Original Article - (2018) Volume 19, Issue 1
1Department of Surgery, Catharina Hospital, Eindhoven, the Netherlands
2Department of Surgery, Cancer Center Amsterdam, Academic Medical Center Amsterdam, the
Netherlands
3Department of Surgery, Maastricht University Medical Center, Maastricht, the Netherlands
4Department of Surgery, Sint Antonius, Nieuwegein, the Netherlands
5NUTRIM School for Nutrition Toxicology and Metabolism, and GROW School for Oncology &
Developmental Biology, Maastricht, the Netherlands
6Department of Surgery, Onze Lieve Vrouwe Gasthuis, Amsterdam, the Netherlands
7Department of Gastroenterology, Maastricht University Medical Center, Maastricht, the Netherlands
8Department of Surgery, Medical Spectrum Twente, Enschede, the Netherlands
9Department of Surgery, Utrecht Medical Center, Utrecht, the Netherlands
10Department of Surgery, Universitätsklinikum Aachen, Aachen, Germany
11Department of Gastroenterology, Academic Medical Center Amsterdam, the Netherlands
12Department of Gastroenterology, Catharina Hospital, Eindhoven, the Netherlands
Received October 29th, 2017 - Accepted January 10th, 2018
Introduction A Dutch randomized trial showed that patients with obstructive jaundice due to periampullary tumors and a bilirubin below 250 μmol/l have a higher rate of complications after preoperative biliary drainage as compared to early surgery. Therefore, in the Netherlands the recommended treatment is early surgery without preoperative biliary drainage. This study investigated adherence to this recommendation. Methods A retrospective multicenter cohort study was performed in patients undergoing pancreatoduodenectomy for suspected malignancy in a 2-years period in seven Dutch high-volume centers. The proportion of and reasons for preoperative biliary drainage were studied. Results Pancreatoduodenectomy was performed in 609 patients, of whom 401 (66%) presented with preoperative jaundice. Of these, 245 patients had bilirubin levels below 250 μmol/l. Preoperative biliary drainage was performed in 165 (67%) of these patients. In the majority of patients, no medical reason justifying a preoperative biliary drainage could be retrieved from the medical charts (n=102, 62%). Preoperative biliary drainage was mostly performed in the hospital of diagnosis prior to referral to a pancreatic center (53%). After referral, the rate of preoperative biliary drainage varied considerably between pancreatic centers (13% - 58%, p<0.001). Conclusion In the Netherlands, more than half of the patients with obstructive jaundice still undergo preoperative biliary drainage prior to surgery in the Netherlands without an urgent medical reason. Given the negative influence of preoperative biliary drainage on outcome, this practice should be improved.
Pancreatoduodenectomy; Pancreatic Neoplasms
PBD preoperative biliary drainage; PD pancreatoduodenectomy
Most patients with a pancreatic and periampullary tumor present with obstructive jaundice. Elevated bilirubin levels are known to result in coagulation disorders, impaired cell-mediated immunity, impaired anastomotic healing and a higher risk for developing sepsis [1, 2, 3]. For these reasons, preoperative biliary drainage (PBD) to lower bilirubin levels prior to pancreatoduodenectomy (PD) was routinely used for decades to improve the patients’ general condition and to decrease the chance of postoperative morbidity and mortality. Since the PBD introduces a risk for complications by itself (e.g. post- ERCP pancreatitis and cholangitis), it has been a matter of debate whether PBD should be performed routinely or only on indication [4, 5, 6, 7, 8, 9, 10, 11]. In a Dutch randomized controlled multicenter trial which compared PBD with plastic endoprothesis to early surgery (within one week of diagnosis) [12], patients with obstructive jaundice in periampullary tumors with bilirubin levels below 250 μmol/l at the time of randomization appeared to have a significantly higher rate of complications after PBD. Therefore, in the Netherlands the preferred treatment in these patients is currently early surgery, preferably performed within one week after diagnoses and without PBD [13]. The aim of this study was to investigate the current practice of PBD in the Netherlands in patients operated for suspected periampullary tumors. Furthermore, we aimed to gain insight in the reasons for PBD prior to pancreatoduodenectomy.
