- (2010) Volume 11, Issue 2
Titus Thomas1, James Bebb1, Jayan Mannath1, Krish Ragunath1, Phillip V Kaye2, Guruprasad P Aithal1
1Biomedical Research Unit and 2Department of Histopathology, Nottingham Digestive Diseases Centre and Nottingham University Hospitals NHS Trust. Nottingham, United Kingdom
Received September 2nd, 2009 - Accepted February 2nd, 2010
Context Fluid analysis obtained by EUS guided FNA is used to aid in diagnosis and management of cystic lesions in the pancreas. Complementing fluid aspiration with brushing of cyst wall may increase the cellular yield. Objective To compare cellular yield of pancreatic cyst FNA with and without wall brushing. Design Comparative study. Setting Tertiary referral centre. Patients Fifty-one patients with cystic pancreatic lesions referred for EUS-guided aspiration/sampling were included (median age 69 years; interquartile range: 49-77 years). Main outcome measures Comparing adequacy of cellular yield between EUS-guided aspiration alone vs. EUS-guided aspiration and cyst wall brushing. Intervention EUS-guided FNA and/or wall brushing (aspiration only: No. 27; brushing: No. 24). Results There was no significant difference in age (P=0.496) cyst size (P=0.084) or cyst location (P=0.227) between groups. Overall 29.5%; (15/51) of samples were acellular/insufficient with no significant difference between the two groups (22.2% in the aspiration only group vs. 37.5% in the brushing group; P=0.356). The remaining samples were adequate for cytological evaluation (77.8% vs. 62.5%; aspiration only vs. brushing groups). Seventeen cases were neoplastic (8 benign, 9 malignant). The diagnostic accuracy was 61.9% and 55.0% in aspiration only and brushing groups, respectively. Two out of 4 (50.0%) patents were diagnosed as having cancer in the brushings group compared to 1/5 (20.0%) in the FNA only group (P=0.524). Limitations Non-randomised series. Conclusions The cellular yield was similar in FNA and brushing group. Greater proportion of patients with malignant cystic pancreatic lesions diagnosed by EUS sampling was in the brushing group, but this did not reach statistical significance.
Biopsy, Fine-Needle; Endosonography, Pancreatic Cyst
IQR: interquartile range
Up to 10% of cystic lesions in the pancreas are cystic tumours [1]. About 75% of cystic tumours are benign (serous and mucinous) cystadenomas or cystadenocarcinomas [2] and these in conjunction with intraductal papillary mucinous neoplasms (IPMNs) account for the three most commonly encountered cystic tumours of the pancreas [3]. Accurate diagnosis of benign cystic neoplasms is vitally important due to the differential malignant potential of these lesions and the need for curative surgery in selected cases of IPMN’s and mucinous cystadenomas. Although CT scan may help in characterisation of these lesions based on wall calcification, septa, mural nodules and features of pancreatitis, further characterisation of these lesions is essential before major pancreatic surgery [4, 5]. Endoscopic ultrasound can often be used to provide additional morphological information and also to perform fine needle aspiration cytology of exfoliated cells for cytological diagnosis [6]. In addition, biochemical analysis of cellular fluid for CEA, CA 19- 9 and amylase may help further differentiate these lesions to a certain extent [7]. Although the specificity is good the sensitivity for FNA cytology remains low due to poor cellular yield [8]. Complementing fluid aspiration with brushing of cyst wall may increase the cellular yield.
The primary aim of the study was to determine and compare the cellular yield of pancreatic cyst FNA cytology with that of cyst wall brushing. The secondary aims were to determine and compare the sensitivity and diagnostic accuracy of pancreatic cyst FNA cytology with EUS-guided pancreatic cyst wall brushing.
