- (2006) Volume 7, Issue 4
Anil Bagul, Ajith K Siriwardena
Hepatobiliary Surgical Unit, Manchester Royal Infirmary. Manchester, United Kingdom
Received: 3 May 2006 Accepted: 22 May 2006
Context Classifications of chronic pancreatitis based on either histologic (Marseilles) or endoscopic (Cambridge) criteria are not widely used. Objective The present study describes the development and validation of a three-stage clinical categorical classification system for chronic pancreatitis. DesignPatients with a diagnosis of chronic pancreatitis (577.1: ICD-9) for 1993 were identified from records of the Hepatopancreaticobiliary service at a University hospital. Endoscopic or CT evidence of chronic pancreatitis were mandatory for inclusion. Patients Forty one patients met the criteria and were categorized according to a 3-stage system as mild, moderate or end-stage disease. Main outcome measure The clinical course over the subsequent decade was followed by chart review with re-categorization of stage at each review. Results At the outset of the study, 18 (44%) patients were categorised as having mild disease, 19 (46%) as moderate and 4 (10%) as end-stage. The number of patients with mild disease fell over the subsequent 5 years and at the end of the 10-year chart study period, no patients were categorised as mild. The number of patients with diabetes at the outset of the study period was 2 (5%). At two years this was 3 (7%), five years 10 (24%) and 10 years was 25 (61%). Conclusions These results show that the Manchester classification of chronic pancreatitis is both practical and feasible and now requires prospective evaluation and independent appraisal by other centres.
Pancreas; Pancreatitis; Pancreatitis, Chronic /classification
DPPHR: duodenumpreserving pancreatic head resection
In order to be of value, a disease classification system should be able to categorise stages which are clinically distinct and which have relevance to patient management. Further, the classification system should be relatively simple, reproducible and prospectively validated. Chronic pancreatitis, defined as a continuing inflammatory disease of the pancreas characterised by irreversible morphological changes which typically cause abdominal pain and/or permanent impairment of pancreatic function has proved resistant to categorization [1, 2]. The classification produced by the Marseilles international symposium in 1984 was invaluable in defining the disease and identifying various subtypes and clinical entities [1]. However, the classification is based on morphological characterisation and despite subsequent modification [3] is not widely applicable in clinical practice. The King’s College Cambridge classification of 1983 sought to address this and provide a clinically utilizable system based on endoscopic retrograde pancreatographic (ERCP) findings [4]. However, the Cambridge classification does not address the issues of pancreatic exocrine and endocrine function or the presence of extra-pancreatic complications.
More recent work on understanding the temporal course of chronic pancreatitis led to the Zurich international classification [5, 6] which has been used to define patient cohorts in recent studies of patients undergoing surgery for chronic pancreatitis [7, 8]. Limitations of the Zurich classification are that it is confined to patients with alcoholrelated chronic pancreatitis and does not provide prognostic or disease-stage related information [6]. In many patients, pancreatic endocrine and exocrine dysfunction occur relatively late in the disease [9] (although patients may have these features as index presentations) similarly, biliary stricture occurs later in the disease course [10]. Using an analogy similar to that in renal failure, our group recently reported the term “end-stage chronic pancreatitis” as describing those individuals with extra-pancreatic complications typical of long-standing disease such as distal biliary stricture and portal vein thrombosis together with varying degrees of exocrine and endocrine failure [11]. This disease descriptor categorises patients typically with long-standing disease but in whom the management options are limited as a result of extra-pancreatic complications. This concept of disease staging in chronic pancreatitis is not new and has previously been reported by Ramesh [12] and also by the Heidelberg group (H Friess personal communication).
The present study describes the development of a three-stage clinical categorical classification system for chronic pancreatitis. Prospective clinical evaluation is the gold standard for acceptance of the practical feasibility of any new classification system. Accepting that this takes a prolonged period of time, an alternative method used here as a compromise is to study the case notes of patients having their index presentation with chronic pancreatitis in 1993. Patients were categorised according to the disease descriptors defined in the three-stage clinical classification system and then their clinical course over the subsequent decade was followed by chart review.
Definition of Categorization System
A three stage system was selected to facilitate practical clinical use (Table 1). The terms “mild”, “moderate” and “end-stage” were selected to represent stages of disease progression. For each stage a series of obligatory criteria and a range of optional criteria were selected. For all stages it was stipulated that there must be radiological evidence of chronic pancreatitis: either crosssectional imaging by computed tomography or magnetic resonance scanning or pancreatic duct visualization by ERCP (magnetic resonance scanning was not routinely available in 1993 at the outset of this study).