Data Collection
Data were retrospectively collected from medical patient charts in seven Dutch high-volume (≥20 PDs for pancreatic cancer/year) centers (Academic Medical Center, Amsterdam; Catharina Cancer Institute, Eindhoven; Medical Spectrum Twente, Enschede; Maastricht University Medical Center, Maastricht; OLVG, Amsterdam; Sint Antonius Hospital, Nieuwegein; University Medical Center, Utrecht) and included patient characteristics, preoperative diagnostic and treatment procedures and tumor characteristics. The aim of the study was to determine the proportion of PBD in patients with obstructive jaundice with bilirubin levels lower than 250 μmol/l. Furthermore, documented reasons for drainage were collected as well as differences in the proportion of patients undergoing PBD in high volume centers.
Patient Selection
All patients undergoing PD for suspected-periampullary malignancy in 2013 and 2014 were analyzed. Patients undergoing PD in an emergency setting were excluded. Preoperative bilirubin levels were recorded and only patients presenting with jaundice and bilirubin levels between 21.0 μmol/l and 250 μmol/l were included for further analysis. The cut-off point of 250 μmol/l was chosen since only patients with bilirubin levels lower than 250 μmol/l were included in the RCT demonstrating the negative impact of pre-operative biliary drainage [12]. In patients with bilirubin levels above 250 μmol/l the decision whether or not to perform pre-operative drainage is still under debate.
Preoperative Biliary Drainage
PBD was defined as preoperative biliary drainage performed by endoscopic retrograde cholangiography (ERCP) or percutaneous transhepatic bile duct drainage (PTCD). The type of drainage and type of stent (plastic or metal) that was used was recorded.
Indications for PBD
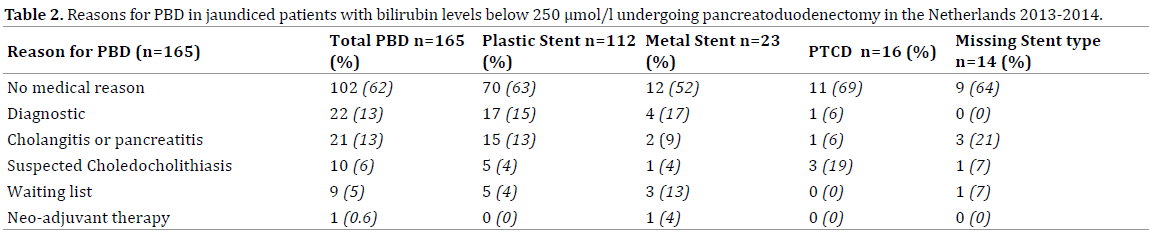
All hospital charts of patients undergoing PBD were scrutinized to identify the main reason of the treating physicians to perform a PBD. In total 6 categories could be identified: ‘diagnostic’ (if PBD was performed after contrast injection in the bile duct during ERCP for diagnostic reasons), “cholangitis / pancreatitis”, “suspicion of choledocholithiasis”, “waiting list” (if early surgery could not be provided in the expert center), “neo-adjuvant therapy” and “no medical reasons” (if none of the previous reasons were identified).
Ethics
All methods were carried out in accordance with the Helsinki Declaration of 1964 and later versions. The medical ethical committee was consulted and they concluded that according to the Dutch law on Medical Research in Humans and given the retrospective design, the current study did not require informed consent by involved patients. According to Good Clinical Practice, all patient derived data were anonymised.
Statistical Analysis
Statistic analyses were performed by using IBM SPSS statistics version 22. P-values lower than 0.05 were considered statistically significant.
In total, 609 patients underwent a PD for suspected pancreatic or periampullary cancer. Elevated bilirubin levels were present in 401 (66%) of these patients: below 250 μmol/l in 245 (61%) patients and above 250 μmol/l in 114 patients (28%). In 42 (11%) patients pre-operative bilirubin levels were missing and these patients were excluded from further analysis. The 245 jaundiced patients were further analysed. Baseline characteristics of the patients included in this study are presented in Table 1.
