Research Article - (2015) Volume 23, Issue 2
Department of family medicine, Université de Sherbrooke, New Brunswick Canada Centre de formation médicale du Nouveau-Brunswick, New Brunswick Canada Vitalité Health Network, New Brunswick Canada
Edith Couturier, MD
Department of family medicine, Université de Sherbrooke, New Brunswick Canada
Natacha Dion, MD
Department of family medicine, Université de Sherbrooke, New Brunswick Canada
Vanessa Girouard, MD
Department of family medicine, Université de Sherbrooke, New Brunswick Canada
Jessy Phillips, MD
Department of family medicine, Université de Sherbrooke, New Brunswick Canada
Jennifer Brunet, Ph.D
School of Human Kinetics, University of Ottawa, Canada
Background: Although prior research has shown that physicians perceive various barriers that hinder the systematic promotion of physical activity in practice, no study has contrasted the barriers reported by physicians who regularly prescribe physical activity with those who are not prescribing it.
AIM: The aim of this qualitative study was to explore barriers and enablers to prescribing physical activity in primary care among family physicians who are currently prescribing it and those who are not.
METHODS: This study used quantitative, to assess physicians’ prescribing behavior, and qualitative, to identify barriers and enablers within each group, methodologies. Participants were drawn from a web-based survey. For the current study, identified family physicians prescribing physical activity (n=3; prescribers) and not prescribing it (n=6; nonprescribers) participated in a face-to-face semi-structured interview. Interviews were audio-recorded and transcribed verbatim. Thematic analysis was employed in which four researchers independently identified barrier and enabler themes.
RESULTS: Various barriers hindering physical activity prescriptions were reported by both groups of physicians, with some differences noted across groups. Cross-group comparisons also led to the identification of enablers among prescribers. These included awareness of the value of physical activity prescription, positive attitude toward physical activity, recognizing physical activity prescription as part of family medicine, having access to resources (e.g., physical activity prescription pads), and developing resiliency against patient rebuttal and non-compliance.
CONCLUSION: This study improves our understanding of the barriers encountered by family physicians to prescribing physical activity in primary care. Focusing on the enabling factors elucidated in this study may help family physicians counter perceived barriers and increase physical activity prescription rates
Exercise, Prescriptions, Primary Care, Physicians, Qualitative Research
How This Fits in with Quality in Primary Care
What do we know?
• Family physicians consider lifestyle counseling an important part of their work; however, only a small number promote physical activity by prescribing it in primary care.
• Barriers to prescribing physical activity include physicians’ perceptions that patients are ambivalent about behavior change and lack motivation to change their behavior, as well as lack of time, knowledge, and skills.
What does this paper add?
• In addition to identifying barriers similar to those reported in earlier studies, this study innovates by contrasting barriers with enablers of physical activity prescription derived from the reported experiences of prescribers.
• Enablers identified that could help non-prescribers overcome perceived barriers to prescribing physical activity appear simple to implement. They include increasing awareness of the value of physical activity prescriptions, nurturing positive attitudes toward physical activity among family physicians, demonstrating how physical activity prescription can be integrated into habitual practice, providing resources which can ease practice, and developing resiliency against patient rebuttal and non-compliance.
Estimates suggest that if Canadians adhered to current physical activity recommendations [1], there would be a 33% decrease in coronary heart disease-related deaths, a 25% reduction in deaths related to stroke and osteoporosis, 20% less deaths due to colon cancer, hypertension, or type 2 diabetes, and about 15% fewer deaths related to breast cancer [2]. The benefits of physical activity nevertheless extend beyond primary prevention. For example, physical activity has been shown to effectively reduce blood pressure in hypertensive patients [3], reduce overall and cardiovascular mortality in cardiac patients [4], reduce disability in stroke patients [5], reduce glycemic index in diabetic patients [6], decrease pain symptoms in patients with osteoarthritis [7], reduce depressive symptoms in psychiatric patients and the general populations [8], lower risk of falls among osteoporosis patients [9], improve motor action, balance, and gait in patients with Parkinson’s Disease [10] and improve quality of life among patients with Chronic Obstructive Pulmonary Disease [11] and rheumatoid arthritis [12]. In addition to its therapeutic benefits, which in some cases are of magnitude stronger or comparable to pharmaceutical therapy [13], physical activity has the advantages of having a low potential for harmful side effects and of exposing patients to benefits positively affecting numerous health conditions [14]. This is significant given the high prevalence of patients with multimorbidity [15]. Consistent with numerous clinical guidelines [16–20], physical activity should therefore be considered as a first-line therapeutic approach and prescribed in primary care.
