Keywords
α-smooth muscle actin; FGF-1; Human lung fibroblasts; MEK signaling
pathway; MMP-1; Type I collagen; P38 signaling pathway; PI3K signaling pathway;
TGF-β/Smad signaling pathway
Introduction
Fibroblasts are the main mesenchymal cells found in connective
tissues and synthetize, secrete and turnover several molecules
of the extracellular Matrix (ECM), including structural proteins,
adhesive proteins, glycosaminoglycans and proteoglycans
[1]. Fibroblasts are involved in all ECM physiological and
pathophysiological procedures and participate actively in idiopathic pulmonary fibrosis (IPF), a frequent interstitial lung
disease (ILD). IPF is a progressive, irreversible, and lethal lung
disease characterized by the expansion and prevalence of
activated fibroblasts and myofibroblast subpopulations, which
accumulate focally. These cells develop an active and abnormal
ECM remodeling and participate in their increase, finishing
eventually with an exaggerated accumulation of ECM and
irreversibly altering the lung histo-architecture [2].
Abnormal ECM turnover in IPF is dependent on fibroblast and
myofibroblast subpopulations, including the downregulation
of matrix metalloproteinase(MMP-1), and the upregulation of
collagen and alpha-smooth muscle actin (α-SMA), a hallmark of
myofibroblast differentiation; all these processes are mediated
predominantly by TGF-β1 stimulation, recognized as the foremost
profibrogenic cytokine in different organs [3]. Therefore, fibroblast
and myofibroblast subpopulations play a pivotal role in fibrotic
diseases, such as IPF, as these cells are involved in the turnover of
the ECM and may exhibit fibrogenic activity [4]. Myofibroblasts
can derive from classic interstitial fibroblasts and from type II
alveolar epithelial cells by epithelial-mesenchymal transition
and possess an ECM secretory phenotype. In lungs, they mainly
synthetize I and III type collagens in a 3:1 proportion and other
molecules [5]. On the other hand, we have found that the acidic
fibroblast growth factor (FGF-1) combined with heparin (FGF-
1/H) chains several antifibrogenic effects, antagonizing the profibrogenic
activity of TGF-β1 in fibroblasts obtained from human
lung fibroblasts (HLF). Some of these effects observed in HLF in
vitro include the upregulation of MMP-1, the downregulation of
collagen I and TGF-1-induced α-SMA [6,7]. Similar results have
been demonstrated in a pulmonary fibrosis model in female
Sprague-Dawley rats in vivo, where lung fibrosis was attenuated
when prolonged transient overexpression of FGF-1 (AdFGF-1)
and TGF-β1 (AdTGF-β1) using adenoviral vectors was used [8].
In this model, the FGF-1 had preventive and therapeutic effects
on TGF-β1-induced lung fibrosis by inhibiting myofibroblasts
differentiation and the proliferation of alveolar epithelial cells,
by downregulating TGF-1, and degrading transforming growth
factor-β receptor type 1 (TBRI), through the inhibition of
Smad2/3 phosphorylation [8]. Furthermore, signaling pathways
activated by FGF-1/H to upregulate MMP-1 and to downregulate
collagen I and α-SMA are only partly understood. Consequently,
we studied the signaling pathways activated by FGF-1/H in HLF
that upregulate MMP-1 and downregulate collagen I and TGF-
β1-induced α-SMA expression. We hypothesized that FGF-
1/H activates different signaling pathways that regulate the
expression of MMP-1 and collagen I or inhibit the upregulation of
α-SMA induced by TGF-β1 in HLF.
Different aspects were taken into account for the development
of the present work. Mainly, the fact that physiopathogenetic
mechanisms involved in IPF are complex and involve different
physiological mediators such as cytokines, chemokines,
interleukins and growth factors that, in turn, activate several
signaling pathways, including MEK, JNK, p38, pI3K and TGF-β/
Smad. The latter stimulate fibroblasts, myofibroblasts and
type II cells subpopulations characteristic of IPF, a non inflammatory disease [1-3]. Besides, FGF-1 can activate all these
pathways independently of the cellular type, interacting with
all the receptors of the FGF family (FGFR1-4), thus efficiently
participating in the modulation of the metabolic turnover of the
ECM [9]. Also, FGF-1/H anti-fibrous potential, as evidenced both
in vitro and in vivo [6-8], can lower the expression of collagen,
especially type I, the most abundant protein in fibrous lung tissue.
It also increases the expression of MMP-1, that constitutes the
initial degrading enzyme of type I fibrillar collagen in the native
state [2,3], and decreases the expression of α-SMA, essential
in the trans-differentiation of fibroblast into myofibroblasts
[1,5]. Consequently, our interest was to find out which of these
signaling pathways were activated in fibroblasts to promote the
expression of these three proteins. To achieve this goal, we used
a cellular model that can broaden our knowledge of the role of
FGF-1 in the pathophysiology of IPF. Patients affected by this
illness generally die between 3 to 5 years after the appearance of
the first respiratory symptoms [2,3,10], a fact that clearly points
out the relevance of this research. We expect that, by integrating
the results obtained herein with the previous information of the
anti-fiber potential of FGF-1, novel research will be developed to
finally find an effective therapy for this illness.
Research Methodology
The aim of this research was to determine the signaling pathways
stimulated by FGF1/H in fibroblasts derived from human lung
that upregulate MMP-1 and downregulate collagen I and TGF-
β1-induced α-SMA expression. To achieve this goal, the following
experimental approaches were designed.
Fibroblasts obtention from human lung
Human lung fibroblasts (HLF) in passage 4-6 (n=3), were obtained
as described elsewhere [6,7]. In brief, the fibroblasts were
obtained from samples of lung tissue via the open lung biopsy
from normal areas from patients with lung cancer and cultured in
Ham's F12 (F-12 Nutrient Medium), supplemented with 10% FBS.
Experiments were performed when cells reached 70% confluence
while cultured in serum-free media (SFM). In all experiments the
cells were then treated with 20 ng/ml recombinant human FGF-
1 (R&D, Minneapolis, MN) plus 100 μg/ml heparin (FGF-1/H) or
TGF-β1 (5 ng/ml). Control cells were incubated in SFM only.
FGF-1, heparin, and TGF-β1 concentration was based in previous
studies [6,7]. Heparin was used because it plays an essential
role in FGF signaling as it has a direct association with it and its
receptor [11-13]. FGF and heparin were used in combination,
because it has been confirmed that when incubated alone, they
have a negligible effect [6,7].
FGF-1/H-activated signaling pathway
pharmacological inhibition
HLF were kept for 24 h in serum-free media. On the next day, they
were pre-incubated for 30 min with selective pharmacological
inhibitors of signaling pathways (see below), followed by the
addition of FGF-1/H; incubating the cells finally for a period of
up to 24 h, depending on the experiment: for MMP-1 and type I
collagen proteins the last period was 24 h, for MMP-1 and α1(I)
pro-collagen mRNA expression analysis for 6h, for evaluation of
ERK1, p38, AKT1, JNK1 up to 8h, and finally to ETS-1 expression
for 30 min.
