Research Article - (2016) Volume 24, Issue 5
Getinet Ayele
Community and maternal Health project officer in Save the Children in Segen People Area Zone, Sourthern Nation
Seblewengel Lemma
Lecturer in Addis continental institute of public Health, Addis Ababa, Ethiopia
Eskzyiaw Agedew*
Lecturer in Department of Public Health, Arba Minch University, Southern Ethiopia
Submitted date: August 31, 2016; Accepted date: September 13, 2016; Published date: September 20, 2016
Corresponding Author:
Eskezyiaw Getahun Adedew
PH LecturerArba Minch University
Nablis Communications and Research group
Trainings and Research Section Manager,Arba Minch,Ethiopia
Tel: +251-920413878
E-mail: esk1agid@gmail.com
Background: Pregnancy-induced hypertension is causing striking maternal, fetal and neonatal mortality and morbidity both in developed and developing countries. It represents the most common medical complications of pregnancy with a reported incidence between 5 and 10%. Therefore this study was conducted to investigate determinants of pregnancy-induced hypertension for evidence based public health intervention based on local context.
Objective: To assess factors associated with hypertension during pregnancy in Derashe Woreda.
Methods: Institutional based unmatched case control study was conducted among pregnant women who have anti natal follow up in Public Health facility of Dirashe Woreda from January 1 to February 30, 2015. A cluster sampling method was employed to recruit 117 cases (pregnancy induced hypertension mothers) and 349 controls of pregnant mothers in five public health facility based on proportional to population size allocation. Multi variable logistic regression analysis was conducted by SPSS version 20 to identify significant predictors based on p-value less than 0.05 with 95% confidence level.
Result: From all participant 117 (25.1%) were pregnancy induced hypertension groups (case) and 349 (75.1) from non-hypertension groups (controls) were involved. From all respondent 55 (11.8%) have previous history of pregnancy induced hypertension. Age of mothers between 25-30 and > 30 years Adjusted odd ratio 4.59 (1.14-18.59) and 6.59 (2.99- 14.50) respectively, lack awareness on risk of hypertension 8.24 (1.87-35.96), absence of chronic disease 0.14 (0.05-0.430), prime gravid 5.09 (1.23-21.02), frequent salt consumption 4.41 (1.25-15.56), body mass index >30 mg/kg2 9.91 (4.29-22.86), and history of previous pregnancy induced hypertension 2.85 (1.27-6.39) were identified significant factors for pregnancy induced hypertension.
Conclusion and recommendation: Special emphasis should be given for mothers who have pre existing chronic medical illness, old age and prime gravid to have early recognition and readiness for better management of pregnancy induced hyperbaton.
Keywords
Pregnancy-induced hypertension; Dirashe woreda; Case control
Background
Pregnancy induced hypertension also known as toxemia or preeclampsia is a form of high blood pressure in pregnancy and one of the leading causes of mortality and morbidity among pregnant women. Pregnancy related hypertension affect 5-10% of all pregnancies worldwide and cause a substantial maternal and prenatal morbidity and mortality. [1]
Pregnancy related hypertension occurs in about 5% to 8% of all pregnancies and more severe cases are frequently results in poor fetal and maternal outcomes both in developed and developing countries. [2,3]
Pregnancy induced hypertension is characterized by either blood pressure levels of 140/90 mm Hg or higher after 20 weeks gestation, or a blood pressure rise greater than 30/15 from early or pre pregnancy baseline or a rise of mean arterial pressure of more than 105 mm Hg. Such mild forms of PIH require close monitoring. Severe forms of PIH are reflected through blood pressure levels of 160/100 taken on 2 separate occasions, 6 h apart after bed rest. [4,5]
Globally, about 350,000 women die every year from pregnancy related causes and more than half of these deaths occur in sub-Saharan Africa (SSA). Approximately 12% of the maternal deaths are associated with hypertensive disorders in pregnancy such as pregnancy induced hypertension. [6]
Hypertensive disorders are major causes of maternal and perinatal morbidities and mortalities. Incidence of hypertensive disorders of pregnancy in India was 5.38% while preeclampsia and eclampsia accounts 44% and 40% respectively. According to a population based study in South Africa the incidence of hypertensive disorders of pregnancy (HDP) was 12%. Other hospital based studies showed the HDP was the commonest cause of maternal death which contributed for 20.7% of maternal deaths in the country. [7,8]
Studies in Ethiopia show that the incidence of hypertension during pregnancy is around 5% of which majority was due to severe preeclampsia; as study revealed eclampsia complicates 0.7% of the pregnancies. These disorders are major causes of maternal and perinatal morbidities and mortalities. The Ethiopian government plane to reduce maternal mortality due to pregnancy related complication like hypertension, pre partum and post-partum bleeding, but the incidence of hypertension and its complication on mothers and new born is prevalent as indicted by different study conducted in different parts of the country. [9-11] Even though there are few studies exploring on determinants hypertension during pregnancy in Ethiopia, there has no any study conducted yet in the current study area of interest. Therefore, this study was conducted to identify factors associated with hypertension during pregnancy.
