Key words
dental attendance, ethnicity, oral health,
qualitative methods
Introduction
General dental practice has received little attention in
the literature on diversity. The British Dental Association
(BDA) is aware of this problem (BDA, 2002; Gill
and Almond, 2004; Woodcock and Ellman, 2003) and
now has its own equality and diversity committee
whose most pertinent aims and objectives are (a) to General dental practice has received little attention in
the literature on diversity. The British Dental Association
(BDA) is aware of this problem (BDA, 2002; Gill
and Almond, 2004; Woodcock and Ellman, 2003) and
now has its own equality and diversity committee
whose most pertinent aims and objectives are (a) to
Research linking ethnicity and oral health (Beal,
1990; Bedi and Uppal, 1995; Dhawan and Bedi, 2001;
Gelbier and Taylor 1985; Kwan and Bedi, 2000;) has
brought several issues to the fore, including differences
in cultural oral health practices across ethnic
groups, access and uptake of dental services, language
and communication problems with dentists, the importance
of deprivation and the effects of changing
lifestyles on oral health. Newton et al (2001), in their
study of minority ethnic groups in South East London,
suggested that although distrust of the dentist was
a common perception across all minority ethnic
groups, barriers to the use of dental services varied
from group to group; for example, only black
Caribbean and Chinese/Vietnamese identified anxiety
as a significant barrier. People also felt that unnecessary
treatments were often performed which then
resulted in an increase in costs. Other barriers such
as anxiety, cost, language, cultural misunderstanding
and concern about hygiene standards were also uncovered
(Gibbons et al, 2000; Newton et al, 2001).
Williams and Gelbier (1989) have suggested that
reduced compliance could be a result of poor communication
or a lack of understanding. This results in
members of minority ethnic groups failing to understand
or follow instructions and thus getting stereotyped
as ‘problem patients’.
Very few qualitative studies investigating ethnicity
and oral health have been carried out in the UK
(Croucher and Sohanpal, 2006; Gibbons et al, 2000;
Newton et al, 2000). Those that have been undertaken
have largely concentrated on children or older age
groups. The qualitative component of these studies was
limited and was restricted by the use of focus groups
rather than in-depth interviewing. Croucher and
Sohanpal’s (2006) London study is of particular
interest in that, although it identified cost and anxiety
as the main factors inhibiting dental attendance, it
contradicted the work of others in the field (Gibbons
et al, 2000; Newton et al, 2000) by finding homogeneity
in the opinions of members of diverse minority
ethnic groups. Croucher and Sohanpal (2006) explained
this by stating that the poor socio-economic circumstances
of all the subjects in their study was the major
common causal factor.
The study reported here focused on second and
subsequent generations between the ages of 20and 45
years, a group that has been largely neglected in
previous research both of a qualitative and quantitative
nature. This age group was chosen to discover
whether respondents felt their beliefs and attitudes
were any different from those of their elders because of
their exposure to a different culture, and, if so, to
understand the reasons for their perceived changes in
their attitudes towards oral health. The aim was to
explore two main areas: (1) the concepts that people
from different minority ethnic groups have about the salience and timing of dental care and (2) their
perceived barriers to dental care. The University of
Glasgow Ethics Committee for Non-clinical Research
Involving Human Subjects issued a favourable opinion
about the study.
Method
Study design
A phenomenological research methodology was
adopted because the main focus of the study was on
the meanings respondents gave to their activities. The
aim of the analysis was to ‘establish the cognitive
universe or cosmology’ (Silverman, 1985, p.173) in
respondents’ thoughts about diet and oral health.
Qualitative semi-structured interviews (Strauss, 1987;
Strauss and Corbin, 1998) were used with men and
women from different ethnic groups, to build upon
previous work on ethnicity, oral health and diet
(Gibbons et al, 20 0 0 ; Newton et al, 2001). One hundred
respondents from Pakistani, Indian, Chinese and white
backgrounds, aged 20–45 years, were interviewed.
Seventy-five of the sample had been born in the UK,
while the remaining 25 had lived in the UK for a
minimum of 20years. This ensured that respondents
from the minority ethnic groups were primarily second
generation, and those from the white indigenous
sample could be used as a comparison group. Our
terminology for white corresponds with that of Bhopal
(2004); the term majority population is also used
synonymously for white British.