The analysis of α-SMA was performed as follows: cells were
stimulated for 24 h in serum-free medium (SFM), followed by
incubation with TGF-β1 (5 ng/ml) during 24 h to stimulate protein
expression. On the next day, cells were pre-incubated for 30 min
with the respective pharmacological inhibitor, and finally FGF-
1/H was added to the same medium and incubated during 24
h (without eliminating the inhibitors). In parallel experiments,
HLF were incubated in the presence of the corresponding
pharmacological inhibitor in the absence of FGF-1/H or TGF-β1
for 24 h (negative controls).
The selective pharmacological inhibitors of specific signaling
pathways were: PD098059 (40μM; Calbiochem, San Diego, CA,
USA), an inhibitor of ERK1/2/3 of the MEK-ERK MAPK signaling
pathway; SB203580 (20μM), a p38-MAPK signaling pathway
inhibitor Calbiochem, San Diego, CA); SB600125 (50μM;
Cell Signaling Technology, Beverly, MA) the JNK1/2/3 MAPK
pathway inhibitor; LY294002 (50μM; Cell Signaling Technology,
Beverly, MA), a phosphatidylinositol 3-kinase (PI3K) inhibitor;
and SB431542 (10μM; Calbiochem, San Diego, CA), an inhibitor
of TBRI kinase activity and consequently, an indirect inhibitor
of Smad2/3 phosphorylation (an integrant of the TGF-β/Smad
signaling pathway).The dosage of the inhibitors was based on
previous studies of our study group [14].
Western blot analysis
Proteins drawn from whole-cell extracts and serum-free
conditioned media were obtained independently from
fibroblasts stimulated with 20 ng/ml FGF-1 (R&D, Minneapolis,
MN) plus 100μg/ml heparin (FGF-1/H) or TGF-β1 (5 ng/ml) 24
h. We separated 20μg of protein from whole-cell extracts or
12μg from conditioned media by electrophoresis on SDS-PAGE
gels, and these simples were then transferred to nitrocellulose
membranes and incubated with primary antibodies: anti-human
α1(I) collagen (Col 1α1 (L-19) Goat polyclonal (sc-8783; Santa
Cruz Biotechnology, INC; dilution 1:200); anti-MMP-1 (Ab-1)
Mouse Mab (41-1E5; Calbiochem; dilution 1:200); monoclonal
anti-α-smooth muscle actin (1A4; Sigma-Aldrich, St. Louis
MO; dilution 1:300); rabbit polyclonal anti-Erk1 (K-23) ab (sc-
94; Santa Cruz Biotechnology; dilution 1:500); anti-phospho-
Erk1 (12d4), Mouse mab (sc-81492; Santa Cruz Biotechnology;
dilution 1:200); anti-JNK1 (D-2), Mouse mab (sc-7345 Santa Cruz
Biotechnology; dilution 1:500); anti-phospho-JNK1 (9H8), Mouse
mab (sc-81502; Santa Cruz Biotechnology; dilution 1:500); anti-
AKT1 (H-136), Rabbit polyclonal antibody (sc-8312 Santa Cruz Biotechnology; dilution 1:500); antiphospho-AKT1 (Ser 473),
Rabbit mab (Santa Cruz Biotechnology; dilution 1:500); anti-p-38
Map Kinase, Rabbit pab (#9212; Cell Signaling; dilution 1:200);
anti phospho-p-38 MAPK (Thr180/Tyr182) (D3F9), Rabbit mAb
(#4511; Cell Signaling; dilution 1:1000); and anti-β-tubulin (Santa
Cruz Biotechnology; dilution 1:200). A Western blot quantitative
analysis was conducted with Image Lab 5.2.1 software with
results expressed in mean±SD values of relative intensity units
(RIU) as a ratio of the band density to total β-tubulin. Changes
observed in phosphorylated protein levels were measured
with reference to respective nonphosphorylated proteins. The
measure of MMP-1 in conditioned media has not a currently
control intern; therefore, the concentration of protein charged in
the gel is accurately quantitated.
RNA extraction, cDNA synthesis and RT-qPCR
Total RNA was isolated from treated or control HLF (incubated
6h), using the TRIzol reagent (Invitrogen Life Technologies, Grand
Island NY) and reverse-transcribed into cDNA using High-Capacity
cDNA reverse transcription kit (Applied Biosystems™, Foster city
USA) according to the manufacturer´s instructions. Quantitative
real-time PCR (RT-qPCR) was performed with Quant Studio
12K Flex (Applied Biosystems™) using the following specific
TaqMan probes (Applied Biosystems™). Collagen 1 COL 1A1
(Hs00164004_m1) and MMP1 (Hs00899568_m1). The cycling
conditions were 95° for 20sec, then 40 cycles at 95° for 15s and
60° for 1min. The levels of mRNA expression were assessed
after normalization using the HPRT (hypoxanthine-guanine
phosphoribosyltransferase) TaqMan probe (Hs00399225_m1) as
endogenous control. All amplifications reactions were performed
in triplicate, and the relative quantification of mRNA expression
was calculated using the comparative threshold cycle method
(2^-ΔΔCT) [15]. RT-qPCR analysis was performed for three
independent experiments. Data are presented as the mean ±
standard deviation of three independent experiments.
Collagen content measurement
Concentrations of newly synthesized collagen were measured in
the conditioned media via a quantitative Sircol Soluble Collagen
Assay (Biocolor Ltd, Carrickfergus, Northern Ireland), according to
the manufacturer's specifications [16]. Results are expressed as
the mean ± standard deviation values of μg collagen/mg protein.
Expression of the ETS-1 transcription factor
To determine whether some of the transcription factors that
regulate different genes of the metabolism of extracellular matrix
in fibroblasts is activated by FGF-1, and if heparin potentiates this
action, ETS-1 was chosen [17]. For this, cells were incubated for 30
min with FGF-1, heparin alone or the combination FGF-1/H. We
examined the expression of transcription factor ETS-1 by Western
blot; ETS-1 was purified from the nucleus after stimulating the
HLF with FGF-1/H, FGF-1, or heparin using a commercial kit (NEPER
Nuclear and Cytoplasmic Extraction Reagent Kit, Thermo
Scientific 7883) according to the manufacturer's specifications
[18]. Western blot was performed on the nuclear fraction with
an anti-ETS-1 rabbit polyclonal antibody (N276) Rabbit pab (sc 111; Santa Cruz; dilution 1:200); Anti-Lamin A + C Rabbit pab
(GTX101127; Genetex; dilution 1:500) was used as a load control
charge. A Western blot quantitative analysis was conducted using
Image Lab 5.2.1 software and results are expressed as mean ± SD
of relative intensity units (RIU) as a ratio of the band density to
nuclear lamin A/C.
Statistical analysis
Results are presented graphically based on the means ± SD of
at least three independent experiments. Statistically significant
changes between samples were assessed by one-way ANOVA
and with Tukey´s post hoc tests for multiple comparisons. The
analyses were performed using the statistical package GraphPad
version 6.01 (GraphPad Software, Inc., La Jolla, CA, USA). P<0.05
was deemed statistically significant.