Methodology
Study area and period
In Segen Areas People Zone (SAPZ) there are five Woreda and Derashie is one of the woreda which is from Zonal town in 60 Km and 336 Km from Hawassa city which is the Southern regional capital city. The Woreda town has two broad urban and 16 rural kebeles. The total population of the Woreda is 130,276 and number of households are 6,384. Among this population 30,354 of them are reproductive age and 4,507 is expected number of pregnancy. The Woreda surrounded by Konso in the eastern part, Gamo Goffa Zone and Amaro Woreda in the northern part and Alle Woreda in West and Southern part. In its health access there is one health post in each kebele and four health centers and one Primary Hospital managed by the Government.
Study design
Institutional based Unmatched Case control was conducted to assess factors associated with pregnancy induced hypertension in Derashie Woreda, 2015.
Cases: Were all pregnant mothers who have ANC follow up from 20 weeks gestational age and that have pregnancy induced hypertension.
Controls: Mothers who were not hypertensive (normotensive) during their pregnancy at the same period, at the same health facilities and who came for ANC follow up.
Source and study population
All pregnant mothers who came for Antenatal follow up in Derashie Woreda Public Health facility who were in 20 weeks of gestational age and above were considered as Source population where as pregnant mothers who have ANC follow up in selected five public health facility who were in 20 weeks of gestational age and above were considered as Study population.
Inclusion and exclusion criteria
Pregnant mothers who were in gestational age 20 weeks and above included in the study and known chronic hypertension mothers were not considered in study.
Sample size determination
The sample size is computed by Epi-info version 3.5.1 based on the following assumptions. A ratio of hypertension cases to controls of 1:3, power 80, confidence level 95%, and odd ratio 2 by considering for relevant factors from other studies that have significant association with hypertension. [12,13]
From the above Table 1 the final sample size was taken from Age greater than 30 years by adding 10 none response since it is maximum for case 117 and 353 for control and the total sample size is 470.
|
Relevant factors |
Expected frequency of exposure among control |
Case |
Control |
Total Sample |
|---|---|---|---|---|
|
Age>30 |
21.1% |
107 |
321 |
428 |
|
Gravidity |
38.1% |
95 |
285 |
380 |
Table 1: Sample size determination.
Sampling procedure
Cluster sampling methods was employed in a total five public Health facility based proportion to population size for case and controls in which four were health centers and one Hospital.
Data collection
Data was collected by using structured questioner and pre test before starting actual data collection. The questioner was containing written consents, socio demographic data, socio economic factors, reproductive health and feeding habits parts which were developed by adapting from different peer reviewed literatures. The interview was conducted in Amharic language by five diploma clinical nurse and supervised by three master’s public health professionals. Weights were measured at the time of data collection by portable digital Seca scale where subjects without shoes and minimally clothed. Height was measured to the nearest 1 cm and weight to the nearest 1 kg. Body mass index was calculated as weight/high. [2]
Hypertension status assessment
Blood pressure of pregnant mothers were measured manually with a validated sphygmomanometer in sitting position at the right upper arm after the mothers take rest at ANC clinic for five minutes and classify as pregnancy induced hypertension which is systolic blood pressure ≥ 140 mm Hg or diastolic pressure ≥ 90 mm Hg which occurs twenty weeks of gestational age on wards on previously normal hypertensive woman after taking three times similar measurements and considered as cases. The presence of edema at face, hands and legs was investigated by physical examination.