Considering that over 75% of the population consult their primary care provider annually [21–23] and that patients perceive physicians as the most reliable source of information for physical activity [24] , there is potential for family physicians to play an important role in the promotion of physical activity [25]. Furthermore, previous results indicate that patients expect health-behavior related information from their primary care providers and that physician advice can be a strong external cue for health-promoting actions [26]. However, although family physicians consider lifestyle counseling as an important part of their work [27], only 16% of family physicians in Canada promote physical activity by prescribing it in primary care [28].
In order to change professional practice, it is important to assess physicians’ barriers to the systematic promotion of physical activity in primary care. Previous research has shown that barriers include physicians’ perceptions that patients are ambivalent about behavior change [29–31] and that they lack motivation to change their behavior [32]. Other barriers reported include lack of time, knowledge, and skills [32–38]. In order to build on these findings, studies are needed to explore what distinctions exist in the barriers to physical activity promotion between physicians who regularly prescribe it and those who do not. This will help to understand which barriers may have an impact. Focusing on these two groups will also enable the elucidation of strategies helping physicians to overcome barriers to physical activity prescription. As part of an effort to improve physical activity promotion in primary care, we explored barriers and enablers to prescribing physical activity among family physicians who currently prescribe it and those who do not.
Following ethics approval from the Vitalité Health Network institutional review board, we conducted a study using quantitative and qualitative methodologies. Quantitative methods were used first to assess physicians’ prescribing behavior (Phase I), followed by a qualitative component, which sought to identify barriers and enablers within each group (Phase II). Participants agreeing to participate in this study provided informed consent before data collection began.
Phase I: Web-based survey
In Phase I, 387 physicians listed in a provincial medical training program mailing list were invited to take part in a web-based survey to assess whether they were prescribing physical activity. For this, participants were provided the following statement: “Based on best evidence for exercise prescription and a review of most feasible exercise prescription practices in clinical settings, it is recommended that doctors use the following practice principles. STEP 1: Discuss the benefits of physical activity and establish realistic individualised goals with the patient. STEP 2: Hand out a written physical activity prescription which specifies frequency, intensity, type, and duration” [39]. They were then asked: “Do you regularly recommend physical activity in writing to most of your patients using the principles stated above?” The five response options were: 1 = NO, and I do NOT intend to in the next 6 months; 2 = NO, but I intend to in the next 6 months; 3 = NO, but I intend to in the next 30 days; 4 = YES, I’ve been doing it for LESS than 6 months; 5 =YES, I’ve been doing it for MORE than 6 months. These represent the pre-contemplation, contemplation, preparation, action, and maintenance stages of change in the Transtheoretical Model of Health Behavior Change [40], respectively. Data on participants’ age, sex, medical speciality, average number of patients seen per day in the office, and physical activity level were also collected as part of this survey. Clarity of all items in the questionnaire was confirmed through a pilot test among five physicians.
Phase II: Individual interviews
In keeping with the notion of theoretical sampling, family physicians categorized as pre-contemplators (n=7) and maintainers (n=4) were invited to participate in a face-to-face, semi-structured interview because they represent non-prescribers and regular prescribers, correspondingly. Interviewers (EC, ND, VG, JP) initiated interviews with general introductory questions to help establish rapport and confirm proper categorisation of participants. The interview guide followed during the interviews also included open-ended questions and probes to explore perceived barriers and enablers associated with the adoption of a medical practice implementing physical activity prescription. Based on prior research [29,31,32] and theories of behavior change [41–44], the questions were created to cover a range of factors that can affect implementation of practice guidelines, including physicians’ expectancies regarding the outcomes of their behavior, attitudes toward the behavior, normative beliefs, and perceived behavioral control. In this sense, it served as a checklist of points for discussion, but the interviewers allowed flexibility in the direction participants would take the discussion. Sample questions are: “What do you think about evidence suggesting prescribing exercise?” and “What could be barriers or facilitators for you to integrate exercise prescription in your practice?” Interviews lasted between 25 and 45 minutes (average = 32 minutes). All interviews were audio-recorded and transcribed verbatim.