Results
FGF-1/H induces the overexpression of MMP-1
by the activation of JNK, MEK, and TGF-β/Smad
signaling pathways
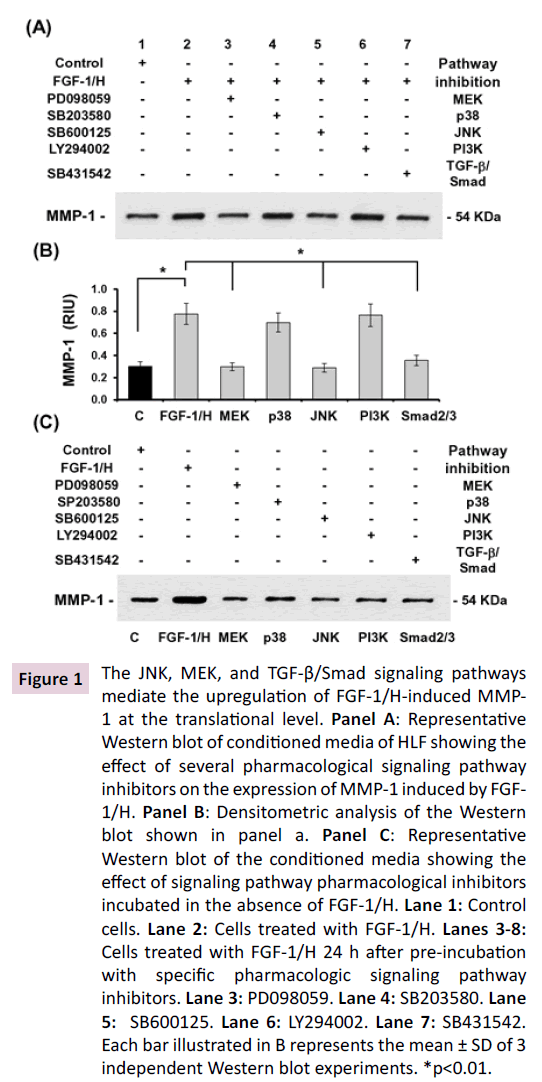
The effect of FGF-1/H on MMP-1 expression was evaluated
by Western blot and RT-qPCR. Our Western blot analysis of
MMP-1 secreted into the culture media revealed a significant
overexpression when compared to the control (Figures 1A-1B;
Lane 2 vs. 1; p<0.01).When cells were incubated with FGF-1/H in
the presence of selective inhibitors of the signaling pathways of
interest, the overexpression of MMP-1 was significantly blocked
by PD098059, SB600125, and SB431542, inhibitors of JNK, MEK,
and TGF-β/Smad signaling pathway, respectively (Figures 1A-1B;
Lanes 3, 5, and 7; p<0.01). On the other hand, inhibitors of the
p38 and PI3K pathways, LY294002 and SB203580 respectively,
did not block FGF-1/H-induced MMP-1 expression (Figures
1A-1B; Lanes 4 and 6). HLF incubated with the pharmacologic
inhibitors in the absence of FGF-1/H show that these molecules
alone did not have any effect on the expression of MMP-1 (Figure
1C; Lanes 3-7 vs. 2); showing similar levels of expression to as
those of control cells (Figure 1C; Lane 1).
Figure 1: The JNK, MEK, and TGF-β/Smad signaling pathways
mediate the upregulation of FGF-1/H-induced MMP-
1 at the translational level. Panel A: Representative
Western blot of conditioned media of HLF showing the
effect of several pharmacological signaling pathway
inhibitors on the expression of MMP-1 induced by FGF-
1/H. Panel B: Densitometric analysis of the Western
blot shown in panel a. Panel C: Representative
Western blot of the conditioned media showing the
effect of signaling pathway pharmacological inhibitors
incubated in the absence of FGF-1/H. Lane 1: Control
cells. Lane 2: Cells treated with FGF-1/H. Lanes 3-8:
Cells treated with FGF-1/H 24 h after pre-incubation
with specific pharmacologic signaling pathway
inhibitors. Lane 3: PD098059. Lane 4: SB203580. Lane
5: SB600125. Lane 6: LY294002. Lane 7: SB431542.
Each bar illustrated in B represents the mean ± SD of 3
independent Western blot experiments. *p<0.01.
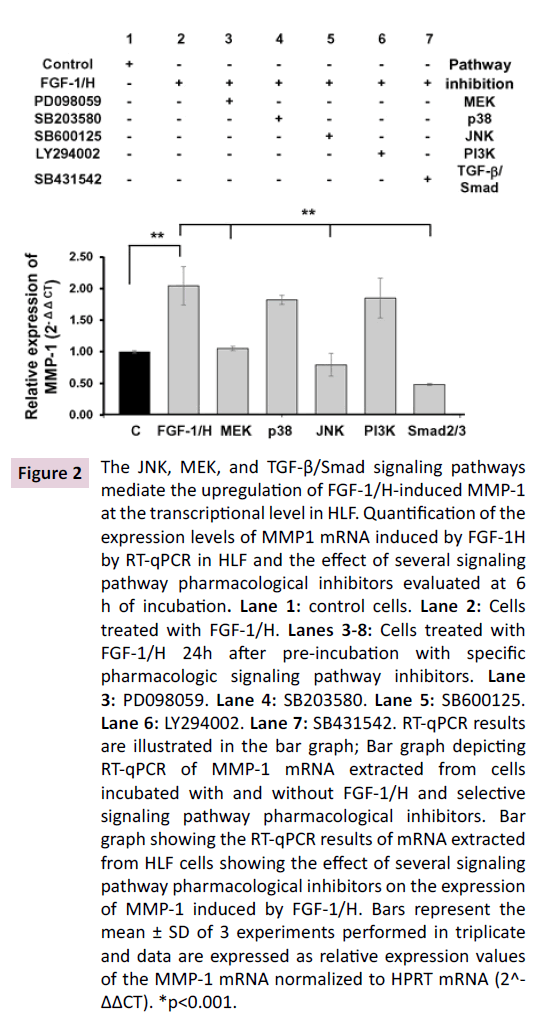
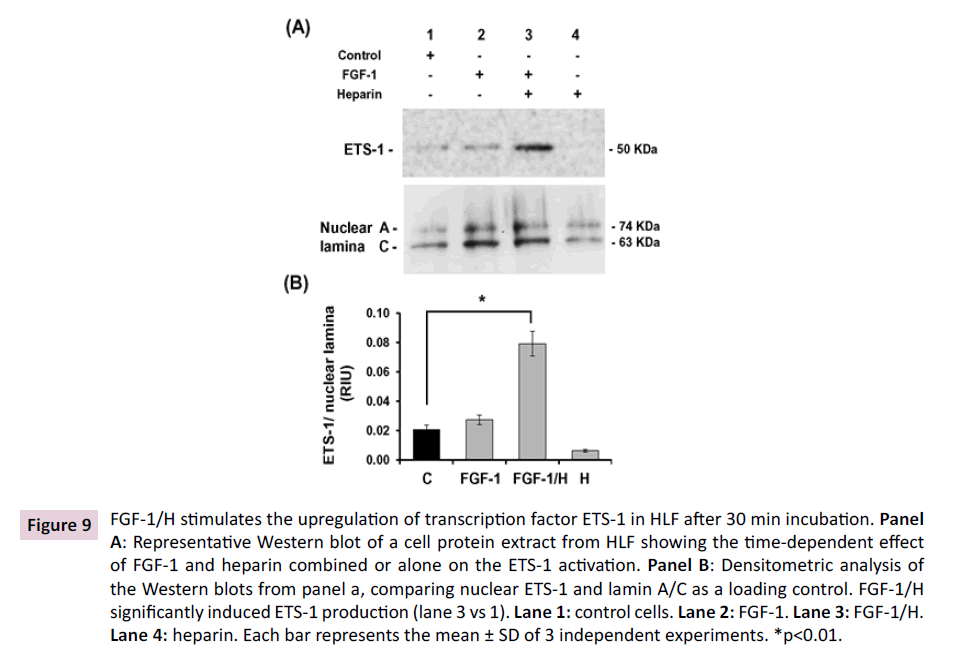
RT-qPCR experiments using mRNA extracted from the HLF (Figure
2) confirm the results of the Western blot: MEK, JNK, and TGF-β/
Smad signaling pathways inhibitors diminished the upregulation
of MMP-1 gene induced by FGF-1/H (Figure 2; Lanes 3, 5 and 7
vs. 2; p<0.001).