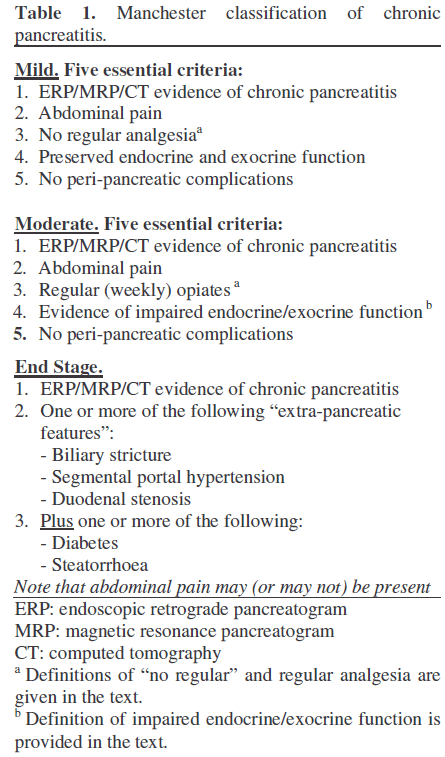
The definition of mild chronic pancreatitis can be problematic. Five essential criteria were required. These are listed in Table 1. Radiological evidence of chronic pancreatitis was mandatory. In an attempt to reflect the clinical entity of “mild” chronic pancreatitis, it was mandatory for this stage that there be no regular opiate intake (with regular being taken as weekly) and that there be no clinical evidence of impaired pancreatic exocrine or endocrine function or extra-pancreatic complications (duodenal stenosis, portal vein thrombosis and/or distal bile duct stricture).
Moderate chronic pancreatitis was simply defined as abdominal pain with radiological evidence of chronic pancreatitis without extra-pancreatic complications. To be categorized as moderate chronic pancreatitis, clinical evidence of impairment of either endocrine or exocrine function was required.
End-stage chronic pancreatitis was defined with more rigidity. There must be radiological evidence of chronic pancreatitis and at least one obligatory factor from a range of extrapancreatic complications plus one or more clinical factors to suggest end-stage pancreatic function: either steatorrhoea or diabetes mellitus. During the period of this study, glucose tolerance testing was utilized in assessing pancreatic endocrine function. Pancreatic exocrine function was assessed in some patients by measurement of urinary recovery of breakdown products of paraamino benzoic acid (PABA test). In recognition that all the extra-pancreatic complications described can occur during the immediate aftermath of severe acute pancreatitis, it was further stipulated that there must not be an antecedent history of an index attack of acute pancreatitis in the preceding 3 months (index being defined as a first-ever attack of pancreatitis). This stipulation does not therefore exclude those patients with endstage disease whose clinical course would manifest as relapsing episodes of pain (with or without hyperamylasemia).
A novel feature of this classification system that takes into recognition the fact that pain may not be the dominant symptom in longstanding disease is the categorization of abdominal pain as non-obligatory in end-stage chronic pancreatitis.
Study Design and Patient Population
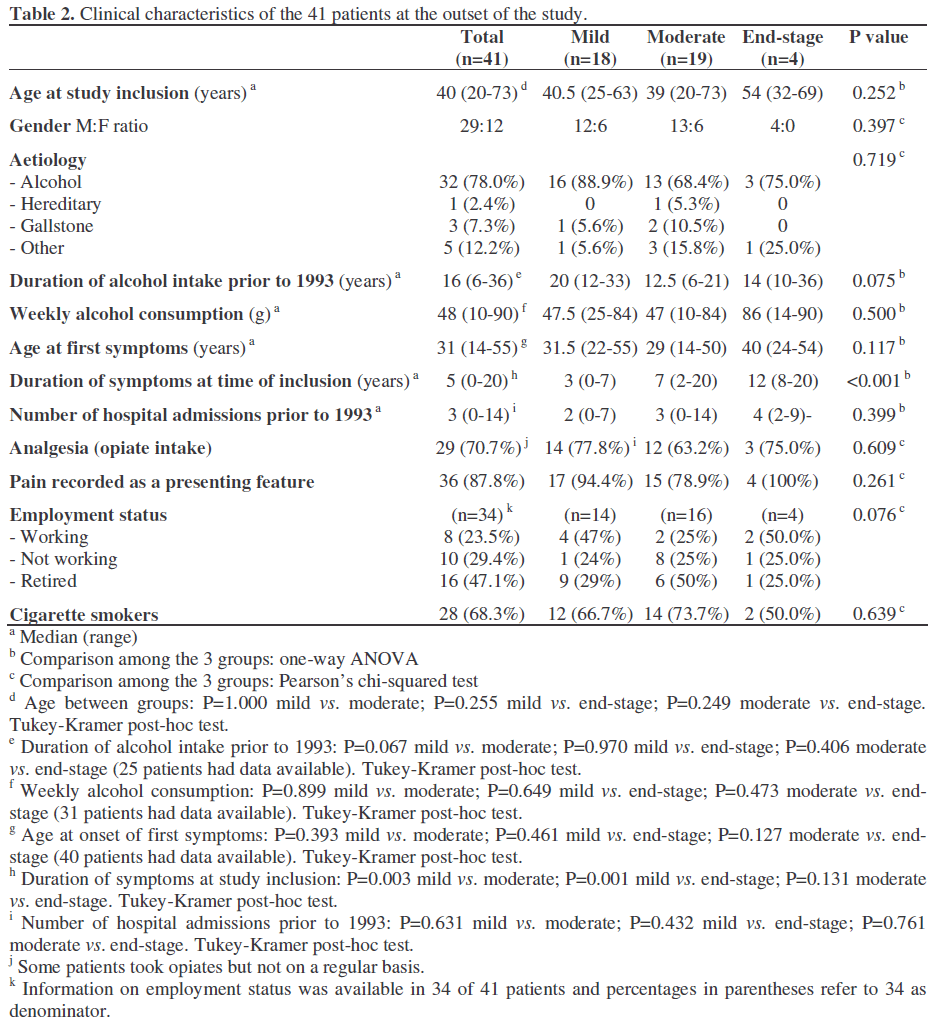
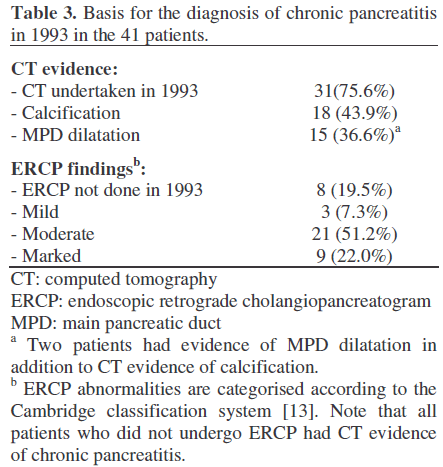