Sample
A purposeful sampling strategy (Maxwell, 1996; Miles
and Huberman, 1994; Patton 1990) was used to ensure
that the main ethnic groups living in Glasgow were
represented (Umeed, 2000). Electoral rolls of areas in
the city where people from minority ethnic groups
were concentrated, in conjunction with a name analysis
system, formed the principal basis for developing
the sample (Ecob and Williams, 1991). All potential
respondents were initially sent letters outlining the
purpose and scope of the study, including a short
screening questionnaire covering basic demographic
and household information enabling the selection of
appropriate respondents to fit the sampling frame.
Interviews were then arranged. The name analysis and
use of screening questionnaires had already proved
successful in Glasgow (Ecob and Williams, 1991;
Mullen, 1993). Little difficulty was experienced with
the use of the name analysis method, but there were a
few problems with the accuracy of the electoral roll
and in accessing respondents in multiple-occupancy tenement property. Consequently, we also obtained
supplementary lists of potential respondents by contacting
community organisations utilised by minority
ethnic groups (Miles and Huberman, 1994). On the
day of the interview, respondents were given an
information sheet which explained the scope and
purpose of the study and asked if they were willing
to sign a consent form. If they were in agreement the
interview went ahead. Before the tape recorder was
switched on a few demographic characteristics of
respondents were collected. All written material for
our study was in English.
A single dentist (RC), with considerable experience
in multi-ethnic research, carried out the qualitative
interviews. As the study concentrated on the second
generation, translation skills were not required for 80
respondents, although three interviews were conducted
by the interviewer in Punjabi and Urdu, and for
17 interviews within the Chinese community an
interpreter was used. Although the interviewer (RC)
had qualified as a dentist, this was not disclosed during
the course of any interview, his role remaining strictly
that of the research assistant.
The interviews
The overall aim was to discover the concepts that
people from different minority ethnic groups have about oral health and how such views may affect their
oral health practices. Our specific research questions
were to investigate the reasons for ethnic differentials
previously observed in oral health (Croucher and
Sohanpal, 2006; Gibbons et al, 2000; Newton et al,
2001; Williams andGelbier, 1989), identify those factors
which inhibit consulting a dentist, and highlight the
main areas where change could be implemented. In this
article, we present an analysis of respondents’ attitudes
towards dental attendance and dentists.

Being aware of the different patterns between minority
ethnic groups and the general population in
relation to both socio-economic position and employment
status (Modood and Berthoud, 1997; Williams
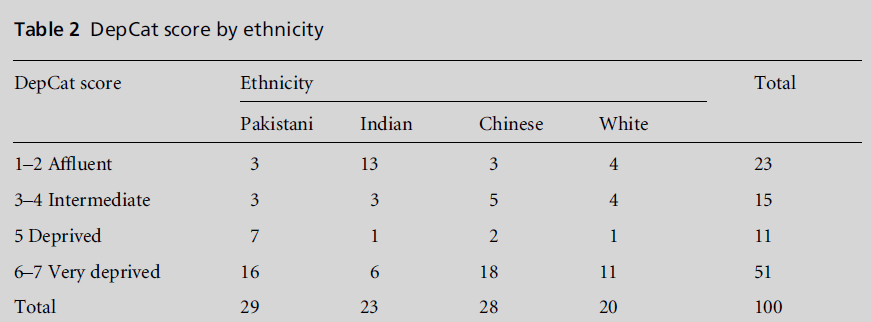
et al, 1998), questions focused on a variety of social indicators: level of education, occupation, employment
status, and Carstairs’ Deprivation Category (DepCat)
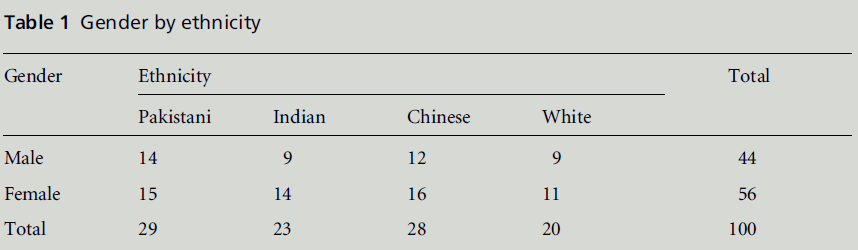
(Morris and Carstairs, 1991; see Box 1). The breakdown
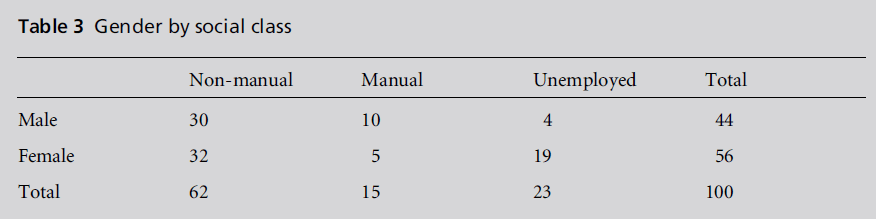
of the sample can be seen from Tables 1, 2 and 3. The numbers in Table 3 were derived from selected
data about respondents occupational titles and job
descriptions, and whether they were currently employed
or unemployed.