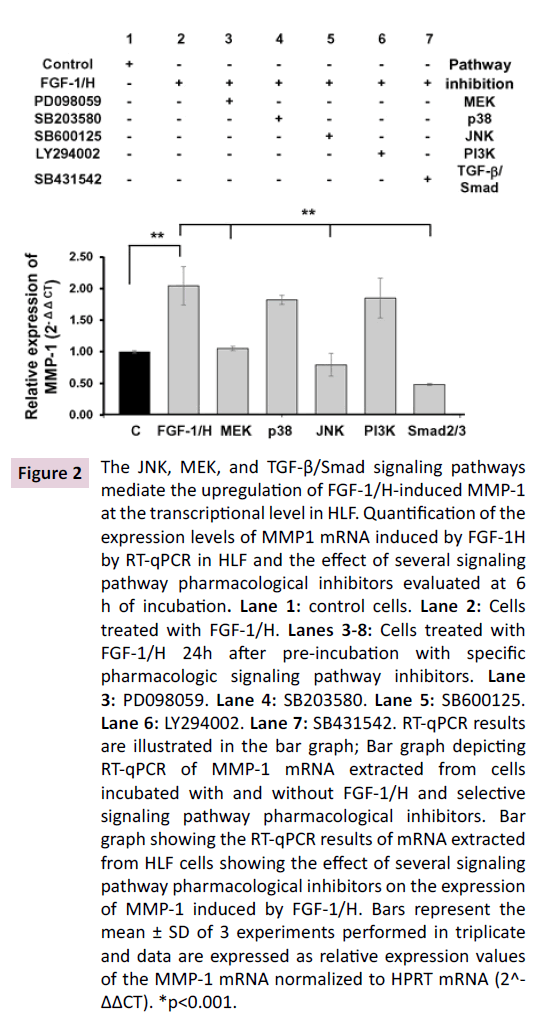
Figure 2: The JNK, MEK, and TGF-β/Smad signaling pathways
mediate the upregulation of FGF-1/H-induced MMP-1
at the transcriptional level in HLF. Quantification of the
expression levels of MMP1 mRNA induced by FGF-1H
by RT-qPCR in HLF and the effect of several signaling
pathway pharmacological inhibitors evaluated at 6
h of incubation. Lane 1: control cells. Lane 2: Cells
treated with FGF-1/H. Lanes 3-8: Cells treated with
FGF-1/H 24h after pre-incubation with specific
pharmacologic signaling pathway inhibitors. Lane
3: PD098059. Lane 4: SB203580. Lane 5: SB600125.
Lane 6: LY294002. Lane 7: SB431542. RT-qPCR results
are illustrated in the bar graph; Bar graph depicting
RT-qPCR of MMP-1 mRNA extracted from cells
incubated with and without FGF-1/H and selective
signaling pathway pharmacological inhibitors. Bar
graph showing the RT-qPCR results of mRNA extracted
from HLF cells showing the effect of several signaling
pathway pharmacological inhibitors on the expression
of MMP-1 induced by FGF-1/H. Bars represent the
mean ± SD of 3 experiments performed in triplicate
and data are expressed as relative expression values
of the MMP-1 mRNA normalized to HPRT mRNA (2^-
ΔΔCT). *p<0.001.
FGF-1/H downregulates collagen I through the
MEK, P38, and PI3K signaling pathways
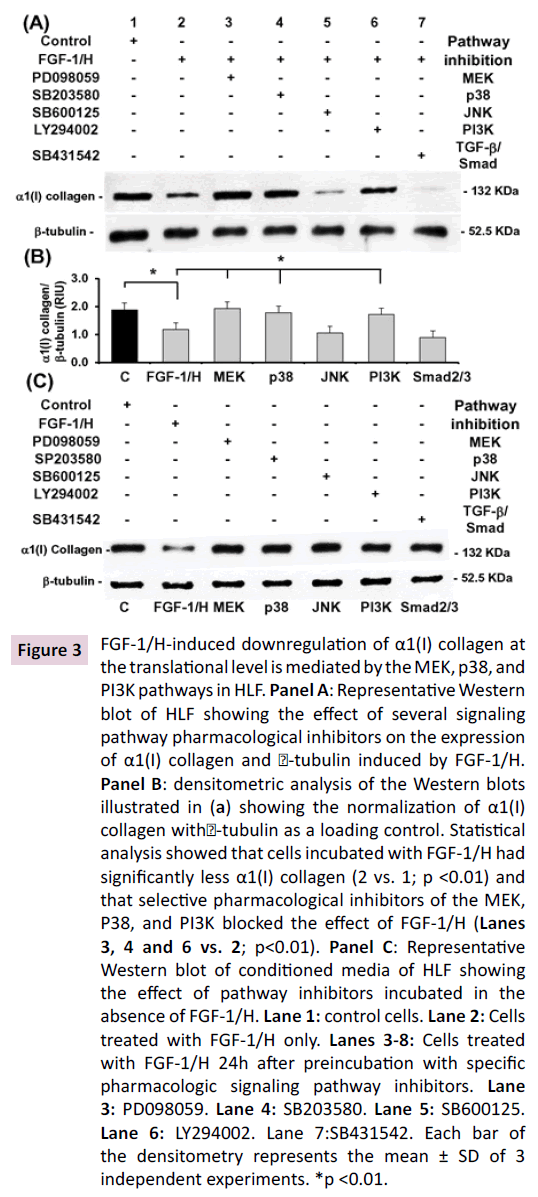
The effect of FGF-1/H on collagen I protein expression was
analyzed via Western blot, to pro-collagen α1(I) chain collagen
with RT-qPCR, and also the amount of total collagen secreted
into the culture media using the Sircol reagent was measured.
The Western blot analysis shows that HLF express high quantities
of pro α1(I) collagen (Figures 3A-3B; Lane 1), which is significantly
downregulated by FGF-1/H (Figures 3A-3B; Lane 2 vs. 1; p<0.01).
When FGF-1/H was incubated in the presence of selective pharmacologic inhibitors, the MEK, P38, and PI3K inhibitors
blocked the effect of FGF-1/H (Figures 3A-3B; Lanes 3, 4, and 6
vs. 2; p<0.01). JNK and TGF-β/Smad pathways inhibition did not
restore collagen downregulation induced by FGF-1/H (Figures
3A-3B; Lanes 5 and 7 vs. 2; NS). A control of this analysis was
performed through the incubation of HLF cells in the presence
of the pharmacologic inhibitors only and in the absence of FGF-
1/H, showing that these molecules alone did not have effect on
the expression of pro α1(I) collagen (Figures 3C; Lanes 3-7 vs. 2).
