common initial investigations but have limited sensitivity. Angiography, venous sampling methods and somatostatin receptor scintigraphy are often employed as second line investigations but with variable success. The increased cost and invasiveness need to be considered. SRS appears to be a valuable imaging technique for the detection of gastrinomas and metastases from other neuroendocrine tumours and has the advantage of being able to screen the whole body.
EUS has emerged as an accurate, highly sensitive and cost effective modality for the preoperative localisation of pancreatic neuroendocrine tumours. The use of the technique for multiple endocrine tumours and for distant metastases is, however, limited. The combination of EUS and SRS may be able to provide most of the information required preoperatively and seems to be the optimal approach available to date.