Table 1 :Gender by ethnicity
Table 2 :DepCat score by ethnicity.
Table 3:Gender by social class.
These categories make the research comparable
with previous studies of minority ethnic populations
(Modood and Berthoud, 1997) and those carried out
on the Scottish population (Central Research Unit,
2001). The respondents also accurately reflected the
employment experience of minority ethnic groups.
Previous writers have argued that social class measures
are often deficient in relation to research on ethnic
minorities (Smaje 1995; Williams et al, 1998). Researchers
have also argued that local area deprivation
measures are equally important (Chandola 2001;
Nazroo 1997). In our study we have followed this
lead, giving the deprivation index under each quotation
and in Table 2.
Analysis
The two theoretical approaches that guided the analysis
were grounded theory (Glaser, 1978; Glaser and
Strauss, 1967; Strauss, 1987) and analytic induction
(Cressy, 1973; Lindesmith, 1968; Znaniecki, 1934).
Hammersley (1990, p.604) maintains that the two
approaches are ‘attempts to apply the hypotheticaldeductive
method to ethnography’. The final goal of
both grounded theory and analytic induction is the
same and this goal can be distinguished from research
using statistical methods: ‘The claim is not to
representativeness but to faultless logic’ (Silverman,
1985, p.14).
The semi-structured interviews (Strauss, 1987;
Strauss and Corbin, 1998) lasted approximately one
hour and were tape recorded. All interviews were
transcribed by a secretary who was employed for that
purpose, coded and indexed as soon as they were
completed. This allowed for important emergent
themes in the data to be followed up in the interviews
of subsequent respondents (Mullen, 1993; Strauss, 1987). To ensure the validity and reliability of the
initial coding frame, a selection of transcribed interviews
was coded independently by one of the principal
investigators (KM) and the research assistant (RC).
High degrees of agreement were achieved. Data were
initially analysed using QSR (Qualitiative Solutions
and Research) NVivo (QSR, 2002), and emergent
themes were noted and included in the coding frame
(see Dowell et al, 1995; Lindesmith, 1968).
Details of the technicalities of the process of transcription
and computer coding can be found in Fielding
and Lee (1991) and Pfaffenberger (1988). In practice,
NVivo was extremely useful in the early stages of the
analysis, which involved the production of descriptive
material. However, the researchers felt it to be inflexible
when they wished to progress from a purely
descriptive presentation of the material to the development
of an analytic focus. Initial descriptive coding,
using NVivo, was carried out jointly by the research
assistant (RC) and the principal investigator (KM) to
ensure reliability. Subsequent analytic coding, axial
and selective (Flick, 2006), was carried out by the
principal investigator (KM) using paper transcripts
generated byNVivo. In the results section that follows,
the subthemes presented are those that emerged from
the data and are the respondents’ own categorisations.
Results
Importance and frequency of dental
attendance
A perceived generational shift was seen to be an
important influence on attitudes towards oral health.
The older generation in the ethnic minority communities
was considered to be less knowledgeable
about oral health, as a 45-year-old Chinese respondent,
housewife and mother of three children, stated:
R24: ‘I think it is the generation, and the Chinese culture,
they don’t have much knowledge of oral health.’
Interviewer: ‘And what do you think is the reason for
that?’
R24: ‘I feel they pay attention to other things but not oral
health.’
