- (2010) Volume 11, Issue 6
Everson LA Artifon, Jonas Takada, Luciano Okawa, Eduardo GH Moura, Paulo Sakai
Gastrointestinal Endoscopy Unit, University of São Paulo. São Paulo, Brazil
Received July 29th, 2010 - Accepted September 16th, 2010
Context Endoscopic retrograde cholangiopancreatography (ERCP) is the procedure of choice for biliary decompression in patients with unresectable pancreatic cancer. However, it may be unsuccessful in 3 to 10% of cases. When ERCP is unsuccessful, the usual alternatives are percutaneous transhepatic biliary drainage or surgery. Recently, several authors have reported the use of EUS-guided biliary drainage in patients with malignant biliary obstructions, with acceptable success and complication rates. We describe three cases of unresectable pancreatic cancer associated with obstructive jaundice, treated by EUS-guided biliary drainage. Case report Three patients with unresectable pancreatic cancer, associated with obstructive jaundice, were included. ERCP was unsuccessful because of complete tumor obstruction of the distal common bile duct and papilla invasion. An EUS-guided rendezvous maneuver was attempted, without success. Then, EUS-guided choledochoduodenostomy, with a partially covered self-expanding metal stent, was performed in the same procedure. There were no early complications and the procedure was also clinically effective in relieving jaundice in all cases. Conclusions EUS-guided biliary drainage is a feasible alternative to percutaneous transhepatic biliary drainage or surgery in unresectable pancreatic cancer with obstructive jaundice when ERCP fails. However, the development of new specific instruments and studies comparing this procedure with percutaneous transhepatic biliary drainage and surgery are needed.
Cholangiopancreatography, Endoscopic Retrograde; Endosonography; Pancreatic Neoplasms
Endoscopic transpapillary biliary drainage is the procedure of choice for biliary decompression in patients with unresectable pancreatic cancer associated with obstructive jaundice [1, 2, 3, 4]. However, ERCP failure can occur in 3 to 10% of cases [1, 2, 4], even in experienced hands. This failure is related to operator inexperience, anatomic variation, tumor extension, prior surgery or incomplete drainage [1, 2, 3, 4].
The alternatives for biliary drainage in unsuccessful ERCP cases include precut sphincterotomy when a pathologic lesion is suspected, a second-attempt ERCP, percutaneous transhepatic drainage or surgery [1, 3, 5, 6]. However, percutaneous transhepatic biliary drainage has a complication rate of up to 30%, including biliary fistula, peritonitis, empyema, hematoma and liver abscesses [1, 7]. Furthermore, if subsequent internal drainage cannot be achieved, the patients would have to accept long-term external biliary drainage which can be uncomfortable and is non physiological, with significant impairment of quality of life [1]. Surgery offers long-term patency but is associated with increased morbidity and mortality [7]. Several studies have reported the use of EUS-guided biliary drainage in patients with malignant biliary obstructions, allowing for biliodigestive anastomosis with acceptable success and complication rates [4, 7]. We herein describe our experience with three cases of unresectable pancreatic cancer associated with obstructive jaundice which were treated by EUSguided biliary drainage.
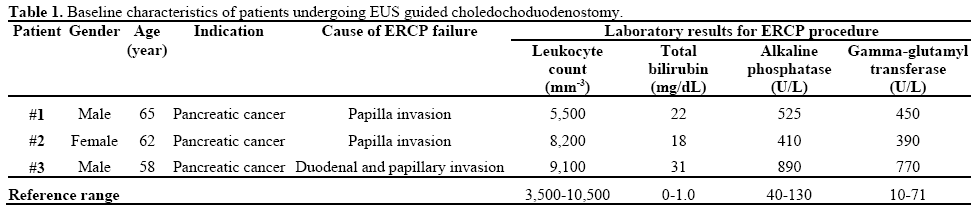
EUS-guided choledochoduodenostomy was performed in the first portion of the duodenum in three patients with pancreatic adenocarcinoma and obstructive jaundice and no signs of cholangitis (Table 1). ERCP was attempted but unsuccessful due to complete obstruction of the distal common bile duct by the tumor and papilla invasion.
The concept of EUS-guided biliary drainage was discussed with the families as an alternative to avoid percutaneous transhepatic biliary drainage or surgery. Informed consent was obtained in all cases and was approved by the Research Ethic Committee at University of São Paulo (CAPPesq). EUS-guided biliary drainage was performed by an experienced endoscopist, under conscious sedation, using a combination of intravenous midazolam, fentanyl and propofol. It was a procedure involving an obstructed biliary system, and a prophylactic antibiotic (ciprofloxacin 400 mg i.v.) was used, only in the beginning of the procedure.
The common bile duct was visualized using a linear echoendoscope (GFUCT160, Olympus, Tokyo, Japan). Color Doppler US was used to identify the vascular anatomy. The dilated bile duct was punctured with a 19 gauge FNA needle (EUSN-19-T, Cook Endoscopy, Winston-Salem, NC, USA). The puncture position was chosen based on EUS evaluation, at the common bile duct above the tumor, through the distal part of the duodenal bulb (Figures 1 and 2). To confirm successful biliary access, the bile was aspirated and iodine contrast was injected under fluoroscopy to demonstrate biliary opacification (Figure 3).
A 0.035 inch guidewire was introduced through the EUS needle, using fluoroscopy. An attempt was made to pass the guidewire through the lesion to reach the duodenum as a “rendezvous” maneuver, without success.