Data quality control
For insuring data quality training was given for data collectors and supervisor. After this Pre test of the questionnaire was conducted on 5% clients in Areba Minch town Health Center a week prior to the actual survey; and necessary modification is done according to the gap identified. Interviewee of participant was carried out in private room during ANC follow up. Data collection process was strictly followed day to day by the supervisor and principal investigators and the collected data was cheek its completeness and consistency every day by supervisors and principal investigators. Wight, height and blood pressure of every pregnant mother were measured using standard technique and calibrated equipment by adjusting for every measurement.
Data analysis
Data was coded and entered in to Epi-Info version 3.5.1 and exported to SPSS Version 20 for analysis. Exploratory data analysis was done to check missing values, potential outliers and the normality distribution for those continuous variables. Descriptive Frequencies were calculated to describe the study population in relation to relevant variables. Binary logistic regression analysis was conducted to assess the crude association between dependent and independent variables. Finally Variables which shows association in Binary logistic regression analysis and have P-value less than 0.3 entered in to Multivariate logistic regression model, to identify significant independent predictors of hypertension and to control the possible effect of confounding. Finally significant factors were identified based on AOR include in 95% Confidence level and P-value less than 0.05.
Operational definition
Pregnancy induced hypertension (PIH): Is systolic blood pressure ≥ 140 mm Hg or diastolic blood pressure ≥ 90 mm Hg at after gestation age of twenty weeks on previously normal hypertensive woman.
Preeclampsia: Which is systolic blood pressure ≥ 140 mm Hg or diastolic pressure ≥ 90 mm Hg which occurs twenty weeks of gestational age on wards on previously normal hypertensive woman with proteinuria of 1+ or 2+ on dipstick. [14]
Body mass index: Was categorized according to 2009 IOM classification: underweight (BMI<18.5), normal weight (BMI 18.5-24.9), overweight (BMI 25.0-29.9) and obese (BMI ≥ 30.0) (24) (35,36,37).
Ethical consideration
Ethical clearance was obtained from Addis Continental Institute of Public Health. Permission letter was obtained from Areba Minch University post graduate public Health coordinating office. Permission letters was obtained from Derashe Woreda Health office. Then verbal consent was taken from each participant after clearly explaining the purpose of the study. They were informed to withdraw from study at any time and/or to refrain from responding to questions if they were not interest to participate by any reason.
Result
Socio-demographic characteristics of pregnant mothers
In the present study 117 (25.1%) were pregnancy induced hypertension groups (case) and 349 (75.1) from nonhypertension groups (controls). The mean age of pregnant women was 30.88 years with + 4.53 years standard deviation. Above half mothers were in age group from 30-49 years and 205 (44%) has no formal education. Majority of mothers were 376 (80.7%) were house wife and the rest were farmer and work in private business respectively (Table 1).
Reproductive history, current and pre-existing chronic medical illness of pregnant mothers
Majority of respondent were multi gravid which accounts 364 (78.1%) and the rest were prime gravid. Majority 301 (64.6%) of pregnant mothers have > 3 times Anti natal follow up and the rest have less than 2 times. Among all mothers who has current pregnancy induced hypertension above half 53.85% of have leg edema and 2.56% have face and bilateral edema and the rest 2.69% of have edema involved face, hand and leg (Figure 1).

Figure 1: Diagrammatic presentation of sampling procedure of study conducted in Derashe Woreda.
From all participant pregnant mothers 55 (11.8%) have previous history of pregnancy induced hypertension and the rest 411 (88.2%) have no history. From all interviewed pregnant mothers 28 (6%) have chronic illness like renal disease, cardiac and diabetic disease. Of all participant 305 (65.55%) had no information about major danger sign of pregnancy. Of those who knows about danger sign of pregnancy 130 (27.9 %%) list 1-2 type and 31 (6.7%) knows 3-4 type of major danger sign of pregnancy (Figures 2 and 3).