Only FGF-1/H induced the downregulation of pro α1 (I) collagen
(Figure 3C; Lane 2 vs. 1; p<0.01).
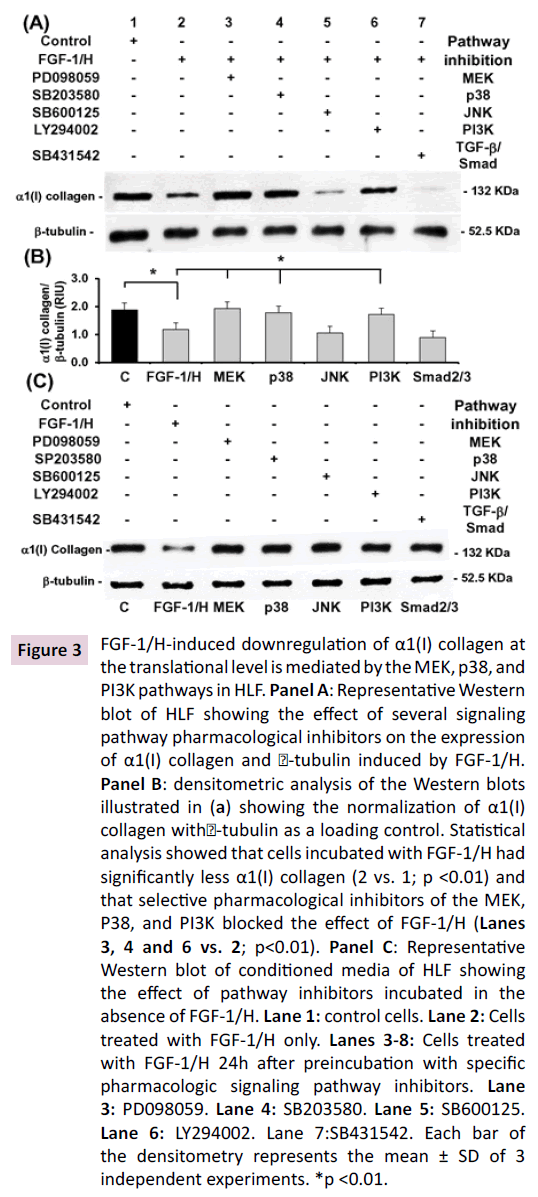
Figure 3: FGF-1/H-induced downregulation of α1(I) collagen at
the translational level is mediated by the MEK, p38, and
PI3K pathways in HLF. Panel A: Representative Western
blot of HLF showing the effect of several signaling
pathway pharmacological inhibitors on the expression
of α1(I) collagen and -tubulin induced by FGF-1/H.
Panel B: densitometric analysis of the Western blots
illustrated in (a) showing the normalization of α1(I)
collagen with-tubulin as a loading control. Statistical
analysis showed that cells incubated with FGF-1/H had
significantly less α1(I) collagen (2 vs. 1; p <0.01) and
that selective pharmacological inhibitors of the MEK,
P38, and PI3K blocked the effect of FGF-1/H (Lanes
3, 4 and 6 vs. 2; p<0.01). Panel C: Representative
Western blot of conditioned media of HLF showing
the effect of pathway inhibitors incubated in the
absence of FGF-1/H. Lane 1: control cells. Lane 2: Cells
treated with FGF-1/H only. Lanes 3-8: Cells treated
with FGF-1/H 24h after preincubation with specific
pharmacologic signaling pathway inhibitors. Lane
3: PD098059. Lane 4: SB203580. Lane 5: SB600125.
Lane 6: LY294002. Lane 7: SB431542. Each bar of
the densitometry represents the mean ± SD of 3
independent experiments. *p <0.01.
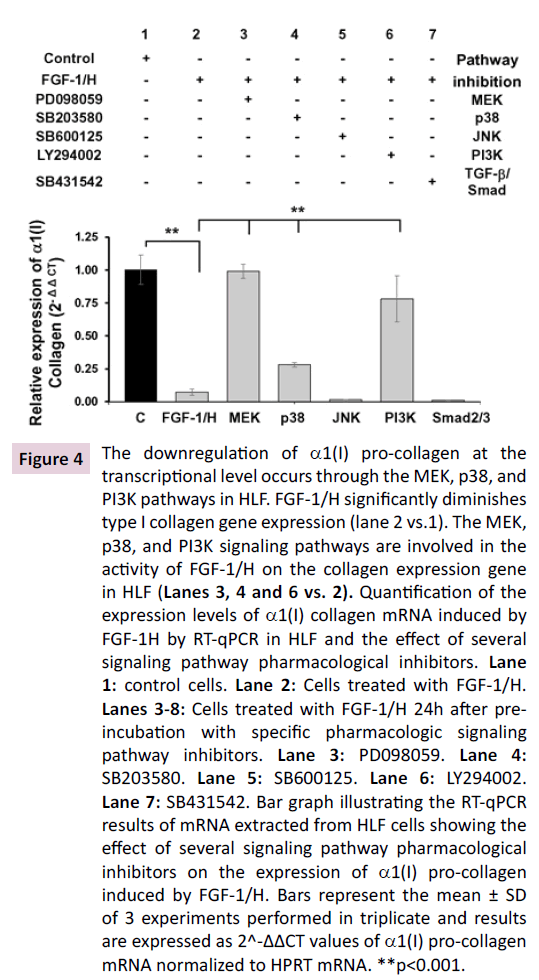
The collagen expression gene measured by RT-qPCR confirms
the results evaluated by Western-blot. The MEK, p38, and PI3K signaling pathways are involved in the activity of FGF-1/H on the
collagen expression gene in HLF (Figure 4; Lanes 3, 4, and 6 vs. 2; p<0.001).
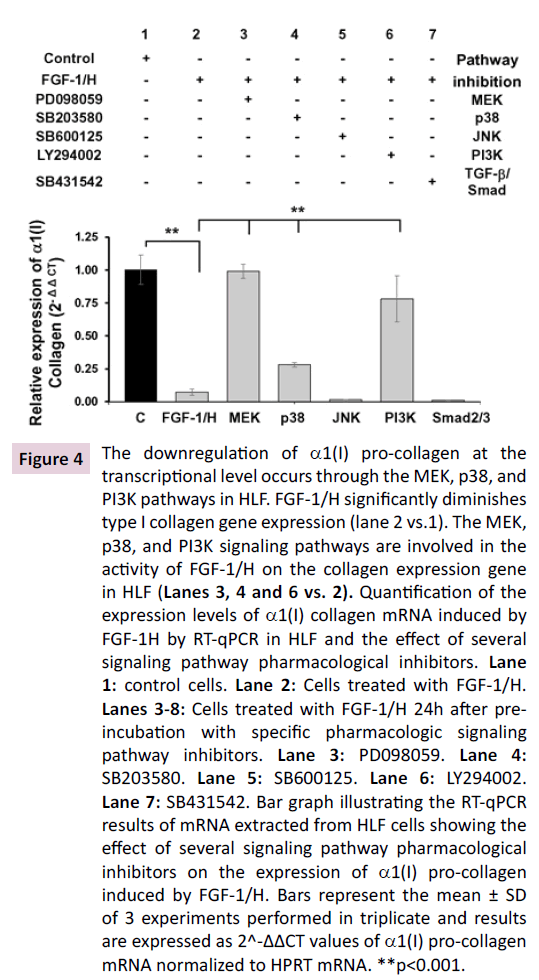
Figure 4: The downregulation of α1(I) pro-collagen at the
transcriptional level occurs through the MEK, p38, and
PI3K pathways in HLF. FGF-1/H significantly diminishes
type I collagen gene expression (lane 2 vs.1). The MEK,
p38, and PI3K signaling pathways are involved in the
activity of FGF-1/H on the collagen expression gene
in HLF (Lanes 3, 4 and 6 vs. 2). Quantification of the
expression levels of α1(I) collagen mRNA induced by
FGF-1H by RT-qPCR in HLF and the effect of several
signaling pathway pharmacological inhibitors. Lane
1: control cells. Lane 2: Cells treated with FGF-1/H.