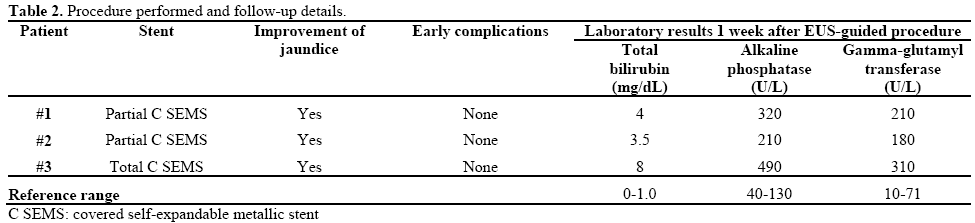
Then, the needle was withdrawn and a wire-guided needle knife (KD-441Q, Olympus, Tokyo, Japan) was used to increase the orifice in the duodenal wall, using coagulation power to avoid bleeding. Then, a partially covered self-expandable metallic stent (60x10 mm; WallFlex®, Boston Scientific, Natick, MA, USA) was passed over the guide, through the choledochoduodenal fistula, without any dilatation procedure (Figure 4). There were no early complications and the procedure was also clinically effective in relieving jaundice in all cases (Table 2). The patients subsequently underwent palliative chemotherapy. The follow-up will be carried out as long as the patient remains alive.
For more than 20 years, EUS has continued to evolve from a purely diagnostic to a therapeutic procedure [3, 4, 6, 7]. The ability to place a needle within the imaging plane of the ultrasound endoscope allows the expansion of the potential applications of this technique [7], Wiersema et al. first performed EUSguided cholangiography to guide ERCP in 7 patients in 1996 [6].
An EUS rendezvous to obtain bile duct access for conventional ERCP was first reported in 2004, by Mallery et al. [8]. This technique is used solely to puncture the obstructed bile duct and pass a guide wire antegrade through the native papilla to allow subsequent ERCP. EUS-guided biliary rendezvous can be done through a transduodenal route to the common bile duct or through a transgastric route to the intrahepatic ducts. The technical success rate is about 80% [9]. The complications are uncommon, but duodenal perforation and fluid leaks have been described [9]. Advantages of this procedure include achievement of biliary drainage at a single session by using conventional ERCP techniques, and possibly fewer complications than other EUS transluminal drainage approaches. However, a limitation of this technique is that it can be attempted only in patients in whom the papilla is endoscopically accessible. In our cases, we tried to pass the guidewire through the distal lesion to reach the duodenum and complete an ERCP as a rendezvous maneuver. However, it was not possible because the guidewire did not reach the duodenum, even after several attempts. EUS-guided biliary drainage was then performed.
In 2001, Giovannini et al. performed the first choledochoduodenal fistula under EUS guidance in a patient with pancreatic cancer using a needle knife followed by transduodenal stenting [10]. Ang et al. reported two cases with unresectable pancreatic cancer and the obstructed biliary system was successfully decompressed by the creation of a choledochoduodenal fistula and transduodenal biliary stent [1].
In 2003, Giovannini et al. described the first EUSguided hepaticogastrostomy, in a patient with proximal metastatic biliary obstruction [11]. Other authors have also reported successful outcomes of this technique in which an anastomosis was created between the dilated left intrahepatic biliary system and the cardia or the lesser curve of the stomach [12, 13].
Shami and Kahaleh et al. [4, 14] recommend intrahepatic access to the biliary system because it seems to be safer than the extrahepatic approach. However, other studies have shown that the extrahepatic approach may also be feasible and safe [15, 16, 17]. In 2007, Artifon et al. [2] and Bories et al. [12] described the successful use of a partially covered metallic stent for EUS-guided biliary drainage during hepaticogastrostomy [16].
In our cases, a 19 gauge FNA needle was used to perform the initial transduodenal common bile duct puncture as reported above. Then we used a 0.035 guide wire through the EUS needle into the common bile duct, followed by the insertion of needle-knife catheter (7.8 Fr of diameter) over the guide wire to enlarge the orifice in the duodenal wall, thereby avoiding bleeding and additional dilatation at the puncture site. This step could be carried out with other specific materials, such as a cystotome. However, this needle was not available and we felt that the wireguided needle knife could provide an adequate opening for the passage of the metal stent, with little risk of bleeding.
In 2003, Burmester et al. [3] described a one-step method using a new device consisting of a 19 gauge fistulotome with a 0.25 inch guidewire, a pusher tube and an 8.5 Fr plastic stent fixed with a 3.0 nylon suture. This method of direct puncture of an extrahepatic or an intrahepatic duct could reduce the risk of guidewire dislocation during instrument change which must be done when the two-step method is used [3]. However, additional studies with this device are needed.
EUS-guided biliary drainage has many advantages over percutaneous transhepatic biliary drainage [1, 3, 4, 18]. The proximity of the transducer to the bile duct during EUS is the major advantage [4, 19]. Even in patients who have undergone a total gastrectomy or a partial gastrectomy with a Billroth II reconstruction, EUS can reveal the etiology of extrahepatic cholestasis which may not be possible with ERCP [1, 3, 4, 6, 20]. Other advantages include puncture of the biliary tree with color Doppler information to avoid vascular injury, the lack of ascites in the interventional field and the lack of an external tube, improving the quality of life of the patients [1, 21].
Choledochoduodenostomy can prevent clogging and tumor ingrowth and/or overgrowth because it creates a fistula far from the obstructing tumor [17, 21]. Furthermore, the short access route between the duodenal bulb and the bile duct provides good stabilization of the echoendoscope, the avoidance of major vascular structures and orientation of the puncture towards the hepatic hilum.
EUS-guided choledochoduodenostomy for malignant biliary obstruction has been shown to be an effective alternative to percutaneous transhepatic biliary drainage or surgery when ERCP fails. Increasing experience and improvement of the technique and equipment will probably improve the safety of the procedure. Studies comparing EUS-guided biliary drainage and percutaneous transhepatic biliary drainage and surgery are needed.
The authors have no potential conflict of interest