Patients
Patients referred for EUS guided sampling of pancreatic cystic lesions between May 2002 and January 2008 in a large tertiary referral centre with a catchment population for referral covering at least three surrounding districts (population of over 3 million in total) as a part of their clinical management were included. The EUS-guided echobrush is being used in our centre for cyst wall sampling since August 2005. Patients were divided into the ‘aspiration only’ group and ‘brushing’ group (cyst aspiration plus wall brushing). All patients had CT scan prior to EUS evaluation.
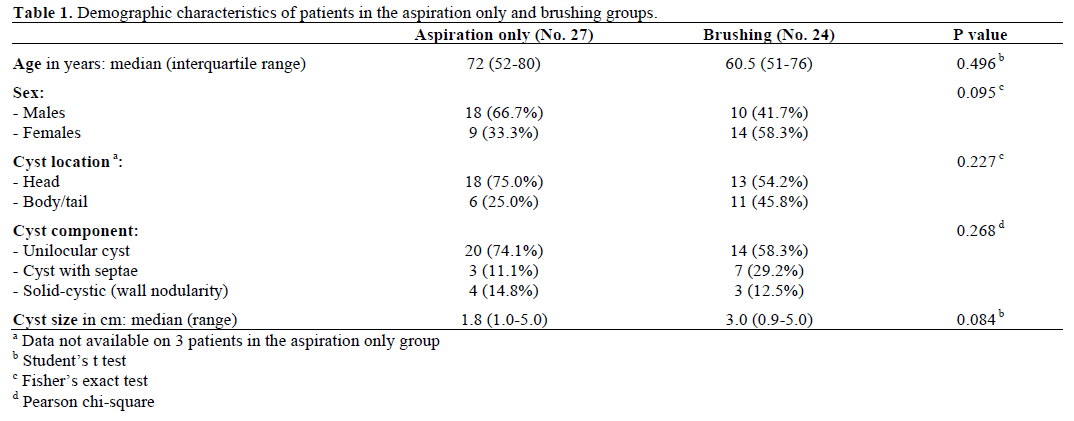
Overall 51 patients (28 males and 23 females) with a median age of 67 years (interquartile range, IQR: 52-77 years) were included. Twenty-seven were in the aspiration only group and 24 in the brushing group. Table 1 compares the demographic features and cyst characteristics of both groups. Overall the lesions were located in the head/uncinate process in 31 (60.8%) patients. The maximum cyst size ranged from 0.9 to 5.0 cm (median: 2.4 cm). One to four passes were made (median: 1). In 15 patients (29.4%) passes were made from the first part of duodenum and the remaining from the stomach. There was no significant difference in age (P=0.496), cyst location (P=0.227) or cyst size (P=0.084) between the two groups. Thirteen patients (25.5%; aspiration only group: 7, 26.0%; brushing group: 6, 25.0%; P=1.000) had an established clinical diagnosis of chronic pancreatitis (based on history and EUS findings) prior to EUS-sampling. Forty-four patients (86.3%) had cystic lesion identified by CT or abdominal ultrasound while the other 7 patients had missing data because they were referred from outside the region. Five patients (9.8%) had additional sampling either prior to or at the same time of the EUS procedure (all 5 patients were in the brushing group: 2 patients had ERCP and brush cytology as well as EUS-FNA prior to cyst aspiration only and brushing and 3 patients had EUS-trucut biopsy at the same time as the EUS-guided brushing)
Data Collection
Demographics, pre-EUS investigations and procedures, details of EUS procedure, post-procedure complications, histological diagnosis and follow-up data was collected prospectively from endoscopy, histopathology, information technology data base (Nottingham information system, NoTis (https://www.nuh.nhs.uk/ictservices/drs-induction/ NotISDocs.aspx) and case notes for the cohort sampled using both echobrush and fine needle aspiration. This was then compared to data collected retrospectively form patients who had only fine needle aspiration for sampling the cystic lesions.
EUS Procedure and Cyst Wall Brushing
Patients were routinely given intravenous antibiotics (ciprofloxacin 400 mg) prior to puncturing the cyst and oral ciprofloxacin 500 mg bid for 3 days after the procedure.