Interviewer: ‘And the reason behind that?’
R24: ‘I think they do not have much education on the
subject or knowledge, they don’t know that they have to
look after their health, or oral health, but now in this
generation they know more about oral health.’ (DepCat 7)
A 28-year-old male, part-time marketing lecturer,
from an Indian background echoed this view:
R1: ‘Absolutely, yeah, as an Indian, I think y’know my
parents’ attitude towards oral health has been pretty
relaxed, they weren’t as proactive as I am in relation to
oral health.’ (DepCat 6)
The issues of aesthetics and the importance of good
oral health were considered to be more pronounced
among this younger generation, compared with their
elders, as a 30-year-old female Chinese health development
officer stated:
R22: ‘Confidence-wise, I know when I had a gap in my
tooth I was very conscious of it and I didn’t want to smile
and things like that. Just the whole appearance ... if you
don’t have good oral hygiene you would have bad breath
and things like that.’ (DepCat 6)
Respondents viewed themselves as having a greater
awareness of oral health than their parents, and did try
to make an effort to visit the dentist. However, even
though they were aware of the recommendation that
the dentist should be visited every six months, there
were many instances of people only going to the
dentist when something was wrong. Thus, the dentist
was seen more as a problem solver rather than someone
to be seen on a regular basis, as reported by a 33-
year-old Pakistani male pharmacist:
R3: ‘I think a person should visit a dentist maybe at least
three times a year, just for a general check-up. And
obviously if they are in any kind of pain they should go
and see a dentist immediately. But I don’t practise it. I
should go, but a reason being is the time trying to go with
a busy life, so I end up postponing. The only time I go is
if I am having problems with my teeth or gums.’
(DepCat 6)
Although this was a common tendency across all
groups, the white group reported they went more
regularly for six-month check-ups, and women tended
to make more regular visits to the dentist than men.
However, there was also a feeling among some that
six-monthly visits were too regular.
Barriers to dental care
Barriers experienced by first-generation members of
ethnic minorities when visiting the dentist include
those such as language, communication, and cultural
awareness, but these did not directly affect most respondents in our sample. However, other barriers
to attending such as expense, time, lifestyle factors and
anxiety were of concern. There were difficulties associated
with arranging a suitable time in the day when
they could get an appointment. As one 32-year-old
Chinese male general practitioner (GP) stated:
R89: ‘The time, yeah, because you have to make an
appointment to see a dentist and not many dental practices
are open at the weekend. Week days are impossible
for me to go.’ (DepCat 2)
The tension between the dentists’ and patients’ timetables
can also be seen in this quotation from another,
this time 29-year-old, Chinese male day care officer:
R12: ‘Sometimes the dentist that I attend is a very busy
dentist and if I want to make an appointment after 5 or 6,
sometimes I need to wait a while, but sometimes when I
have finished work, I am feeling tired and I don’t really
want to go anywhere, I just want to get straight home.’
(DepCat 2)
Expense was a particular concern, and some respondents
preferred to use the community or hospital
services, where no fee was charged, even though this
took up more of their time. Financial issues were also
salient in their discussion of NHS versus private
dentistry. There was a general perception that private
dentists were more competent, although whether this
was based on experience or anecdote was difficult to
fully ascertain. Respondents often wished they could
have a private dentist but because of cost considerations
had to remain with an NHS dentist. As a 41-
year-old Pakistani self-employed male with three
children said:
R64: ‘I have come across a number of dentists that I have
visited. They were not as capable as those dentists that
only took private patients – they have been double capable
than those who are operating on the national health
service ... But unfortunately with the state of my teeth it
would cost me a fortune to get my teeth fixed.’ (DepCat 5)
Cost issues and access were also exacerbated by the
perception that there were fewer NHS dentists available.
As a 33-year-old Indian female educational
project officer with one child stated:
R57: ‘Often you find it is a problem with the private and
the NHS ... an excellent dentist was recommended to me,
but when I went to make an appointment, I was told he is
not taking any more patients. So that was a bit of an issue.
