Tomczyk K1*, Chmaj-Wierzchowska K1, Izycka N2 and Wilczak M1
1Department of Mother and Child Health, University of Medical Sciences, Poznan, Poland
2Department of Gynecological Oncology, University of Medical Sciences, Poznan, Poland
- *Corresponding Author:
- Tomczyk K
Department of Mother and Child Health, University of Medical Sciences, Poznan, Poland
Tel: +48515182726
E-mail: katarzyna.zielin@gmail.com
Received Date: May 30, 2019; Accepted Date: August 13, 2019; Published Date: August 20, 2019
Citation: Tomczyk K, Chmaj-Wierzchowska K, Izycka N, Wilczak M (2019) Extirpation of a Giant Ovarian Tumor: A Case Report. Gynecol Obstet Case Rep. Vol. 5 No.2:78.
Keywords
Cystadenoma; IOTA protocol; Laparoscopy; Laparotomy; Oophorectomy; Ovarian tumor
Introduction
Ovarian epithelial tumors account for 65-75% of all ovarian tumors. Histologically, these tumors may be divided into three categories: benign, borderline and malignant. The benign mucinous (40%) have a 10-year survival rate of 100%. In borderline tumors (10%) 10-year survival rate is about 60%. The third group of the malignant tumor has a 10-year survival rate at 30-40% [1]. Ovarian tumors are most commonly observed in adults. In children (age <16 years) less than 2%) [2]. Before every surgical treatment, the whole diagnostic process should be performed in order to plan an adequate surgical procedure (the way and the range). Unfortunately, there is a lack of diagnostic knowledge as well as reliable and accurate diagnostic methods that could precisely assume the type of the lesions. This paper analyses a case report of a young woman with an enormous ovarian tumor in the abdomen and pelvis. The purpose of the work was to describe possible diagnostic methods before the surgical treatment and to comment on surgical problems dealing with removing giant ovarian tumors.
Case Presentation
The 22-year-old patient was admitted to the hospital due to abdominal pain and abdominal distension. She reported a noticeable increase in the abdominal circumference and episodes of lumbar pain lasting for 6 months before the time of admission. She suffered from nausea and obstructions. No other complains were noticed. She was a nulliparous woman with regular menses, lasting 5-7 days. Medical history revealed no previous surgeries or illnesses except anorexia nervosa during adolescence. Negative family history was noticed.
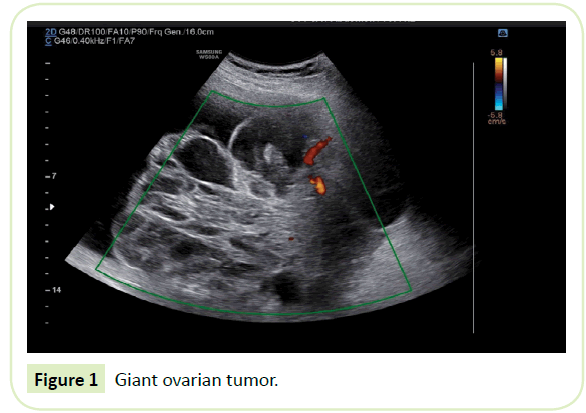
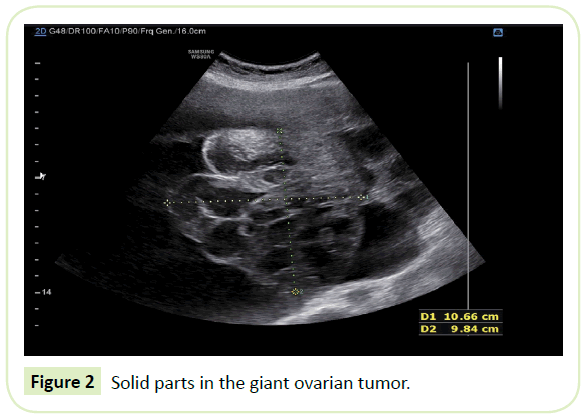
The physical examination revealed a giant mass filling the pelvis and abdominal cavity (reaching the level of navel), causing distension of the abdominal wall. The uterus was palpable, moved to the right. During hospitalization, a complete study was performed. Vaginal ultrasound examination showed an enormous multiloculated tumor not possible to measure as a whole change. Abdominal ultrasound examination revealed that the tumor filled the pelvic and abdominal cavity, approximately 30 cm in diameter. The tumor was evaluated according to IOTA terms and definitions as a multilocular-solid tumor with cysts filled with anechoic fluid, with the presence of solid component, measuring 147 × 103 mm. The most possible origin of the tumor was the ovary. The uterus was not visible. Moderate blood flow in the solid components of the tumor was detected using Doppler ultrasound (color score 3). The IOTA ADNEX model showed 93,8% risk of malignancy, including 41.9% risk of borderline ovarian tumor and 6.2% chance for a benign tumor (Figures 1 and 2). IOTA Logistic Regression 1 and 2 models were also calculated for this patient-they showed the risk of malignancy at the level of 0.998 and 0.999, respectively.