All patients had platelet count and coagulation profile checked and corrected if needed prior to the procedure. Procedures were done under intravenous sedation with diazepam and pethidine or midazolam and fentanyl. Cyst sampling was done by two operators with a combined experience of over 1,000 linear EUS procedures (GPA and KR). The lesion was identified and punctured using a 19 G needle using curvilinear echoendoscope (GF-UCT240-AL5, Olympus KeyMed, Essex, United Kingdom) and 50% of the cyst content was initially aspirated. The echobrush (Cook Medical, Limerick, Ireland, United Kingdom) was then passed through the handle and advanced through the needle till the whole brush could be visualised in the cyst. The wall of the cyst was then brushed by to and fro movement of the brush tip by moving the shaft of the needle at the handle. The opposite wall of the cyst was then visualised by moving the handle of the scope sideways and the brushing repeated at least four times (Figure 1). The brush was targeted if septae or nodules were present on the cyst wall. The brush was pulled back into the needle tip prior to removing the needle from the cyst and the needle apparatus with echobrush was withdrawn as a whole. The cyst was then aspirated to dryness using either a 19 G or 22 G needle. In patients where only FNA was done the cyst was punctured and aspirated using a 22 G needle.
Figure 1. Linear endoscopic ultrasound showing EUS-guided brushing of a cystic pancreatic lesion. a. EUS-FNA 19 G needle entering a cystic lesion in the head of the pancreas. b. The cyst being aspirated. c. The cyst wall being brushed by echobrush introduced through the needle. d. The cyst aspirated to dryness after cyst wall brushing.
Histological Evaluation
Two slide smears were then made with the brush, air dried and fixed in alcohol. The brush was then detached using cutting pliers and sent for cytological evaluation. The specimens were not evaluated by an on site cytopathologist. The cytology brush smears were evaluated separately from the fluid aspirates postbrushing. The cellularity of the samples was classified as adequate, insufficient for analysis or inadequate/acellular. Satisfactory specimens are those that were adequate for cytological evaluation. Cytological diagnosis was reported in histological terms when possible or classified into diagnostic categories conventionally used in non-gynaecological cytopathology as the following: positive for malignancy, negative for malignancy, atypical or indeterminate, suspicious and unsatisfactory [9]. All specimens were analysed by a single expert histopathologist (PVK).
The final diagnosis was based on operative histology, death from malignant disease, or absence of disease progression on prolonged follow-up of at least 12 months. Patients with diagnosis other than cancer were considered to be true positives if they were mucinous tumours with malignant potential confirmed by surgical histology (mucinous cystadenoma and IPMNs). Patients were considered true negatives if cancer/IPMN was not established at the end of 12- month follow-up. For true negatives differentiation between mucinous or non-mucinous cysts was not attempted but these patients were grouped under benign cysts. These patients had follow-up CT scans to monitor cyst size and change in morphology. Patients without histological confirmation (either by EUS guided trucut biopsies, laparoscopic biopsy or surgical histology), as well as those lost on follow-up or with follow-up of less than 12 months were considered true negatives and were excluded form the sensitivity analysis. Technical failures and samples insufficient for cytological evaluation were considered false negatives even if the final diagnosis was benign.
Written informed consent was obtained from all patients prior to the procedure. The study protocol conforms to the ethical guidelines of the World Medical association Declaration of Helsinki- Ethical Principles for Medical Research Involving Human Subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004. All procedures were done as a part of patient care and no extra tests or procedures were done as a part of the study.
Data are reported as frequencies, median values, ranges, and interquartile ranges (IQRs). The Fisher’s exact, the Pearson chi-square, and the Student’s t tests were used as appropriate to compare the two groups. Two-tailed P values than 0.05 were considered statistically significant. The statistical package used was Arcus QuickStat statistical software [10].