Data analysis
Data gathered were analyzed using thematic analysis, which is a search for themes that emerge as being important to describe the phenomenon under investigation [45]. It incorporated both techniques of deductive and inductive analysis. Specifically, it allows for the identification of themes based on existing theoretical concepts and concepts identified in the literature through the process of deductive coding as well as for themes to emerge directly from the data using inductive coding. For this study, four researchers (EC, ND, VG, JP) independently engaged in the coding process to identify subthemes by carefully reading and re-reading the transcript to recognize patterns in the data [46]. Next, they grouped related subthemes together. Any discrepancies were resolved through discussions and consensus was reached. There was variability in the order in which researchers analysed the transcripts. This allowed noting evidence of data saturation as there were no new themes identified from the last interviews analysed by each researcher. The next step involved selective coding whereby related subthemes were combined into core concepts, (i.e., higher-order themes) based on both theoretical propositions and existing studies [47]. During this stage, particular attention was paid to identify similarities and differences between the two groups of physicians. In the final stage, a fifth researcher (MB), who had not yet been involved in the analysis, reviewed the final coded data to ensure the higher-order themes were representative of the raw data. His assessment was in agreement with the coding scheme, which provides interpretative validity and enhances the credibility and trustworthiness of the findings reported in this study.
Responses from 29 family physicians who completed a web-based survey were used to identify potential participants for the qualitative component of this study. They ranged in age from 32 to 61 years (mean = 41 years). All were White, more than half (n = 16) were women, less than half (n = 13) reported adhering to the recommended ≥ 150 minutes of moderate or vigorous physical activity per week, and 13 were paid through a fee for service scheme. They reported seeing between 11 and 40 patients per day (average = 25 per day). Of these 29 family physicians, 3 out of the 4 prescribers and 6 out of the 7 nonprescribers were interviewed. The interviewed participants ranged in age from 32 to 61 years (mean = 43 years), most (n = 6) were women, less than half (n = 3) reported adhering to the recommended ≥ 150 minutes of moderate or vigorous physical activity per week, and six were paid through a fee for service scheme. They reported seeing between 16 and 35 patients per day (average = 22 patients per day). There were no apparent difference in the distribution of these characteristics between prescribers and non-prescribers.
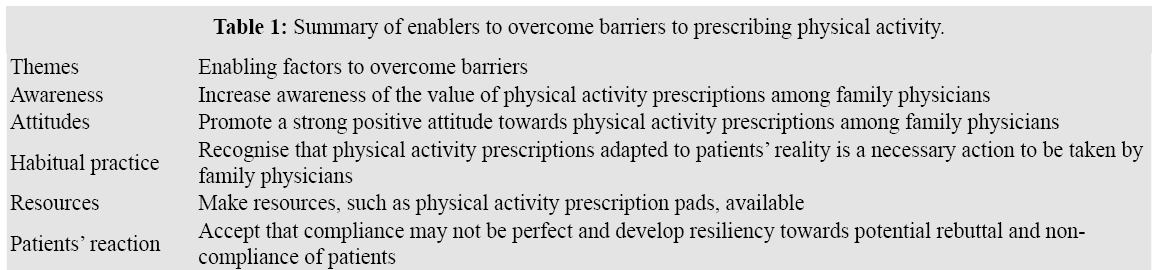
In total, five themes relating to barriers and enablers were identified: (1) Awareness of the value of prescribing physical activity, (2) Attitudes toward physical activity, (3) Habitual practice, (4) Resources can affect practice, and (5) Patients’ reaction guide physicians’ behavior. These themes are summarized in Table 1. Each theme is described below, along with supporting quotations. Citations were translated from French to English at the time of manuscript writing and pseudonyms were used in lieu of real names to protect participants’ anonymity.