Patients with a discharge diagnosis of chronic pancreatitis (International Classification of Diseases, version 9:577.1) were identified by the audit department of the Manchester Royal Infirmary. Patients having this diagnosis made for the first time in 1993 were selected by study of the case notes. This process identified a population of 52 patients. Seven patients in whom the case notes could not be traced were excluded (five of these patients had died and notes were no longer available; listed causes of death in these patients were: gastrointestinal bleed in 1, alcoholic liver disease in 1, ischaemic heart disease 1, bronchogenic carcinoma in 1, and renal disease in 1). After study of case notes, 4 patients who were classified as having chronic pancreatitis but who had no clinical or radiological basis for making this diagnosis were excluded to leave a final study population of 41. The demographic profile of this population is seen in Table 2. Alcohol was the predominant etiologic agent accounting for 78%. The CT and ERCP basis for the diagnosis of chronic pancreatitis at the time of inclusion in the study is seen in Table 3. ERCP findings were categorised according to the Cambridge classification system [13].
Patients were then allocated categories according to the Manchester and ABC [12] classification systems. Case notes were then reviewed for information recorded at annual follow-up at yearly intervals over the subsequent decade. No deaths were recorded in these 41 patients over the follow-up period. Follow-up was grouped into three time periods: 1993-1995, 1996-1999 and 2000 to 2003.
Data are presented as medians and ranges. One-way ANOVA was used to compare the three groups and the Tukey-Kramer correction was applied when multiple comparisons were produced. The Pearson’s chi-squared test was applied to discrete data. The within-subject comparison of the classification scores was analysed by means of the sign test. Significance is accepted at the two-tailed P value less than 0.05 level. The StatsDirect version 2.4.5 software package was used (StatsDirect Ltd., Sale, Cheshire, UK; www.statsdirect.com).
Disease Progression from 1993 to 2003
At the outset of the study, 18 (44%) patients were categorised as having mild disease, 19 (46%) as moderate and 4 (10%) as end-stage. The number of patients with mild disease fell over the subsequent 5 years and at the end of the 10-year chart study period, no patients were categorised as mild (Figure 1).
The characteristics of the patients according to the Manchester score at the outset of the study are reported in Table 2. There were no significant differences in age among the three groups (P=0.252; Table 2). Symptoms had been present for a significantly shorter period of time in patients diagnosed in 1993 as mild chronic pancreatitis compared to those with moderate or end-stage disease (P=0.003 and P=0.001, respectively).
The number of patients with diabetes at the outset of the study period was 2 (5%). At two years this was 3 (7%), at five years 10 (24%), and at 10 years was 25 (61%).