Cellular Yield, Sensitivity and Diagnostic Accuracy in Both Groups
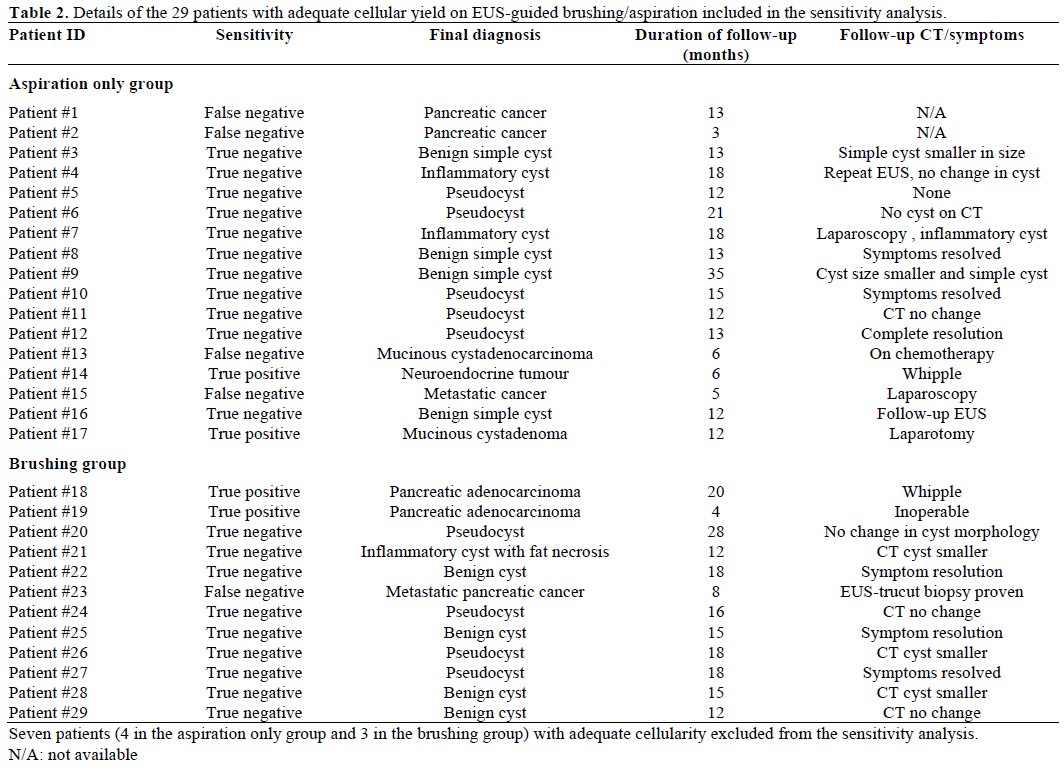
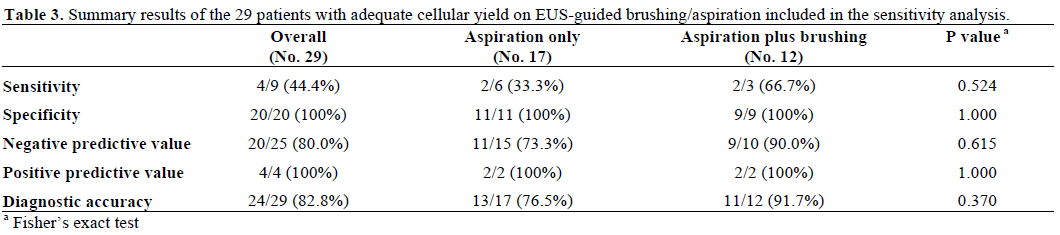
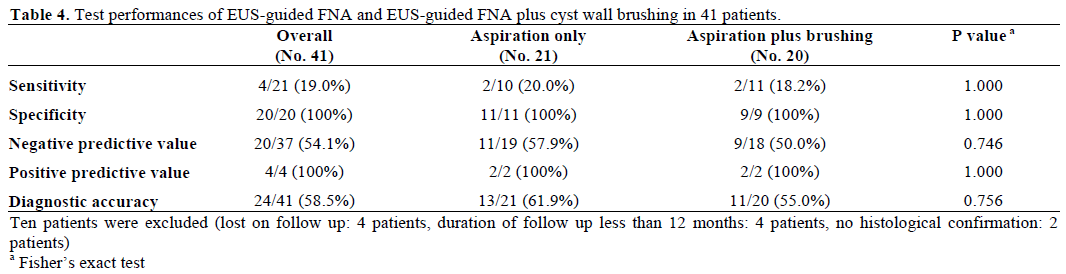
Overall the cellular yield was adequate in 36/51 (70.6%; aspiration only vs. brushing: 21/27 vs. 15/24, 77.8% vs. 62.5%; P=0.356), and acellular/insufficient for analysis in 15/51 (29.5%; aspiration only vs. brushing: 6/27 vs. 9/24, 22.2% vs. 37.5%). Seven of the 36 patients with adequate cellular yield were excluded from the sensitivity analysis (4 in the aspiration only group and 3 in the brushing group). The reasons for exclusion were as follows: no follow-up data (2 patients); follow-up duration less than 12 months (4 patients); no histological confirmation (1 patient). Table 2 shows the diagnosis of patients in both groups with adequate cellular yield and the results are summarized in Table 3. In 3/15 (20.0%) patients with acellular aspirate the final diagnosis was pseudocyst (based on history and fluid amylase). Table 4 shows the test performances in both groups. Ten patients were excluded from the sensitivity analysis (2 patients because of no histological confirmation, 4 patients lost on follow-up, and 4 patients with a follow-up period less than 12 months). All but one patient with adenocarcinoma had histological confirmation of diagnosis (considered true positive). He had C5 cytology and died within 4 months of diagnosis of metastatic disease. Overall 4/41 (9.8%) of patients were true positives, 17/41 (41.5%) false negatives and 20/41 (48.8%) true negatives at a median follow-up of 14 months (IQR: 12-18 months) giving an overall sensitivity, specificity, negative predictive value and diagnostic accuracy of 19.0%, 100%, 54.1% and 58.5%, respectively. Eleven out of 21 cases (52.4%) and 9/20 (45.0%) were true negatives in the aspiration only and brushing groups at a median follow-up of 12 and 15 months, respectively. There was no significant difference in sensitivity (aspiration only vs. brushing, 20.0% vs. 18.2%; P=1.000), diagnostic accuracy (aspiration only vs. brushing, 61.9% vs. 55.0%; P=0.756) or negative predictive value (aspiration only vs. brushing, 57.9% vs. 50.0%; P=0.746) between the two groups.