Awareness of the Value of Prescribing Physical Activity
One of the findings relates to the positive effect of participating in this study on creating awareness about the value of prescribing physical activity. By being asked to reflect on their current practices and the potential value of incorporating physical activity prescriptions, we noted that non-prescribers started to transition from pre-contemplation (i.e., not interested in incorporating physical activity prescription in their practice in the foreseeable future) toward contemplation (i.e., starting to consider that incorporating physical activity prescription in their practice would be possible and could be beneficial) or preparation stages (i.e., intending to incorporate physical activity prescription in their practice in the foreseeable future). We also saw that as participants acknowledged the value of physical activity prescriptions, they found themselves thinking about changing their practice. For example, many non-prescribers mentioned something like the following:
« Yes, I think it’s a good idea. I would really like to try it. »
(non-prescriber: Janice)
Given these observations, it is possible that physicians’ lack of awareness about physical activity prescription constitutes an important barrier to prescribing it in primary care. However, not all non-prescribers were ready to start prescribing physical activity. Some physicians expressed doubt toward the potential added benefit of presenting patients with such a prescription. For example, statements like the following reinforce the idea that a lack of awareness may be a barrier:
« I really wonder if writing a prescription will be more beneficial.» (non-prescriber: Martin)
Attitudes toward Physical Activity
Regardless of whether physicians were prescribers or non-prescribers, they had good knowledge of health benefits associated with physical activity, and this ultimately enhanced their willingness to prescribe it. Participants in this study presented a positive attitude towards the value of an active lifestyle. Both groups of physicians also highlighted that it was an important part of physicians’ role to recommend to their patients to engage in physical activity as can be summarised by a quote from a non-prescriber:
« It’s really important, especially for us in family medicine. It’s kind of our job to encourage our patients to exercise. I would say it’s one of the primary first-line treatments. » (non-prescriber: Stephanie)
The attitudes of prescribers were nevertheless stronger than those of non-prescribers. They talked with more conviction and clearly expressed ranking exercise as a first line treatment option. This strong positive attitude appeared to be a factor enabling prescribers to adhere to a practice incorporating the prescription of physical activity:
« I tell patients it’s like the super pill! Exercise is the strongest pill we can prescribe and it’s also the one with the least side effects. » (prescriber: Robert)
« In my view, it’s a priority. I think it’s one of the first interventions we should recommend for many health problems. » (prescriber: Isabel)
In a similar vein, physicians in the prescribers group expressed a belief that prescribing physical activity was a concrete way for them to prompt their patients to engage in physical activity:
« I think a formal and concrete recommendation tends to have more of an impact than simply saying it verbally. I think the patient will remember it better. » (prescriber: Monique)
In addition, prescribers highlighted that prescribing physical activity in writing was a way for them to stress the seriousness of their physical activity advice to patients and ensure their patients understand that it is an integral part of their medical treatment. They also viewed the action of providing it in writing as a mechanism to help patients retain the information that was discussed during their appointment.
« The patient likes to have a prescription. He likes to have a piece of paper when he leaves the doctor’s office. The patient also retains more information if you give it in writing. » (prescriber: Robert)
These benefits were also perceived by non-prescribers who had not given much thought to the idea of prescribing physical activity in their practice before taking part in this study. For example, one non-prescriber now considering adopting the practice expressed that the prescription could serve as a good reminder and motivator for patients to take part in physical activity.