Figure 1: Giant ovarian tumor.
Figure 2: Solid parts in the giant ovarian tumor.
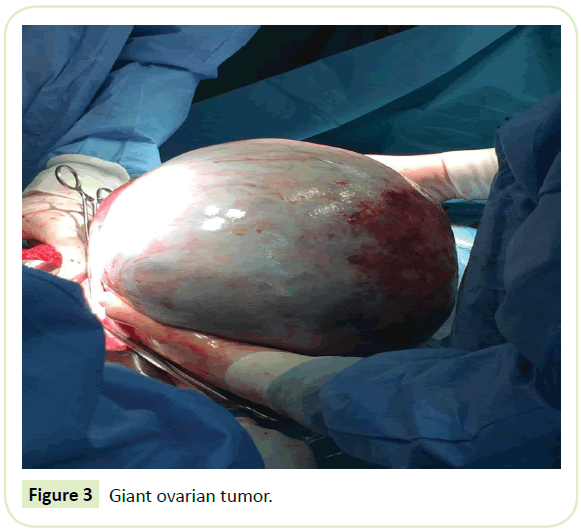
In USG examination the left kidney was unchanged, while the right was not visible. Due to the size of the tumor, urography and colorectal contrast infusion were also performed. Intestines were unaffected but urography showed right urethral dilation and hydronephrosis due to the tumor pression (Figure 3). Lungs X-ray showed lifted diaphragm right crus. Morphology was correct. Serum tumor markers: Carcinoembryonic antigen and alpha-fetoprotein were within the normal range. The biochemistry blood test revealed high C- reactive protein, elevated Ca125, and HE4 levels. The ROMA index calculation for this patient revealed 58.9% risk of malignancy of the tumor. Others laboratory tests are presented in Table 1.
Figure 3: Giant ovarian tumor.
| Variables |
Result |
Norm |
| CRP |
177.20 mg/L |
0.08-3.1 mg/L |
| Ca 125 |
96.19 U/ml |
35 U/ml |
| HE4 |
159.80 pmol/L |
0-60.5 pmol/L |
| Betha-hCG |
0.1 mIU/mL |
<0.1 mIU/mL |
| APTT |
33 sek |
26-36 sek |
| D-dimer |
4691.0 ng/mL |
490 ng/ml |
| fibrynogen |
10.64 g/L |
1.8-3,5 g/L |
| PT |
16.1 sek |
13-17 sek |
| INR |
1.46 |
2-4 |
| Creatynin |
0.58 mg/dL |
0.6-1.3 mg/dL |
Table 1: Laboratory results.
Open laparotomy was preferred rather than laparoscopy, for the high possibility of the malignant origin of the ovarian tumor. Right salpingo-oophorectomy with the intact removing of the integral tumor mass during laparotomy was conducted. Because of the enormous size of the mass and the high risk for malignancy, the midline incision was performed. Surgery was conducted with the use of ligasure vessel sealing system, thus the amount of blood loss was minimal, and the surgery time was shorter. The histopathology result of the frozen section, as well as the result, was cystadenoma proliferans casus limitans-borderline tumor-33 cm in diameter-with a smooth outer surface and a solid structure sized 16 cm on the inner surface. The surgery was uncomplicated. Further pharmacological treatment included antibiotics: Cefuroksime axetil 3 × 1500 mg I.V., Amikacin 2 × 500 mg I.M., Metronidazole 3 × 500 mg I.V, Enoxaparine 40 mg/ml and painkillers. The post-operative recovery was uncomplicated. The patient was discharged in a good condition on the 7th day after surgery.