Comparing Neoplastic Lesions and Cancer in Both Groups
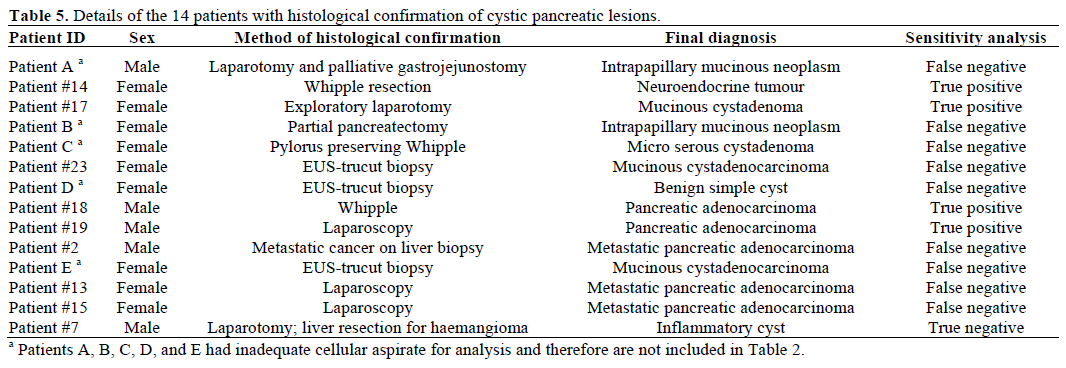
Overall, 17/51 (33.3%) cases were neoplastic (9 adenocarcinoma or neuroendocrine tumour; 8 mucinous cystadenoma or IPMT). The final diagnosis of adenocarcinoma or neuroendocrine tumour was made in 5/27 patients (18.5%) in the aspiration only group and 4/24 patients (16.7%) in the brushing group. Adenocarcinoma was diagnosed by EUS guided sampling in only 1/5 in the aspiration only group and 2/4 patients in the brushing group (20.0% vs. 50.0%, respectively; P=0.524). In 20/41 (48.8%) patients, malignancy was excluded. There were no immediate complications, hospitalisations or procedure related deaths. Table 5 shows all patients with histological confirmation of the diagnosis. None of the patients with adenocarcinoma had a curative resection either because of advanced inoperable disease or associated co-morbidities. Only four patients had diagnostic laparotomy or curative resection. One patient (Patient #14; aspiration only group) diagnosed with a neuroendocrine tumour (true positive) had a curative Whipple operation. Three other patients had a curative resection (two in the brushing group; one in the aspiration only group had diagnostic laparotomy, Patient #17) which showed IPMN in one patient and serous microcystic adenoma in the second and confirmed mucinous cystadenoma in the last patient. However 4/8 (50.0%) of patients with mucinous cystadenoma or IPMN and all but one patient with adenocarcinoma or neuroendocrine tumour had histological confirmation of the diagnosis.
Endoscopic ultrasound has emerged as a useful modality of investigation of pancreatic cystic lesion not only as it outlines the cyst morphology but also since it is the most sensitive test to evaluate the pancreatic parenchyma and ducts. EUS may be useful in differentiating cystic neoplasms from pseudocyst, but, does not reliably distinguish between serous and mucinous cystadenomas or IPMN. When faced with mucinous neoplastic cysts which have malignant potential, surgery or surveillance with serial imaging are considered as management options [11]. However, no single imaging finding reliably differentiates these two