Lanes 3-8: Cells treated with FGF-1/H 24h after preincubation
with specific pharmacologic signaling
pathway inhibitors. Lane 3: PD098059. Lane 4:
SB203580. Lane 5: SB600125. Lane 6: LY294002.
Lane 7: SB431542. Bar graph illustrating the RT-qPCR
results of mRNA extracted from HLF cells showing the
effect of several signaling pathway pharmacological
inhibitors on the expression of α1(I) pro-collagen
induced by FGF-1/H. Bars represent the mean ± SD
of 3 experiments performed in triplicate and results
are expressed as 2^-ΔΔCT values of α1(I) pro-collagen
mRNA normalized to HPRT mRNA. **p<0.001.
The inhibitors of MEK, p38, and PI3K signaling
pathways blocked the decrement of total
collagen protein secretion induced by FGF-1/H
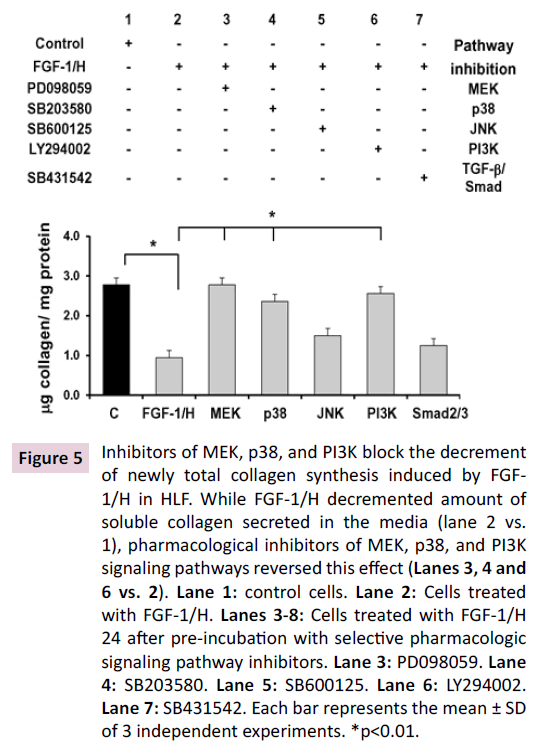
Newly total collagen synthesized and secreted into the culture
medium by HLF was measured by Sircol reagent, confirming
the Western blot results. Thus, while FGF-1/H decremented
collagen protein secreted into culture media (Figure 5; Lane 2
vs. 1; p<0.01), pharmacological inhibitors of MEK, p38, and PI3K
signaling pathways reversed this effect (Figure 5; Lanes 3, 4, and
6 vs. 2; p<0.01).
Figure 5: Inhibitors of MEK, p38, and PI3K block the decrement
of newly total collagen synthesis induced by FGF-
1/H in HLF. While FGF-1/H decremented amount of
soluble collagen secreted in the media (lane 2 vs.
1), pharmacological inhibitors of MEK, p38, and PI3K
signaling pathways reversed this effect (Lanes 3, 4 and
6 vs. 2). Lane 1: control cells. Lane 2: Cells treated
with FGF-1/H. Lanes 3-8: Cells treated with FGF-1/H
24 after pre-incubation with selective pharmacologic
signaling pathway inhibitors. Lane 3: PD098059. Lane
4: SB203580. Lane 5: SB600125. Lane 6: LY294002.
Lane 7: SB431542. Each bar represents the mean ± SD
of 3 independent experiments. *p<0.01.
At the translational level, FGF-1/H induces
downregulation of TGF-β1-induced α-SMA
expression through the JNK, MEK, and TGF-β/
Smad signaling pathways
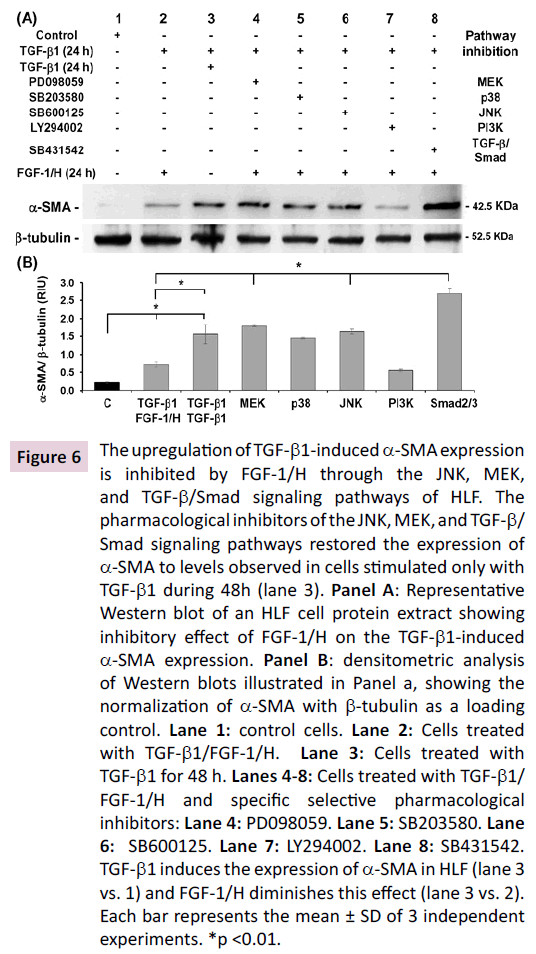
HLF extracted from human lung are composed of about 14.8 ±
11.6 % of myofibroblasts that constitutively express α-SMA [4].
To confirm that TGF-β1 induces the expression of α-SMA, cells
were incubated with TGF-β1 for 48 h (Figures 6A-6B; Lane 3 vs.1; p<0.01). Furthermore, the α-SMA upregulation induced
by TGF-β1 was significantly diminished by FGF-1/H (Figures
6A-6B; Lane 3 vs. 2; p<0.01). For the other samples, cells were
incubated first with TGF-β1 for 24 h followed by incubation with
selective pharmacologic inhibitors of the signaling pathways of
interest for 30 min, and they were finally stimulated with FGF-
1/H for 24 h. We were thus able to evaluate which signaling
pathway is activated by FGF-1/H to inhibit TGF-β1-mediated
α-SMA expression (Figures 6A-6B; Lane 4, 6 and 8 vs. 2; p<0.01).