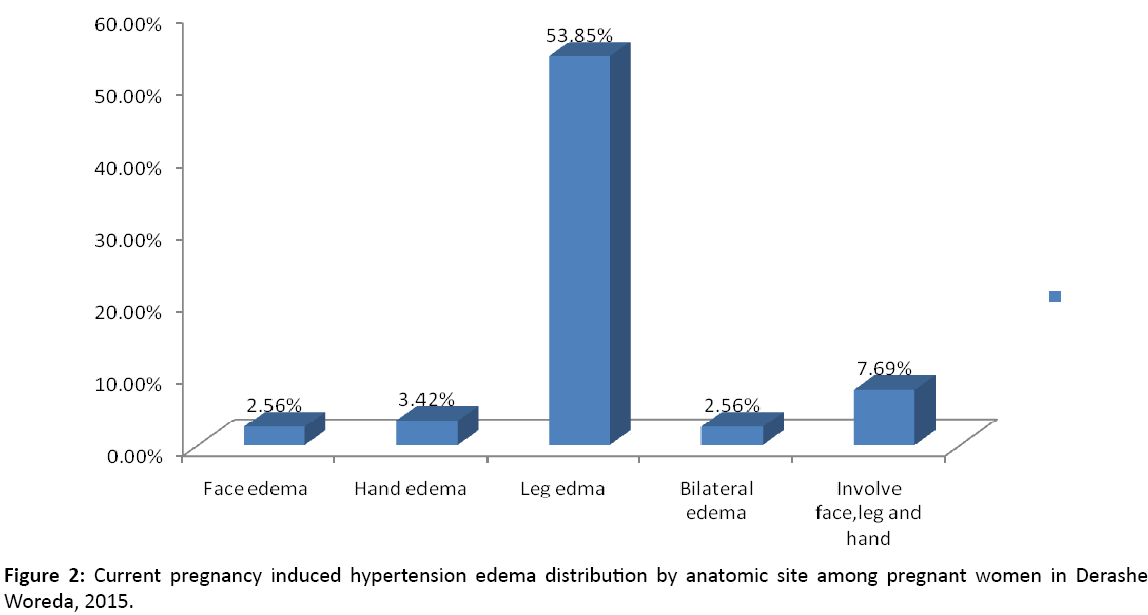
Figure 2: Current pregnancy induced hypertension edema distribution by anatomic site among pregnant women in Derashe Woreda, 2015.

Figure 3: Awareness of major danger sign of pregnancy among pregnant mothers in Derashe Woreda, 2015.
Factors associated with pregnancy induced hypertension
First Binary logistic regressions with 95% confidence level was conducted and factors that shows significant association in binary logistic and those which have p-value less than 0.3 fitted to multi variable analysis model for further identification of significant factors. Finally age of mothers between 25-30 and > 30 years AOR 4.59 (1.14-18.59) and 6.59 (2.99-14.50) respectively, those who have on awareness on risk of hypertension 8.24 (1.87-35.96), those who no chronic medical illness 0.14 (0.05-0.430), Multi gravid 5.09 (1.23-21.02), frequent salt consumption 4.41 (1.25-15.56), body mass index >30 mg/kg2 9.91 (4.29-22.86), and previous pregnancy induced hypertension history 2.85 (1.27-6.39) were identified significant factors for pregnancy induced hypertension (Tables 2 and 3).