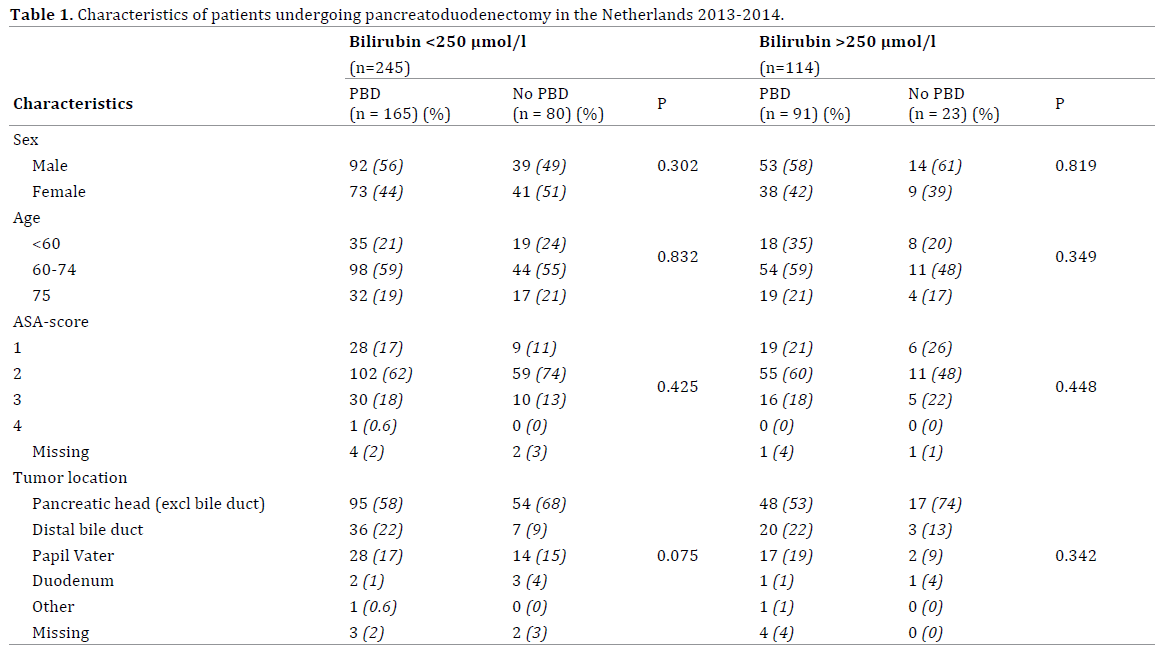
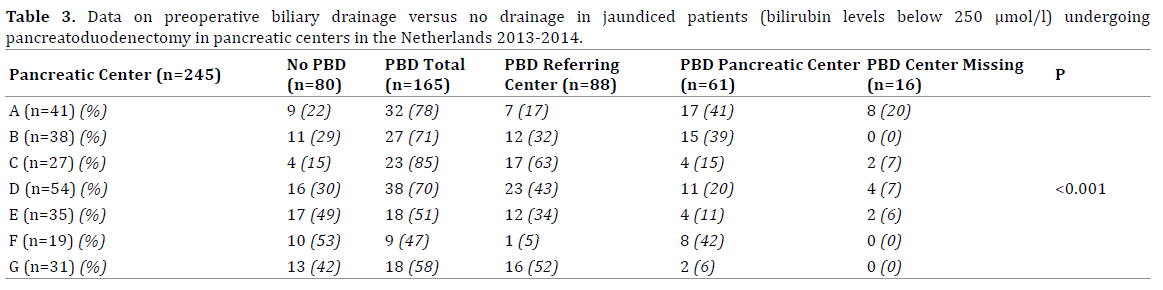
In 80 (33%) patients presenting with bilirubin levels below 250 μmol/l early surgery without PBD was performed. The remaining patients (n=165, 67%) underwent PBD prior to surgery. In the majority of patients, no medical reason to justify a PBD could be retrieved from the medical charts (n=102, 62%), Table 2. More than half of the stented patients were already stented in the hospital of diagnosis prior to referral to an expert center (n=88, 53%). Another 61 patients (37%) underwent PBD in the expert center after referral. The total proportion of PBD differed significantly between pancreatic centers (Table 3). Also the proportion of PBD performed after referral differed significantly between centers ranging from 13% to 58% (p<0.001) (Figure 1). PBD was most often performed by using a plastic stent (n=112, 68%).
The current study revealed that the vast majority of jaundiced patients with a pancreatic or periampullary cancer still undergo PBD prior to surgery in the Netherlands. In total 66% of patients with bilirubin levels <250 μmol/l underwent PBD and in most of them, no obvious medical reason to justify a PBD could be retrieved from the medical charts. In most patients, PBD was performed already before referral to a surgical unit in an expert center. However, a relevant proportion of patients underwent PBD prior to surgery in pancreatic centers after referral. The proportion of patients being stented in expert centers varied significantly between centers.