The pharmacological inhibitors of the JNK, MEK, and TGF-β/
Smad signaling pathways restored the expression of α-SMA to
levels observed in cells stimulated only with TGF-β1 during 48 h
(Figures 6A-6B; Lane 3). Thus, FGF-1/H inhibits effects of TGF-β1-
mediated α-SMA expression through these pathways. The p38
and PI3K inhibitors did not affect the diminution induced by FGF-
1/H on the TGF-β1-induced α-SMA expression (Figures 6A-6B;
Lanes 5 and 7).
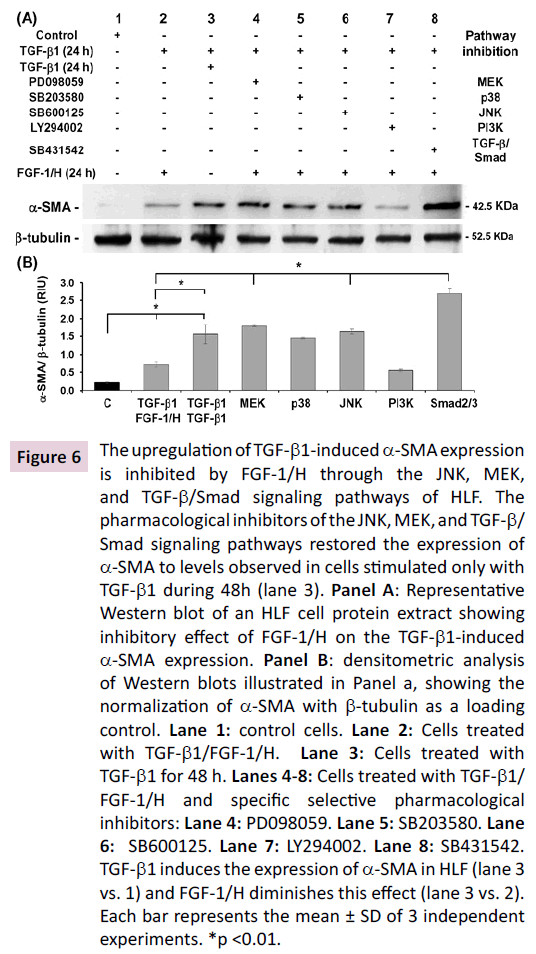
Figure 6: The upregulation of TGF-β1-induced α-SMA expression
is inhibited by FGF-1/H through the JNK, MEK,
and TGF-β/Smad signaling pathways of HLF. The
pharmacological inhibitors of the JNK, MEK, and TGF-β/
Smad signaling pathways restored the expression of
α-SMA to levels observed in cells stimulated only with
TGF-β1 during 48h (lane 3). Panel A: Representative
Western blot of an HLF cell protein extract showing
inhibitory effect of FGF-1/H on the TGF-β1-induced
α-SMA expression. Panel B: densitometric analysis
of Western blots illustrated in Panel a, showing the
normalization of α-SMA with β-tubulin as a loading
control. Lane 1: control cells. Lane 2: Cells treated
with TGF-β1/FGF-1/H. Lane 3: Cells treated with
TGF-β1 for 48 h. Lanes 4-8: Cells treated with TGF-β1/
FGF-1/H and specific selective pharmacological
inhibitors: Lane 4: PD098059. Lane 5: SB203580. Lane
6: SB600125. Lane 7: LY294002. Lane 8: SB431542.
TGF-β1 induces the expression of α-SMA in HLF (lane 3
vs. 1) and FGF-1/H diminishes this effect (lane 3 vs. 2).
Each bar represents the mean ± SD of 3 independent
experiments. *p <0.01.
FGF-1/H stimulates the activation of AKT1, ERK1,
JNK1, and p38 Proteins
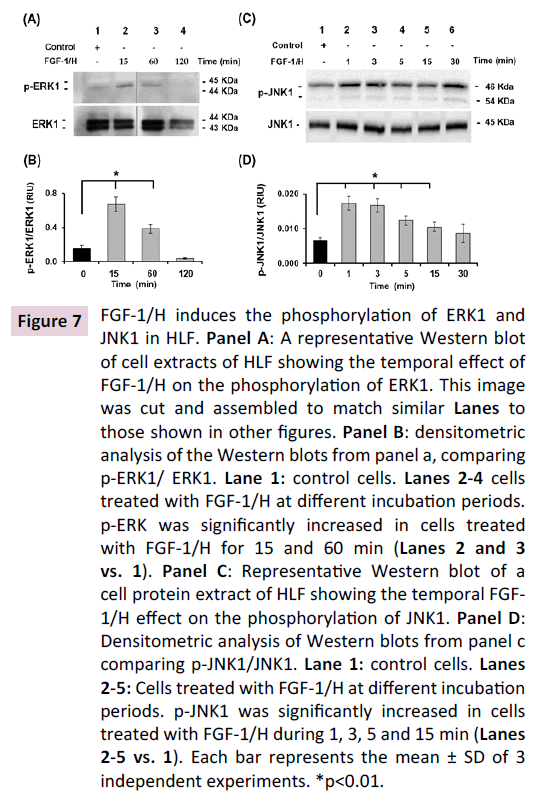
To confirm that the downregulation in α-SMA expression
induced by FGF-1/H observed in our experiments corresponded
with the activation of the above-mentioned signaling pathways,
kinetics of the phosphorylation of specific proteins in pathways
were determined. Thus, by Western blot, the FGF-1/H-induced
phosphorylation of ERK1, JNK1, AKT1, and p38 was assayed.
Accordingly, ERK1, which forms part of the MEK MAPK signaling
pathway, was phosphorylated (p-ERK1) by the exposure of HLF
to FGF-1/H for 15-60 min (Figures 7A-7B; Lanes 2 and 3 vs. 1;
p<0.01). JNK1, which forms part of the JNK signaling pathway,
showed an increase in phosphorylation (p-JNK1) after 1-30 min
exposure to FGF-1/H (Figures 7C-D; Lanes 2-6 vs. 1; p<0.01).