|
Variables |
Frequency of Cases |
Frequency of controls |
Frequency Percent (%) |
|---|---|---|---|
|
Age of mothers < 25 25-30 31-49 |
5 (4.27%) 13 (11.11%) 99 (84.62%) |
42 (12.03%) 166 (47.56) 141 (40.41%) |
10.10 38.40 51.50 |
|
Level of Education No education Primary Education Secondary & above |
73 (62.39%) 34 (29.05%) 10 (8.56%) |
132 (37.82%) 175 (50.14%) 42 (12.04% |
44.00 44.80 11.20 |
|
Occupational statues Housewife Petty trader Farmer |
104 (88.88%) 8 (6.84%) 5 (4.28%) |
272 (77.94%) 64 (18.33% 13 (3.73%) |
80.70 15.50 3.90 |
|
Number of children From 1-2 children 3-5 children >5 children |
45 (38.46%) 65 (55.55%) 7 (5.99) |
294 (84.24%) 53 (15.19%) 2 (0.57%) |
72.75 25.32 1.930 |
|
Gravidity Prime Gravid Multi Gravid |
4 (3.41%) 113 (96.59%) |
98 (28.08%) 251 (71.92%) |
21.90 78.10 |
Table 2: Socio-demographic characteristics of pregnant women in Derash Woreda, 2015.
|
Explanatory Variables |
Hypertension status |
Crude OR (95% CI) |
Adjusted OR (95% CI) |
P-value |
|
|---|---|---|---|---|---|
|
|
Yes (%) No (%)
No (2) |
|
|
|
|
|
Age of mothers <25 25-30 > 30 |
5 (4.27%) 13 (11.11%) 99 (84.62%) |
42 (12.03%) 166 (47.56) 141 (40.41%) |
1 5.89 (2.25-15.44) 8.97 (4.82-16.670 |
1 *4.59 (1.14-8.59) *6.59 (2.99-4.50) |
0.03 |
|
Level of Education No education Primary Education Secondary & above |
73 (62.39%) 34 (29.05%) 10 (8.56%) |
132 (37.82%) 175 (50.14%) 42 (12.04% |
0.42 (0.17-1.05) 1.58 (0.56-4.07) 1 |
1.01 (0.26-3.87) 1.74 (0.45-6.65) 1 |
0.987 |
|
Occupational statues Housewife Petty trader Farmer |
104 (88.88%) 8 (6.84%) 5 (4.28%) |
272 (77.94%) 64 (18.33% 13 (3.73%) |
1.01 (0.35-2.89) 3.08 (0.86-10.92) 1 |
1.97 (0.49-7.94) 5.49 (0.95-31.66) 1 |
0.34 |
|
Gravidity Prime Gravid Multi Gravid
|
4 (3.41%) 113 (96.59%) |
98 (28.08%) 251 (71.92%) |
1 11.0 (3.034-30.72) |
1 *4.66 (1.19-8.17) |
0.027 |
|
ANC 1-2 visit > 3 visit |
48 (13.75%) 69 (86.25%) |
269 (77.07%) 80 (22.93%) |
1 1.38 (0.89-2.12) |
1 1.20 (0.66-2.18) |
0.544 |
|
Distance from the facility <0.5-1 hour > 1 hour |
82 (23.50%) 35 (76.50%) |
269 (77.07%) 80 (22.93%) |
1 0.69 (0.44-1.11) |
1 0.87 (0.45-1.67) |
0.681 |
|
Pervious PIH Yes No |
29 (24.79%) 88 (75.21%) |
26 (7.45%) 323 (92.55%) |
4.09 (2.29-7.31) 1 |
*2.81 (1.26-6.26) 1 |
0.012 |
|
Chronic medical illness Yes No |
21 (17.95%) 96 (82.05%) |
7 (2.00%) 342 (98.00%) |
1 0.09 (0.04-0.23) |
1 *0.14 (0.05-0.44) |
0.001 |
|
Awareness on danger sign pregnancy Yes No |
48 (41.03%) 69 (58..97%) |
135 (38.68%) 214 (61.32%) |
1 1.10 (0.72-1.69) |
1 0.78 (0.37-1.66) |
0.52 |
|
Awareness on risk HYP Yes No |
19 (16.24%) 98 (83.76%) |
21 (6.02%) 328 (93.98%) |
1 3.10 (1.56-5.86) |
1 *8.24 (1.87-5.96) |
0.005 |
|
Frequent alcohol Yes No |
21 (17.95%) 96 (82.05%) |
74 (21.20%) 275 (78.80%) |
1.23 (0.72-2.11) 1 |
0.74 (0.25-2.19) 1 1 |
0.58 |
|
Salt consumption Yes No |
11 (9.40%) 106 (90.60%) |
79 (22.64%) 270 (77.36%) |
2.8 (1.44-5.51) 1 |
4.50 (1.28-15.83) 1 |
0.019 |
|
Pregnancy BMI BMI< 30 kg/m2 BMI>30 kg/m2 |
66 (56.41%) 51 (43.59%) |
325 (93.12%) 24 (6.88%) |
1 10.46 (6.02-18.19) |
1 *9.05 (4.29-22.86) |
0.001 |
*Statically Significant factors, p-value < 0.05
Table 3: Factors associated with pregnancy induced hypertension among pregnant mothers in Desrash Worda in, 2015.