« Perhaps the patient would take it more seriously because we actually took the time to write it down. He could put the prescription on his refrigerator as a reminder. It’s more visual, more objective and more concrete. » (non-prescriber: Amy)
Habitual Practice
Family physicians in the non-prescribers group said they mentioned the importance of physical activity to their patients during their appointments on a regular basis. Although they did not prescribe physical activity in a written format, non-prescribers still said they included physical activity-related verbal encouragements or advice in their treatment plans for patients, as mentioned by this non-prescriber:
« Any chance I have to talk about it, I will talk about it. » (non-prescriber: Janice)
Both groups of family physicians reported providing physical activity advice to patients who had one or more existing chronic health condition. Most times though, physical activity was discussed with patients as a therapeutic option, and less frequently in terms of prevention. Types of health conditions for which physicians more strongly appeared to associate physical activity included hypertension, type 2 diabetes, dyslipidemia, and obesity. Chronic pain and mental health conditions such as depression and anxiety were also listed.
Family physicians from both groups also shared similar views regarding the necessity to adjust their intervention in function of patients’ own readiness to change their physical activity behavior. They mentioned needing to take consideration of patients’ readiness to be active, as well as their interests, goals, and needs based on health status and physical function as expressed by a non-prescriber and a prescriber:
« We have to adapt to the individual. Some will never be able to jog, but swimming may be excellent for them. We try to identify the patient’s interests. We motivate patients according to their interests. » (prescriber: Robert)
«If the patient does not exercise, but is able to, I explore what would be a reasonable objective for him. I want to introduce physical activity progressively with realistic individualized objectives. The patient has to find what he wants to do. » (nonprescriber: Janice)
An element of distinction between the two groups was how prescribers were ready to address challenges associated with prescribing physical activity. Whereas non-prescribers quickly identified many other elements they need to address during appointments with their patients as a barrier, prescribers embraced the action of writing physical activity prescriptions as one of the many things they need to address as physicians. It appeared as if an enabling element for prescribers was simply that their general functioning habits is inclusive of the practice of prescribing physical activity. This can be illustrated by these contrasting quotes from a prescriber and a non-prescriber:
«It’s the way I operate (written prescription) for most other things than physical exercise, so that could be the factor that entices me to also use it for physical activity. » (prescriber: Monique)
« It would often be forgotten because we have many other recommendations to act upon. » (non-prescriber: George)
Resources can Affect Practice
Family physicians, whether in the group of prescribers or non-prescribers, did not feel they lacked time to prescribe physical activity to their patients. They reported that it could be done rather quickly, as stated by two physicians:
« We could say it’s 20 more seconds every time we write a prescription, but I don’t think it’s significant in terms of time. » (non-prescriber: Amy)
« I find it’s the extra 15 seconds, 30 seconds, maximum 1 minute that we can take and which will make a difference for the patient. » (prescriber: Monique)
Interestingly, prescribers felt that a lack of resources presented a challenge to a more widespread use of physical activity prescriptions among family physicians. Prescribers further noted that considerable concerted and coordinated efforts would need to be invested in order to change their colleagues’ perceptions that incorporating physical activity prescription is secondary to their other responsibilities in primary care. Despite already adhering to the practice, one prescriber expressed that even those who commonly prescribe physical activity could benefit from such efforts. This prescriber believed that making it the norm to prescribe physical activity would alleviate some of the perceived barriers:
« I think we will need to redouble our efforts and dedication in order to integrate it all. Having strategies and tools to help with having more time and energy to integrate it into our practice will help us implement it with our patients. » (prescriber: Isabel)
In that sense, one prescriber explained having prepared summary sheets for his patients and using prescription pads specifically designed for physical activity prescription. Not knowing that such resources existed, this was a solution suggested by family physicians in the non-prescribers group:
« Perhaps a pre-prepared pad we could use with some color so as to make it easier for us and easier for the patient to understand. Something standardized would be a good idea! » (non-prescriber: Stephanie)
Patients’ Reactions Guide Physicians’ Behavior
Non-prescribers highlighted that an important barrier for them to make use of physical activity prescriptions was the fear of potential patients’ rebuttal and non-compliance. They described this as a frustrating process during which they would anticipate a lot of resistance. They stated that it would be difficult to prescribe physical activity because it is hard to get patients to understand that it represents a beneficial nonpharmacological treatment option. It is notable that these beliefs that seemed to hinder non-prescribers’ motivation to prescribe physical activity, did not originate from their own experience. Rather, they identified these barriers by predicting patients’ reactions and by referring to experiences they had heard of from colleagues as stated by this non-prescriber:
« I think it’s because of the unknown. I’ve heard from a few people that have done it and it seems to me that the patients didn’t take it well. For me it’s really that kind of reluctance that prevents me from doing it... Will they (patients) do it? That’s the big stumbling block for me. » (non-prescriber: Martin)
Along similar lines, prescribers mentioned that patient compliance was sometimes disappointing. The disappointments were never expressed in the context of patients’ reception of their advice or prescriptions, but rather with regards to patients’ occasional poor adherence to their recommendations. Specifically, prescribers conveyed that it was sometimes difficult to accept that patients would not benefit from their intervention because of their lack of adherence to the prescribed therapy. The prescribers articulated having developed resiliency around this issue. They discussed that imperfect adherence is a reality for any type of treatment option, and that compliance to physical activity prescription is not very different than compliance to other interventions. They talked about persevering with physical activity prescriptions for the greater good of many patients:
« Sometimes it’s disappointing, but we must not give up. » (prescriber: Robert)
In this study, we examined barriers and enablers to prescribing physical activity in primary care among family physicians who currently prescribe it and others who do not. Although the latter group was not actively prescribing physical activity to their patients, all family physicians interviewed had very positive attitudes in relation to the value of physical activity. Further, even non-prescribers reported addressing the subject of physical activity with their patients, which is consistent with a national survey reporting the same practice in over 85% of family physicians in Canada [28]. However, contrasting experiences and positions were noted between physicians prescribing physical activity in their medical practice and those who did not.
One unanticipated finding of this study is that being prompted to think about one’s current physical activity prescribing practices increased family physicians awareness of the value of prescribing it. Further, this ultimately led to the considerations about prescribing it amongst non-prescribers. Thus, it is conceivable that increasing family physicians awareness of the value of prescribing physical activity may lead to increased prescription frequency.
Although the benefits of physical activity were well recognised in our sample of family physicians, our findings suggest that this type of knowledge is not necessarily associated with writing physical activity prescriptions. Given previous studies showing that written prescriptions for physical activity in primary care can have a significantly positive influence on patients’ physical activity level and related fitness markers [37,48–53] and prospective studies with pragmatic prescription interventions reported significant positive shifts in readiness for changes as well as increases in physical activity levels and improved quality of life among patients [50,51,54,55], strategies are needed to increase written prescription frequency. Based on the current findings, it may be valuable for strategies to focus on informing family physicians of the actions they can take to increase their patients’ physical activity and their effectiveness rather than conveying the already known general benefits of physical activity on health.
Consistent with previous reports [37,56–58], our findings suggest that written physical activity prescriptions can represent concrete indications for patients to realise that their care provider is serious about his or her recommendations. They also suggest that written prescription can act as a reminder for patients to engage in and maintain motivation for physical activity. Previous studies show that physical activity prescriptions for patients with low level of physical activity can lead to sustained increases in physical activity, with adherence rates exceeding 50% at 3, 6 and 12 months of follow-up [51,54]. These rates are comparable to compliance rates generally observed for common medical actions including adherence to prescription of pharmacological medication in long-term treatment of chronic illnesses such as hypertension at 50% [59–61], asthma at 43% [62], depression at 40 to 70% [63] and diabetes at 36 to 93% [64].
Beyond recognising the value of using written prescriptions to promote physical activity, prescribers were distinguishable from non-prescribers in this study in the way they described their practice. For prescribers, it appears that prescribing physical activity may be a natural way of practicing medicine in that it was viewed as an integral part of their practice. In fact, despite experiencing barriers, they conveyed that obstacles to prescribing physical activity simply had to be dealt with. They also expressed that it was not different from the other medical acts which involve providing prescriptions. This is in line with Scandinavian studies suggesting that physical activity prescriptions can be effectively integrated in routine primary health care when treated the same way as conventional treatment options [50,51,65]. In that sense, clinical guidelines suggesting that physical activity be included as part of treatment plans 16–20 could become more specific by suggesting that patient-physician discussions around physical activity include the act of writing a physical activity prescription and handing it to patients.