Discussion
Ovarian tumors may be divided in four categories [3] (Table 2). The most common type of epithelial ovarian tumors is a benign cystadenoma, and the serous type (75%) is more common than the mucinous type (25%) [4,5]. The reason for the latest one is inclusions of the ovarian celomic epithelium and usually, these tumors occur in patients of the age 40 and 50 [6]. 15% of the mucinous cystadenomas are malignant [4,7]. Now-a-days, giant ovarian tumors are a rare condition, probably as a result of early diagnosis and treatment. The tumors are often asymptomatic at smaller sizes, easy access to gynecologists; and furthermore, imaging methods like the ultrasound make it easy to diagnose and treat at that stage.
| Types |
Examples |
| Epithelial tumors |
Serous or mucinous cystadenoma or cystadenocarcinoma, Brenner tumor, clear cell carcinoma |
| Germ cells tumors |
Dysgerminoma, choriocarcinoma, teratoma |
| Sex-cord stromal tumors |
Thecoma, fibroma |
| Metastatic tumors |
Uterine, stomach, colon, breast and lymphoma |
Table 2: Types of ovarian tumors.
The role of computed tomography (CT) scan and magnetic resonance imaging may provide more information about the extension of the tumor, its origin and character [8,9]. Laboratory tests, mainly Ca-125 and ROMA might be crucial in malignancy cases [10]. Still, USG examination provides us with important diagnostic information. Because of that simple, cheap and widely available method, giant ovarian tumors are rarely observed and diagnosed. The ovarian cyst is commonly found incidentally, as a small change, during routine gynecological control. On the contrary, many difficulties lie in the diagnostic process of ovarian masses, especially the borderline ovarian tumors. They show many inconsistencies according to tumor marker expression, features in the ultrasound examination and are often inaccurately identified using frozen sections during the surgery. Therefore, the histopathological examination remains the only way of definitive diagnosis of these tumors.
Despite the diagnostic complexities, the development of the IOTA algorithms for the diagnosis of ovarian masses resulted in easier and more adequate pre-operative classification and identification of the lesions. It seems that the IOTA simple rules are effective and provide simple, general rules even for inexperienced ultrasonographers in distinguish between benign and malignant ovarian tumors [11,12]. In the Timmerman study, the IOTA simple rules examination classified correctly 75% cases [11]. Commonly an ovarian cyst is surgically removed when it reaches 4 cm in diameter due to the higher risk of ovarian torsion [13]. Now-a-days for benign tumors laparoscopic enucleation of the cyst or salphingooophorectomy remain the basic surgical techniques [14]. However, the choice of an operative method requires assessment of the patient's age, the size of the cyst and its histopathological character [14].
Giant tumors must be removed due to compressive symptoms. It is necessary to assess the risk of malignancy. The preoperative diagnostic assessment is of utmost importance. Authors suggest that the giant ovarian tumors are usually benign [14,15]. In those cases, laparoscopic extirpation of a giant tumor with cyst drainage (preoperative or during the operation) seems to be a gold standard [16,17]. The preoperative drainage might be achieved in two ways such as ultrasound-guided aspiration or with the use of the Bonanno catheter [17]. Laparoscopic treatment is beneficial as it reduces postoperative pain, risk of wound infection, hospitalization and provides a better cosmetic result that is important for young women. Another well-studied advantage is less chance of postoperative pelvic adhesions which means less possibility for infertile problems in the future [15]. However, that technique encounters some difficulties in case of removing giant ovarian cysts. Although the risk of rupture of a cyst, limited visualization, and the workplace are of the biggest concern, data indicates that the spillage of a malignant cyst content does not worsen the prognosis and survival rate [18-21].
Conclusion
For both techniques (laparoscopy and laparotomy), it is significant to remember about circulatory depression and re-expansion pulmonary edema because of sudden removal of the enormous mass and a big amount of fluid from the tumor. Therefore, some authors prefer slow pre-operative drainage of the giant cyst in epidural anesthesia. In the case of malignancy risk, the efficacy of that procedure remains uncertain. In case of increased malignancy risk, removal of the whole mass and avoidance of the spillage of the cyst into the abdominal cavity seems to be safer. The preoperative diagnostic process is crucial, and the IOTA examination appears to be effective enough in planning the surgical treatment. It is of the greatest advantage to perform those ultrasound assessments before every surgical removal of an adnexal tumor. In our case the IOTA examination revealed the risk of borderline change. Laparotomy was decided to be more reasonable management.