groups. Ahmad et al., showed that the inter-observer agreement of eight expert endosonographers evaluating 31 pancreatic cystic lesions to differentiate between neoplastic from non-neoplastic cyst was only considered to be ‘fair’ (kappa=0.24) [12]. Accuracy rates for diagnosis varied from 40% to 93% in the same study. Therefore EUS-FNA cytology in conjunction with cyst fluid biochemical analysis has been used in an attempt to establish a specific diagnosis when cystic pancreatic lesions are diagnosed [13].
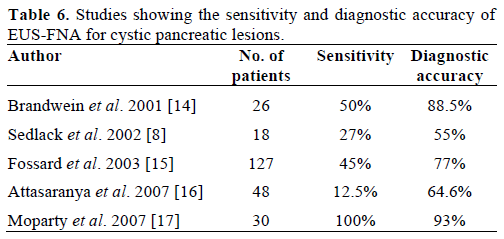
The sensitivity and diagnostic accuracy of EUS-FNA aspiration only group in our study were 20% and 62%, respectively. Several other studies have looked at the sensitivity and diagnostic accuracy of EUS-FNA cytology alone or in combination with cyst fluid biochemical markers to detect cancer and mucinous neoplasms with widely varied results. The sensitivity and diagnostic accuracy of EUS-FNA in these studies are summarised in Table 6 [8, 14, 15, 16, 17]. The varied results seen in these studies may be due to several factors: the differences in point prevalence of pancreatic cancer, chronic pancreatitis and cystic neoplasm in the selected population cohort; presence of on-site cytopathologist to evaluate the adequacy of the samples; the inter-observer variation in cytological evaluation of the samples and the definition used for true positives. Alsibai et al., evaluated the impact of cytology interpretation by an expert cytopathologist from 38/106 cystic pancreatic lesions and showed an improvement in the sensitivity and diagnostic accuracy of EUA-FNA [18] and a therapeutic impact on clinical practice in 39.5% of cases. The sensitivity of EUSFNA cytology alone in several studies has been universally poor (12.5-27%). In the largest prospective study by Frossard et al. [15], 127 patients with cystic pancreatic lesions were evaluated to assess the value of EUS-FNA (compared with the final diagnosis in 67 patients). EUS-FNA cytology alone correctly identified 77% of cases with only one cytopathologist analysing all the specimens. The low accuracy of our study may be partly explained by the absence of an on-site cytologist to evaluate the adequacy of the samples.