In contrast with other studies suggesting that time constraints represent an obstacle to a more widespread use of physical activity prescriptions, [33,34,36,37] we did not identify time as a barrier. This may relate to the observation that although non-prescribers did not use written prescriptions, they reported addressing the topic of physical activity with their patients, such that translating this into filling in a prescription would not require substantially more time. It was nevertheless highlighted that providing resources to ease the process of preparing written prescriptions for physical activity and making it more time effective might be beneficial. To this effect, prescription pads specifically designed to ease the preparation of physical activity prescriptions for patients are now widely available from groups such as Exercise is Medicine and provincial medical societies [66,67]. Furthermore, increasing opportunities to learn about these resources and to acquire skills necessary to use them effectively should be integrated in education programs. Along these lines, groups such as the Canadian Medical Association [68], the American College of Preventive Medicine [25], the Royal College of Physicians [69], the Bipartisan Policy Center in collaboration with the Alliance for a Healthier Generation and the American College of Sport Medicine [70] have called for training on physical activity counselling to be implemented across the education spectrum, including in undergraduate medical programs, residency training, and continuing medical education programs. These actions are important in light of evidence which shows that physicians’ attitudes, knowledge, and behaviors can be shaped through their training, and that they are strong determinants of whether patients will or will not receive physical activity counselling or prescriptions [34,71–73].
Whereas fear of potentially negative reactions from patients was a reason non-prescribers gave for not prescribing physical activity in their practice, prescribers described that they had developed acceptance of the fact that not all patients would be interested in receiving advice on physical activity or would adhere to their recommendations. A number of enablers helped prescribers to deal with the potential for rebuttal from patients. First, prescribers recognised patients among whom it would be worthwhile to prescribe physical activity by investigating their stage of readiness for change. While it is accepted that pre-contemplators are not ready for and should not be forced into behavior change, a shift to action may be attempted among patients in the stages of contemplation and preparation [50]. Second, and consistent with best practice recommendations [39,74], prescribers adapted their physical activity prescription to meet the needs of patients based on factors such as habitual physical activity, physical function, health status, activities of interest, and stated goals. Third, prescribers prepared themselves to accept imperfect adherence by recognizing that compliance to physical activity prescription is not very different from compliance to other interventions. These enablers provide new insight into how to potentially increase physical activity prescription rates and effectiveness.
A particular strength of the present study was that in addition to identifying barriers similar to those reported in earlier studies, the methodology employed enabled us to contrast them with enablers derived from the reported experiences of prescribers. This study nevertheless has some limitations. The low proportion of respondents to the web survey limits our ability to use responses to the web-survey to draw any sort of generalisations. This has minimal implications on our present results since the aim of the survey was simply to identify participants who may become eligible for the qualitative component (Phase II). Further, and inherent to any qualitative research, it is possible that our results do not transfer to other populations. However, having reached saturation of themes suggests attainment of acceptable content validity [75]. Finally, the potential for social desirability to have influenced responses of participants must be considered.
In this study physicians who currently prescribe physical activity in their medical practice identified enablers which could help non-prescribers overcome perceived barriers to prescribing physical activity. Specifically, results suggest that it may be possible to increase physical activity prescription rates by increasing awareness of the value of physical activity prescriptions, nurturing positive attitudes toward physical activity among family physicians, demonstrating how physical activity prescription can be integrated into habitual practice, providing resources which can ease practice, and developing resiliency against patient rebuttal and non-compliance. Interventions integrating these strategies should be tested to evaluate their effectiveness in an effort to improve physical activity prescriptions rates in primary care.
This manuscript was prepared while JB was supported by a Canadian Cancer Society Career Development Award in Prevention.
All authors meet standard authorship criteria. MB conceived the objectives of the analysis, interpreted the data, and wrote the manuscript. EC, ND, VG and JP contributed to the acquisition, analysis and interpretation of data. JB provided help during the stages of data interpretation and manuscript writing. All of the authors contributed in the conception of the work and reviewed the manuscript critically for important intellectual content and approved the final version to be published.