And then others, unfortunately, that are very good tend to
go into private practice. I can’t afford to go into private
you know.’ (DepCat 2)
Additionally, a 35-year-old white male unmarried
journalist stated:
R92: ‘That is quite a foggy area ... I amaware that there are
not many NHS dentists left any more. As soon as they
open up you are continually watching news stories about a thousand people queuing up outside, so I think it is
confusing.’ (DepCat 6)
Fear of the dentist, dental anxiety and a feeling of ‘a
lack of control’ emerged as an important issue. This
stemmed either from the effects of a general fear of
pain, or was linked to specific clinical instances described
by our respondents. The following was expressed
by a 31-year-old single Pakistani male:
R87: ‘Number one, I am scared of drills number two,
scared of the syringes and number three, scared of having
my teeth pulled. These are the only reasons. It just totally
freaks me out just seeing the needle. That is why I don’t
like going because any time that you are getting any tooth
work done you have got to get injections so therefore I try
to avoid it as much as possible.’ (DepCat 6)
Some respondents also mentioned early childhood
experiences which had heightened their anxiety about
dental treatment. Other respondents were anxious
about appropriate sterilisation of equipment.
Communication and the explanation of procedures
was an issue for some individuals, particularly regarding
the use of dental jargon. Some respondents wished
to see more communication between the dentist and
patient. This was particularly important as some
respondents saw a close link between good communication
and lowered anxiety in the dental surgery.
However, most respondents felt that their dentist
communicated with them satisfactorily and explained
treatment to them before carrying out any procedures.
As a 37-year-old white single male working part-time
said:
R41: ‘Yeah, yeah he is very good he is always talking away
and explaining what he is doing.’ (DepCat 6)
Language problems relating to visits to the dentist
were still a problem for the Chinese community. As
reported by a Chinese female, married housewife with
three children, aged 45 years:
R24: ‘It is really only the language barrier as you don’t
know how to explain to the dentist what the problem is.’
(DepCat 7)
For other non-white groups, language was believed by
respondents to have been more of an issue for the
previous generation, although the current generation
occasionally helped in an advocacy role in the dental
surgery. A 37-year-old Pakistani male, married GP,
stated:
R77: ‘I don’t think so for myself no, for my mother yes, for
her to explain, or if I am not available or my father is not
available she is not comfortable with the person that she is
seeing and speaking to and he has to try his best to
communicate with her ... He has to understand the ethnic
diversity and her health beliefs and customs and various
other things before she would feel comfortable.’ (DepCat 2)
The ethnicity of the dentist was not an issue, except in
the case of some minority ethnic women, who preferred
to see a female dentist. Interestingly, if they were
to see a male dentist, they preferred an indigenous
person rather than someone from their own community.
One 24-year-old single female Pakistani development
worker said:
R36: ‘Gender, no, I know it is very stupid, but I would not
mind a white male dentist, but I would mind an Asian
male dentist, I don’t know what the reason is.’
Interviewer: ‘There must be a reason behind it.’
R36: ‘I don’t feel comfortable with Asian guys as there is
the cultural factor going on there and you just don’t feel
comfortable.’
Interviewer: ‘Do you think it becomes much more personal
if you go to an Asian dentist rather than a white
dentist?’
R36: ‘Yes, I would say so.’ (DepCat 5)
As a 33-year-old Indian woman, married administrator
with two children, said:
R72: ‘If it was an Asian male I would probably feel a bit
uncomfortable, I don’t know why. If there was an option
you know, otherwise it makes no difference to me, I would
go to an Asian male doctor, so this is just a dentist, but if
there was a choice then I would pick the white male.’
Interviewer: ‘Why would you do that?’
R72: ‘Probably just because of my upbringing you know,
that I don’t know, it must have something to do with the
way that I was brought up, like, culturally.’ (DepCat 2)
And a quotation from another Pakistani unemployed
female aged 34 years:
R74: ‘Before I used to go to the dental hospital, there was
Asian dentists there. I used to feel a bit awkward, as I am
Asian and I don’t like anyone Asian looking into my
mouth. I think it is me just being stupid.’ (DepCat 4)
Issues of professionalism were important to many
respondents. A 34-year-old white female, single and
self-employed, stated:
R91: ‘His attitude was really annoying ... it was an awful
experience and he was shaving away parts of my teeth in
order to make the one that he done fit. I asked to see a
mirror to see what he was doing and he just went ballistic,
and I think ‘‘you are so old school. If you believe in your
work you will let me watch you shave a bit of my good
teeth’’. He was absolutely really quite cheeky and I
thought what a wholly unpleasant experience. I just think
he hadn’t been used to people answering him back.’