Similarly, the number of patients with steatorrhoea at the outset was 2 (5%), at five years 6 (15%) and at 10 years 11 (27%) while there were no data for the two-year follow up point. Over the course of the 10-year period 11 (27%) patients underwent surgical intervention (distal pancreatectomy in 6, pseudocyst-gastrostomy in 2, pancreatic biopsy in 2, and Roux biliary bypass in 1).
Figure 2 shows categorical allocations of the 41 patient populations using the ABC classification system. Progression across stages of disease is similar and there were no patients with the mild stage of disease by the end of the study period (ABC stage A). Similarly, the proportion of patients allocated to the more severe stage (ABC stage C) increased.
The comparison between the Manchester and the ABS classifications showed that the two score systems were comparable at the outset of the study (P=1.000), while significant (P<0.001) differences were found in the following two time-intervals of the study.
There is a need for a classification system for chronic pancreatitis that can recognise and categorise distinct clinical stages and which has prognostic value. End-stage chronic pancreatitis characterised by endocrine and exocrine insufficiency and local extrapancreatic complications in addition to pancreatic parenchymal disease is often a clearly recognizable entity carrying implications both in terms of prognosis and treatment options and we have previously reported this as a discrete stage [11]. Similarly, a milder or earlier disease category associated with still-preserved exocrine and endocrine function is recognisable and the scoring system proposed here uses the term “mild” chronic pancreatitis for this stage [14]. Progression from mild to end-stage is marked by the development of exocrine and endocrine impairment and this intermediate stage is termed moderate chronic pancreatitis.
This categorisation system has evolved from clinical usage in this unit and requires appraisal and criticism from a broader community with an interest in chronic pancreatitis. It should be noted that other classification systems, notably the ABC system [12] is also derived from an individual unit.
As with the ABC classification, this categorisation is deliberately relatively simple. Much of the terminology sits well with other contemporary classification systems such as the Zurich consensus workshop [5, 6]. The Zurich system refers to “definite ACP” in relation to patients with definite-alcohol related chronic pancreatitis and although it states that terms such as “early” or “mild” can be misleading, it goes on to classify alcohol-related chronic pancreatitis into “early stage” or “late stage”. The disease descriptors for the Zurich “late stage” chronic pancreatitis overlap closely with the Manchester “End-stage” chronic pancreatitis. A limitation of the Zurich classification is its restriction to patients with alcohol-related chronic pancreatitis.
The limitations inherent in the design of this study should be understood when appraising the results: the data were collected retrospectively and thus assessment of features such as abdominal pain relies on historical notes rather than prospectively collected scores or other on-going assessments. The nature of the recruitment process may also introduce bias in that although these patients were new referrals, they were sent to a tertiary specialist centre and thus may not represent a typical disease spectrum.
What then can be learnt from this study? It provides useful information on disease progression in chronic pancreatitis suggesting that categorical allocation is both practical and feasible. It would appear that prognostic information of value to both patient and clinician can also be obtained by this categorisation process. In order to maintain a balanced perspective, it is emphasised that similar information can be gained by other scoring systems and also in practice by the expedient of establishing a diagnosis of chronic pancreatitis and a thorough assessment of exocrine and endocrine function. Nonetheless, the general acceptance of a categorisation system that uses simple, readily understood clinical terms in categorisation may promote greater attention to detail in deriving the information for categorical allocation and thus be of value in its own right.
The term end-stage chronic pancreatitis seems particularly important in the current era of sophisticated surgery for chronic pancreatitis [11]. The development and promotion of duodenum-preserving pancreatic head resection (DPPHR) makes the need for some form of generally accepted classification even more pressing: for example, are patients offered this procedure at the same stage of disease in different centres?
In summary, this study has examined patients presenting to a single pancreatic service in 1993 with a diagnosis of chronic pancreatitis. Patients have been allocated to distinct disease stages: mild, moderate or end-stage chronic pancreatitis based on a series of criteria and then the case notes studied in retrospect for the next 10 years. The results show that the Manchester classification of chronic pancreatitis is both practical and feasible and is worthy of further appraisal by other centres.
We acknowledge the expertise and leadership of Dr Joan Braganza. All these patients were treated under her care in the pancreatic clinic at Manchester Royal Infirmary and the availability of precise data is directly attributable to her attention to detail.
Papers based on this work have been read at the 6th World Congress of the International HepatoPancreatoBiliary Association, Washington DC, June 2004 (abstract in HPB 2004; 6(Supp1):206.) and also at the European Pancreatic Club Meeting, Padua, Italy, June 2004 (abstract in Pancreatology 2004; 4:129-212).