In a small pilot study on 10 patients Al-Haddad et al., [19] compared the cellularity of brush cytology specimens to conventional FNA and showed that in 7/10 patient’s cyst wall brushing provided superior specimens in terms of cellularity and diagnostic yield. Our study does not support these findings as we found no difference in adequacy of cellularity when the aspiration only group was compared to the group which had both aspiration and wall brushing (78% vs. 63%); therefore, insufficient or acellular specimens were similar in both groups (22% vs. 37%). One explanation for this difference may be the patient selection and the drawbacks of the retrospective nature of our analysis for the aspiration only group. In our cohort 12/51 patients (23.5%; 7 in the aspiration group and 5 in the brushings group) had pseudocysts as the final diagnosis and 3/15 (20.0%) patients with acellular/insufficient aspirate had pseudocysts (which usually show only macrophages and bile pigments on cytology) compared to the above mentioned pilot study where patients had either mucinous neoplasms or IPMNs. Secondly the imbalanced allocation of patients with regards to the location of the cysts within the pancreas may have contributed to difference in diagnostic yields. Although the cyst location was not significantly different between the two groups, a greater proportion of patients (75%) in the aspiration group had cysts in the pancreatic head compared to the brushings group (54%). The cysts in the head are technically difficult to brush since a 19 G needle has to be used compared to just aspiration using a 22 G needle. A greater proportion of patients with pancreatic adenocarcinoma were diagnosed in the brushing group (2/4, 50%) compared to the aspiration only group (1/5; 20%). Although the difference between the two groups was not statistically significant, this may have resulted from type II error due to small sample size. Small number of patients with cancer in each group precludes one from making firm conclusions regarding the superiority of wall brushing over cyst FNA only to diagnose malignancy. In the presence of solid components with cysts ideally a trucut biopsy or FNA should be attempted to sample the solid component of the cyst wall.
We acknowledge the limitations of the retrospective nature of our study. In the absence of a histological confirmation or a diagnostic laparoscopy it is difficult to establish or differentiate between mucinous and serous cystadenomas. Therefore we can only say that these patients had benign cysts. We do acknowledge that absence of cancer at 12 months is a soft end point for true negative patients but it would be impractical to perform major surgery on patients suspected to have benign disease. In our methodology we have included only patients with histological confirmation as true positives and therefore our sensitivity analysis is perhaps a true reflection of the sensitivity of EUSguided brush cytology of cystic pancreatic lesions.
Several other studies have reported a low incidence of major complications following FNA (pancreatitis, retroperitoneal bleed, cyst infection or haemorrhage into the cyst) [20, 21]. We did not find any major complication in the two groups. This confirms that in the hands of experienced operators and strict adherence to protocol including prophylactic antibiotics, both cyst puncture and brushing can be performed without increased risk of procedure related complications. There were no major complications in our study, which required over night stay in hospital or prolonged hospitalisation.
In conclusion the cellular yield was similar when brushing are done in addition to FNA compared to FNA only. The value of cyst wall brushing of pancreatic cystic lesions in addition to FNA appears to be modest although a greater proportion of patients with cancer were diagnosed in this group. A randomised controlled trial comparing the cellular yield for EUS-guided FNA only compared to FNA and cyst wall brushing for pancreatic cystic lesions is wanting.
The authors have no potential conflicts of interest