(DepCat 6)
By contrast, a 30-year-old Indian male accountant
assistant, married with two children, said:
R83: ‘Very professional. They know what they are doing.
They actually play music. They have the radio on as well.
That is something that they did not do about 20years ago.
It is a slightly more friendly atmosphere, you go in and
you have flower plant pots and it is a nice airier room.
They have all the new technical stuff and all the high-tech
chairs and instruments, they are all friendly. They have
their masks on for health and safety as well; that is good to
see just like visiting a hospital sort of thing.’ (DepCat 2)
In this respondent’s mind, along with standard professional
issues relating to good health and safety
standards and practices, situational elements were
also viewed as an important part of a professional
approach.
Discussion
Early studies on ethnicity and oral health found a
lack of awareness of standard oral health messages
(Bedi and Uppal, 1995; Prendergast et al, 1997;
Williams and Fairpo, 1988), although more recent
research is tending to show a greater understanding
(Gibbons et al, 2000; Newton et al, 2000, 2001). In
general we discovered that respondents’ awareness of
the standard dental healthmessagewith regard to dental
attendance was high. The problem, which is clearly
stated in most health belief models, is how to help
people follow this through and overcome barriers to
dental care. Respondents viewed themselves as being
more pro-active in attending the dentist than members
of first-generation ethnic minorities, but many
still only visited the dentist when symptoms arose.
It is now the case that many of the issues surrounding
accessing oral health care among different ethnic
groups are general oral health-related issues: such as
dental anxiety (Stewart et al, 1994; Wardle, 1982), and
the personality of the dentist (Bernstein et al, 1979).
The major barriers to regular dental attendance were
not specifically associated with ethnicity but were
related to cost (Finch, 1988), time and dental anxiety,
as well as a dentist’s competence, skill, cleanliness and
ability to communicate. Two additional barriers highlighted
by Newton et al (2001), of distrust of the
dentist and fear of unnecessary treatments, did not
come through in our study.
Similarities found between ethnic groups highlight
the fact that the context ofwork and family puts a time
structure on people’s everyday lives, and this explains
why oral health behaviours such as regular dental
attendance may drop down the list of an individual’s
priorities. Flexibility in the timing of dental appointments
is an important issue.
The results also highlight general problems associated
with cost and accessing NHS dentistry. Private
dentistry was also perceived as having the edge over
NHStreatment. However, care needs to be taken when drawing conclusions, as this view was often based on
anecdotal rather than experiential evidence.
Previous investigations have shown that language
can constitute a major barrier to the receipt of dental
care (Bedi and Uppal, 1995; Williams and Gelbier,
1989). A study conducted in London among older
ethnic groups found language was a particular concern
with the Indian, Pakistani, Bangladeshi and
Chinese participants (Newton et al, 2001). Our study,
conducted among second-generation ethnic groups,
found that, with the exception of the Chinese community,
language was not a direct problem, although
some respondents reported having an advocacy/interpreter
role in relation to accompanying older relatives
to dental surgeries.
Research in dentistry on gender issues of the dentist/
patient relationship has been sadly neglected (Humphris
and Ling, 2000; Kent and Croucher, 1998). One area of
our findings where we did discover differences relating
to culture was in some Pakistani women’s negative
attitudes towards treatment by male dentists from
their own community. This was not purely a gender
issue but related to cultural factors. Similar findings
have been indicated in relation to attitudes towards
general medical practitioners (Ahmad et al, 1991) but
ours is the first study to focus on dentist/patient
interaction.
Our study demonstrates the advantages of using the
qualitative interview method to understand the complexity
of people’s reasoning when they come to the
decision to consult a dentist. An example is the pressures
of work and family cross-cutting minority ethnic
affiliation – such a dynamic inter-relationship would
not have been uncovered by quantitative research.
The age group, from 20 to 45 years, and the
additional entry criterion of having to have lived in
the UK for at least 20ye ars were chosen as there was
interest in discovering the beliefs of second-generation
migrants, people for whom there may be a tension
between the beliefs and attitudes of their elders and
those of current social norms.