PBD has been subject of debate for many years. In 2010 Van der Gaag et al. published the results of the Dutch RCT that randomized patients with a bilirubin below 250 μmol/l to undergo PBD prior to surgery with plastic endoprothesis versus early surgery alone. Early surgery was defined, as ‘preferably within one week after randomization’. The reason to have a maximum waiting time in the early surgery group is that at randomization a maximum bilirubin level of 250 μmol/l was accepted and by waiting longer than a week, bilirubin levels may become to high for safe surgery. The RCT showed that a higher proportion of patients in the PBD-group suffered postoperative and drainage-related complications compared to patients in the early surgery group without PBD [12]. Severe complications occurred in 73.5% of the drainage group, compared to 39.4% the early surgery group [12]. This difference was mainly caused by post PBD complications such as cholangitis (26%). Since then, the recommendation in the Netherlands has been to perform early surgery without PBD whenever bilirubin levels are <250 μmol/l. This recommendation was accepted by all expert centers in the Netherlands, as they had all been participating in the RCT. However, adhering to this recommendation was anticipated to be challenging, as the interval of only one week between diagnosis and surgery may be difficult to achieve, especially as most patients are diagnosed in hospitals that do not perform surgery.
The current study investigated the daily clinical practice in the Netherlands 3-4 years after publication of the RCT. Rather surprisingly it was revealed that the majority of patients with bilirubin levels below 250 μmol/l still underwent PBD prior to surgery. In the majority of patients, no urgent medical reason could be retrieved from the medical charts. Although “waiting list / inability to operate within one week” was specifically mentioned in a small proportion of the patients, this may have played a major role in the patients in whom no specific medical reason was noted. In the RCT, the median time to surgery was already 9 days in the surgery group without PBD, hinting towards difficulties to perform surgery within one week [12].
The proportions of PBD after referral performed in pancreatic centers differed considerably between centers, varying between 13 and 58 percent for patients with bilirubin levels below 250 μmol/l. As referral to expert centers is based upon regional patterns, it is unlikely that case-mix variations within patients account for this difference in the amount of patients undergoing PBD. Therefore, it may well be assumed that this difference is caused by logistical hurdles within the expert centers themselves to realize surgical treatment within one week after referral.
If PBD by ERCP seems to be indicated, the type of stent that will be used, plastic vs. metal, should also be considered. The use of plastic stents has been one of the criticisms on the Dutch RCT [12]. PBD is still indicated in case of extreme hyperbilirubinemie, cholangitis, and the necessity for nutritional support or if it is not possible to perform early surgery because of logistical hurdles. Furthermore, PBD can be indicated in patients who undergo neo-adjuvant treatment [14]. A recent study by Tol et al. showed that the use of a covered metal stent instead of plastic stent reduces stent related complications (metal 6% vs. plastic 30%) and is costeffective in spite of the higher costs of the metal stent itself [14, 15, 16].
Although it might have been interesting, the current study does not describe postoperative complications after PBD as compared to early surgery since the retrospective design of this study does not allow a reliable collection of these data.
The current study should raise awareness in pancreatic centers that in spite of the well-investigated and published beneficial effects of early surgery without PBD, this is not yet achieved in the majority of patients. In the absence of obvious medical reasons in the charts to justify PBD, logistic problems to perform early surgery in the expert centers are the most likely explanation for this practice. Therefore, improving logistics within expert centers, as well as within the referring hospitals is needed to improve the outcome of these patients.
The authors thank all participating hospitals and the Dutch pancreatic cancer group.
This study was funded by a grant from the Dutch Cancer Society (KWF) (grant number 2013-649). The funding source had no role in the study design, data collection and analysis, the writing of the manuscript or the submission for publication.
M. Bakens initiated the study with D. Gouma and I. de Hingh. M. Bakens collected data, performed analyses and wrote the main manuscript and prepared figures and tables.
L. van Rijssen, V. van Woerden, M. Besselink D. Boerma, O. Busch. C. Dejong, M. Gerhards, J. van Hooft, Y. Keulemans, J. Klaase, M. Luyer, I. Molenaar, J. Oor, E. Schoon, W. Steen, D. Tseng, D. Gouma and I. de Hingh collected data in participating hospitals. Furthermore they improved the main manuscript text.
The authors declare no conflict of interest.