Discussion
This study focused on identifying factors affecting pregnancy induced hypertension in pregnant women. Age of mothers who were in age range 25-30 years and greater than 30 years AOR 6.59 (2.99-14.50) and 4.59 (1.14-18.59) respectively, Multi gravid AOR 5.087 (1.23-21.02) times more likely develop pregnancy induced hypertension (PIH) as compared to their counter parts. This finding is in line with study conducted Borka and others related studies. [12,14,15] As study conducted in Boreka extreme age of mothers and multiple pregnancies has effect on hypertension during pregnancy.
Pregnant mothers who have pervious history of pregnancy induced hypertension AOR 2.85 (1.27-6.387) more likely develop PIH as compared their counter parts. This finding is consistent with study conducted systematic review of controlled trials studies. [14] Women who have history of hypertension in the first pregnancy have seven times more likely developing preeclampsia in a second pregnancy and the risk is increase as there pregnancy increase. [13,16] In this study Women who have no preexisting medical conditions like renal and cardiac disease were 86% less likely develop PIH as compared to with those who have pre-existing medical conditions this supported with study done in Asian population and others related study. [14,17,18]
Pregnant mothers who h as no awareness on risk hypertension 8.24 (1.89-35.96) and frequent salt consumption 4.41 (1.25-15.54) more likely develop PIH as compared to their counter parts. This result is in line with study conducted in different setting. [19,20] Existing evidence suggests that a high dietary intake of salt may contribute to the rise in blood pressure and can promote the development of hypertension, or aggravate hypertension already present.
Maternal body mass index >30 kg/m2 9.90 (4.29-22.86) times more likely develop pregnancy induced hypertension as compared to their counter parts. As Maternal body mass index increase the risk of hypertension typically doubled with each 5–7 kg/m2 as indicated in different literatures.21,22 In a systematic review of 13 cohort studies reveals that linear rise in the risk of preeclampsia with increasing pregnancy BMI.
Conclusion
The current study shows that all mothers who have current pregnancy induced hypertension above half have leg edema. There is lack of awareness on major danger sign of pregnancy like vaginal bleeding, bilateral edema, convulsion and fever and headache. Age of mothers between 25-30 and > 30 years, those who have on awareness on risk of hypertension, those who has chronic medical illness, prime gravid, frequent salt consumption , body mass index >30 mg/kg2 , and history of previous pregnancy induced hypertension were identified significant factors for pregnancy induced hypertension.
Recommendation
For health professional and health extension workers
Special emphasis should be given for mothers who have pre existing chronic medical illness, old age and prime gravid to have early recognition and readiness for better management of pregnancy induced hyperbaton.
Health education should be given for mothers during ANC especially on danger sign of pregnancy and reducing feeding of foods that aggravate hypertension during pregnancy like excesses intake of salt.
For researchers
Further research should be conducted to see the effect of pregnancy induced hypertension on birth outcome.
Acknowledgement
We would like to thank Arba Minch University and addis continental institute of Public Health for giving a chance to conduct this research and to our collogues for their generous assistance and valuable comments throughout this research work. Also our heart-felt gratitude goes to Dirashe Woreda health office for their support in provision of health related information.
Authors’ Contribution
GA: Initiated the research, wrote the research proposal, conducted the research, did data analysis and wrote the manuscript. SL: Involved in the write up of methodology of proposal and research work. EA: Contributed in the designing of methodology and write up of proposal and wrote up of the manuscript.