The care in the selection of our respondents means
our findings are generalisable to the other major
studies carried out on these, the main minority ethnic
groups in the UK (Modood and Berthoud, 1997).
They do not, however, directly relate to those parts of
dental studies where other minority ethnic groups
have been considered, in particular the Caribbean,
Bangladeshi, or Vietnamese populations (Bedi and
Uppal, 1995; Gibbons et al, 2000; Laher, 1990;
Prendergast et al, 1997; Williams and Fairpo, 1988).
To conclude, our findings demonstrate that acculturation
has occurred to a large extent in relation to
attitudes towards visiting the dentist, and that the perceptions
found among the different second-generation
minority ethnic groups now fit with current generalpopulation
trends. This is an advance on the recent work in the east end of London by Croucher and
Sohanpal (2006), who although finding homogeneity
in views across minority ethnic groups put this down
to similar levels of elevated social disadvantage. Our
more diverse sample of respondents fromanother area
of the UKindicates that convergence of views may be a
more general phenomenon.
Some issues still remain, however, and it is therefore
important that we continue to be sensitive to the
heterogeneity within ethnic groups. Finally, while we
acknowledge that our results are not generalisable to
other minority ethnic groups, we propose that the
future use of such qualitative methods in this research
field will greatly enhance our understanding of how
patients view access issues, and enable us to tailor our
oral health interventions.
Our central aim should always be to ensure that
culturally competent practice in the delivery of dental
services is achieved. Health services, including dental
services, have to relate to the needs of all sections of the
community. The priority is to meet varied individual
needs and expectations. This is irrespective of a person’s
race, heritage, sex, religious or non-religious belief,
nationality, family background, age, disability or
sexuality.
Acknowledgment
This research was funded by the Scottish Executive
Health Department Chief Scientist Office, grant number
CZH/4/53. We also acknowledge the helpful
comments of David Conway on an earlier draft of
this article.
References
- Ahmad WIU, Kernohan EEM, and Baker MR (1991) Patients’ choice of general practitioner: importance of patients’ and doctors’ sex and ethnicity. British Journal of General Practice 41:330–1.
- Beal J (1990) The dental health of black and ethnic minority communities. Community Dental Health 7:122.
- Bedi R and Uppal RDK (1995) The oral health of minority ethnic communities in the United Kingdom. British Dental Journal 179:421–5.
- Bernstein D, Kleinknecht R and Alexander L (1979) Antecedents of dental fear. Public Health Dentistry 39: 113–24.
- Bhopal R (2004) Glossary of terms relating to ethnicity and race: for reflection and debate. Journal of Epidemiology and Community Health. 58:441–5.
- British Dental Association (BDA) (2002) Religious and Cultural Diversity. www.bda.org/advice/docs/E9.pdf (accessed 29 March 2007).
- Central Research Unit (2001) Scoping Study for a National Study of Scotland’sMinority Ethnic Populations. Edinburgh: Scottish Executive.
- Chandola T (2001) Ethnic and class differences in health in relation to British South Asians: using the new National Statistics Socio-Economic Classification. Social Science and Medicine 52:1285–96.
- Cressey D (1973) Other People’sMoney. New Jersey: Patterson Smith. Croucher R and Sohanpal R (2006) Improving access to dental care in East London’s ethnic minority groups: community based, qualitative study. Community Dental Health 23:95–100.
- DhawanNandBedi R (2001) Transcultural oral health care: 6. The oral health of minority ethnic groups in the United Kingdom – a review. Dental Update. 28:30–4.
- Dowell J, Huby G and Smith C (1995) Scottish Consensus Statement on Qualitative Research in Primary Health Care. Dundee: Tayside Centre for General Practice.
- Ecob R and Williams R (1991) Sampling Asian minorities to assess health and welfare. Journal of Epidemiology and Community Health 45:93–101.
- Fielding NG and Lee RM (1991) Using Computers in Qualitative Research. London: Sage. Finch E (1988) Barriers to the Receipt of Dental Care. London: Social and Community Planning.
- Flick U(2006) Introduction to Qualitative Research. London: Sage. Gelbier S and TaylorWS(1985) Some Asian communities in the UK and their culture. British Dental Journal 8:416–18.
- Gibbons DE, Gelbier S and Newton T (2000) The Oral Health of Minority Groups in Contemporary Britain: a case study in the SouthThamesRegion. London: GKTDental Institute, Kings College.