References
- Posabella A, Galetti K, Engelberger S, Giovannacci L, Gyr T, et al. (2014) A huge mucinous cystadenoma of ovarian: A rare case report and review of the literature. Rare Tumors 6: 5225.
- Bicer S, Erkul Z, Demiryilmaz I, Peker N (2014) A 9-kg ovarian mucinous cystadenoma in a 14-year-old premenarchal girl. Am J Case Rep 15: 326-329.
- Kumar V, Cotran R, Robbins S (2007) Current views on the mechanism of oncogenic cell transformation in ovine pulmonary adenocarcinoma. Postepy Hig Med Dosw 61: 797-804.
- Norris HJ, Jensen RD (1972) Relative frequency of ovarian neoplasms in children and adolescents. Cancer 30: 713-719.
- Grapsa D, Kairi-Vassilatou E, Kleanthis C, Dastamani C, Fillipidou A, et al. (2011) Epithelial ovarian tumors in adolescents: A retrospective pathologic study and a critical review of the literature. J Pediatr Adolesc Gynecol 24: 386-388.
- Gorgone S, Minniti C, Ilaqua A, Barbuscia M (2008) Giant mucinous cystadenoma in a young patient. A Case Rep G Chir 29: 42-44.
- De-Lima SH, Dos-Santos VM, Darós AC, Campos VP, Modesto RF (2014) A 57-year-old Brazilian woman with a giant mucinous cystadenocarcinoma of the ovary: A case report. J Med Case Rep 4: 82.
- De-Perrot M, Brundler M, Totsch M, Mentha G, Morel P (2000) Mesenteric cysts. Dig Surg 17: 323-328.
- Tan A, Li R, Rafique M, Oin S, Pham T (2018) A rare case of giant extra-ovarian mucinous cystadenoma arising from sigmoid mesocolon. J Surg Case Rep 3: 1-3.
- Rajshree D, Rajshree K (2016) Giant mucinous cystadenocarcinoma of ovary: A case report and review of literature. J Midlife Health 7: 41-44.
- Timmerman D, Ameye L, Fischerova D, Epstein E, Melis GB, et al. (2010) Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: Prospective validation by IOTA group. BMJ 14: 341.
- Koneczny J, Czekierdowski A, Florczak M, Poziemski P, Stachowicz N, et al. (2017) The use of sonographic subjective tumor assessment, IOTA logistic regression model 1, IOTA simple rules and GI-RADS system in the preoperative prediction of malignancy in women with adnexal masses. Ginekol Pol 88: 647-653.
- Chang HC, Bhatt S, Dogra VS (2008) Pearls and pitfalls in diagnosis of ovarian torsion. Radiographic 28: 1355-1368.
- Baradwan S, Sendy F, Sendy S (2017) Complete laparoscopic extirpation of a giant ovarian cyst in an adolescent. Case Rep Obstetr Gynecol 1-3.
- Kilinkaslan H, Cipe G, Aydogdu I, Sarac F, Toprak H, et al (2014) Pure laparoscopic management of a giant ovarian cyst in an adolescent. Am J Case Rep 15: 4-6.
- Eltabbakh GH, Charboneau AM, Eltabbakh NG (2008) Laparoscopic surgery for large benign ovarian cyst. Gynecol Oncol 108: 72-76.
- Nagele F, Magos AL (1996) Combined ultrasonographically guided drainage and laparoscopic excision of a large ovarian cyst. Am J Obstet Gynecol 175: 1377-1378.
- Tagliabue F, Acquaro P, Confalonieri G, Spagnolo S, Romelli A, et al. (2009) Laparoscopic approach for very large benign ovarian cyst in young woman. J Minim Access Surg 5: 75-77.
- Dembo A, Davy M, Stenwig A (1990) Prognostic factors in patients with stage I epithelial ovarian cancer. Obstet Gynecol 75: 263-272.
- Sevelda P, Dittrich C, Salzer H (1989) Prognostic value of the rupture of the capsule in stage I epithelial ovarian carcinoma. Gynecol Oncol 35: 321-322.
- Nishiyama T, Hanaoka K (1997) Same day drainage and removal of a giant ovarian cyst. Can J Anaesth 44: 1087-1090.