- Gill A and Almond J (2004) Developing diversity. BDA News 17:3–12.
- Glaser B (1978) Theoretical Sensitivity. Mill Valley: The Sociological Press. Glaser B and Strauss AL (1967) The Discovery of Grounded Theory. Chicago: Aldine.
- Hammersley M (1990) What’s wrong with ethnography? Sociology 24:597–615. Humphris G and Ling MS (2000) Behavioural Sciences for Dentistry. London: Churchill Livingstone.
- Kent G and Croucher R (1998) Achieving Oral Health: the social context of dental care. Oxford: Wright.
- Kwan SYL and Bedi R (2000) Transcultural oral health care and the Chinese – an invisible community. Dental Update 27:296–9.
- Laher MHE (1990) A comparison between dental caries, gingival health and dental service usage in Bangladeshi and white Caucasian children aged 7, 9, 11, 13 and 15 years residing in an inner city area of London, UK. Community Dental Health 7:157–63.
- Lindesmith AR (1968) Addiction and Opiates. Chicago: Aldine.
- Maxwell JA (1996) Qualitative Research Design: an interactive approach. London: Sage.
- MilesMB and HubermanAM (1994) Qualitative Data Analysis. London: Sage.
- Modood MB and Berthoud R (1997) Ethnic Minorities in Britain. London: Policy Studies Institute.
- Morris R and Carstairs V (1991) Which deprivation? A comparison of selected deprivation indexes. Journal of Public Health Medicine 13:318–26.
- Attitudes towards dental care among second-generation ethnic groups 99 Mullen K (1993) A Healthy Balance: Glaswegian men talking about health, tobacco and alcohol. London: Avebury.
- Nazroo J (1997) The Health of Britain’s Ethnic Minorities. London: Policy Studies Institute.
- Newton JT, Khan FA, Bhavnani V, Gelbier S and Gibbons DE (2000) Self-assessed oral health status of ethnic minority residents of South London. Community Dental Oral Epidemiology 28:424–34.
- Newton JT, Thorogood N, Bhavnani V, Gibbons DE and Gelbier S (2001) Barriers to the use of dental services by individuals from minority ethnic communities living in the United Kingdom: findings from focus groups. Primary Dental Care 8:154–61.
- Patton MQ (1990) Qualitative Evaluation and Research Methods. Newbury Park: Sage.
- Pfaffenberger B (1988) Microcomputer-application in Qualitative Research. London: Sage.
- Prendergast MJ, Beal JF and Williams SA (1997) The relationship between deprivation, ethnicity and dental health in 5-year old children in Leeds, UK. Community Dental Health 14:18–21.
- Qualitative Solutions and Research (QSR) (2002) QSR NVivo User Guide. Victoria: Qualitative Solutions and Research.
- Silverman D (1985) Qualitative Methodology and Sociology. Aldershot: Gower. Smaje C (1995) Health Race and Ethnicity. London: King’s Fund Institute.
- Stewart J, Marcus M, Christenson P and Lin W (1994) Comprehensive treatment among dental school patients with high and low dental anxiety. Journal of Dental Education 58:697–700.
- Strauss A (1987) Qualitative Analysis for Social Scientists. Cambridge: Cambridge University Press.
- Strauss A and Corbin J (1998) Basics of Qualitative Research: techniques and procedures for developing grounded theory. London: Sage.
- Umeed I (2000) Health Needs and Knowledge: self-reported health status of South Asian men in Glasgow. Glasgow: Greater Glasgow Health Board.
- Wardle J (1982) Fear of dentistry. British Journal of Medical Psychology 55:119–26.
- Williams R, Wright W and Hunt K (1998) Social class and health: the puzzling counter-example of British South Asians. Social Science and Medicine 47:1277–88.
- Williams SA and Fairpo CG (1988) Cultural variations in oral hygiene practices among infants in an inner city. Community Dental Health 5:265–71.
- Williams SA and Gelbier S (1989) Dentists and ethnic minority communities. British Dental Journal 166:194–5.
- Woodcock J and Ellman L (2003) Open wide (BDA’s equality and diversity committee), Bill watching. BDA News 16:30–6.
- Znaniecki F (1934) The Method of Sociology. New York: Rinehart.