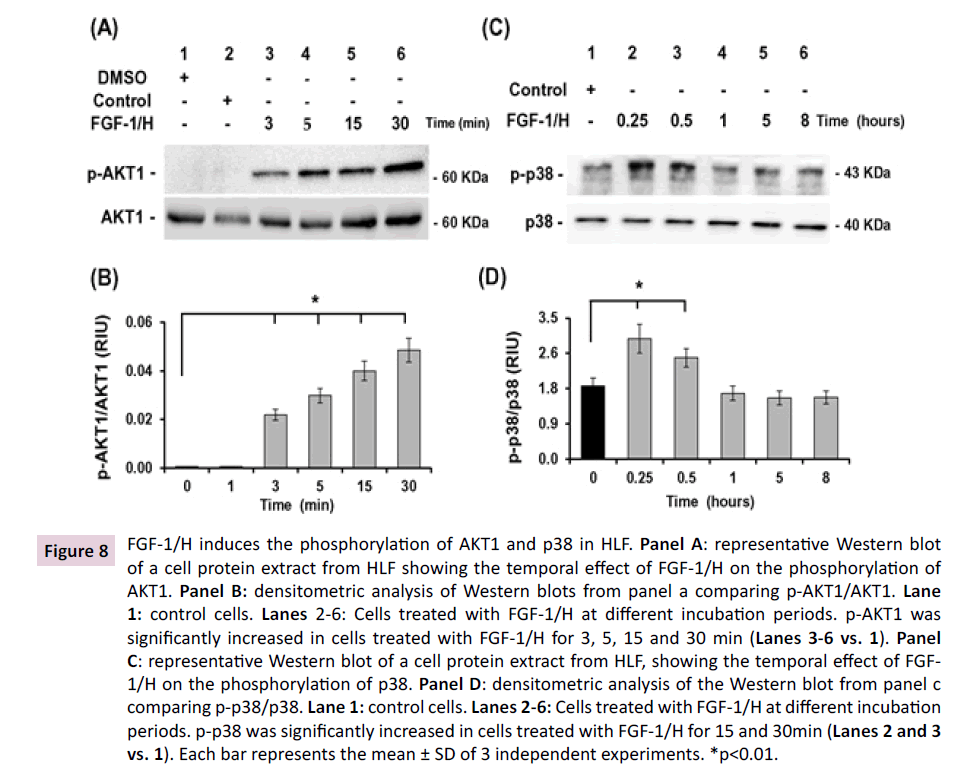
AKT1, a protein that forms part of the PI3K signaling pathway,
showed an increase in phosphorylation (p-AKT1) after 3-30 min
exposure to FGF-1/H (Figures 8A-8B; Lanes 3-6 vs. 2; p<0.01),
while p38 exhibited significant phosphorylation (p-p38) after 15
and 30 min exposure (Figures 8C-8D; Lanes 2 and 3 vs. 1; p<0.01).
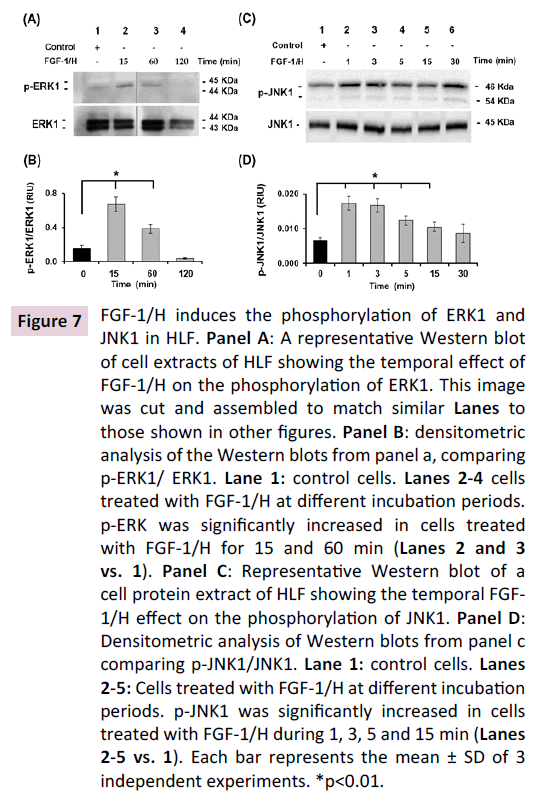
Figure 7: FGF-1/H induces the phosphorylation of ERK1 and
JNK1 in HLF. Panel A: A representative Western blot
of cell extracts of HLF showing the temporal effect of
FGF-1/H on the phosphorylation of ERK1. This image
was cut and assembled to match similar Lanes to
those shown in other figures. Panel B: densitometric
analysis of the Western blots from panel a, comparing
p-ERK1/ ERK1. Lane 1: control cells. Lanes 2-4 cells
treated with FGF-1/H at different incubation periods.
p-ERK was significantly increased in cells treated
with FGF-1/H for 15 and 60 min (Lanes 2 and 3
vs. 1). Panel C: Representative Western blot of a
cell protein extract of HLF showing the temporal FGF-
1/H effect on the phosphorylation of JNK1. Panel D:
Densitometric analysis of Western blots from panel c
comparing p-JNK1/JNK1. Lane 1: control cells. Lanes
2-5: Cells treated with FGF-1/H at different incubation
periods. p-JNK1 was significantly increased in cells
treated with FGF-1/H during 1, 3, 5 and 15 min (Lanes
2-5 vs. 1). Each bar represents the mean ± SD of 3
independent experiments. *p<0.01.
Figure 8: FGF-1/H induces the phosphorylation of AKT1 and p38 in HLF. Panel A: representative Western blot
of a cell protein extract from HLF showing the temporal effect of FGF-1/H on the phosphorylation of
AKT1. Panel B: densitometric analysis of Western blots from panel a comparing p-AKT1/AKT1. Lane
1: control cells. Lanes 2-6: Cells treated with FGF-1/H at different incubation periods. p-AKT1 was
significantly increased in cells treated with FGF-1/H for 3, 5, 15 and 30 min (Lanes 3-6 vs. 1). Panel
C: representative Western blot of a cell protein extract from HLF, showing the temporal effect of FGF-
1/H on the phosphorylation of p38. Panel D: densitometric analysis of the Western blot from panel c
comparing p-p38/p38. Lane 1: control cells. Lanes 2-6: Cells treated with FGF-1/H at different incubation
periods. p-p38 was significantly increased in cells treated with FGF-1/H for 15 and 30min (Lanes 2 and 3
vs. 1). Each bar represents the mean ± SD of 3 independent experiments. *p<0.01.
FGF-1/H stimulates the upregulation of
transcription factor ETS-1
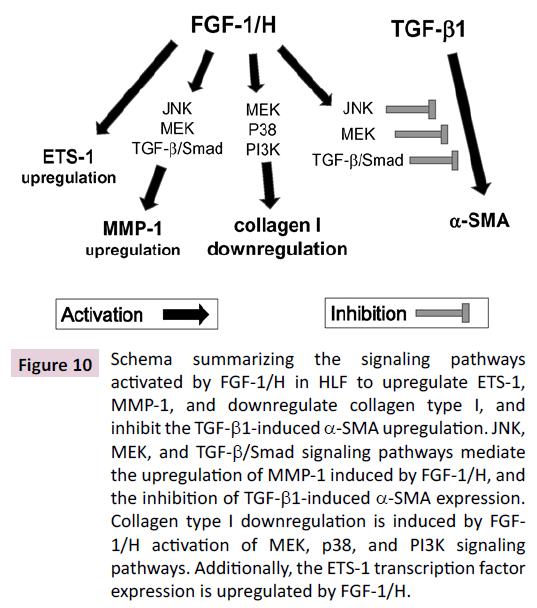
With the aim of evaluate one of the transcription factors
involving in the regulation of genes of the metabolism of the ECM
in fibroblasts, that might be activated by FGF-1/H in HLF, ETS-1 was chosen [17,19]; we examined the expression of transcription
factor ETS-1 by Western blot using nuclear extracts. We found
that FGF-1/H upregulates the expression of this factor after 30
min of stimulation relative to the control (Figures 9; Lane 3 vs. 1;
p<0.01) while FGF-1 and heparin alone have an incipient effect
(Figures 9; Lanes 2 and 4; NS), showing that ETS-1 is efficiently
upregulated by FGF-1/H. Results about the different signaling
pathways activated by FGF-1/H are summarized in Figure 10.
Figure 9: FGF-1/H stimulates the upregulation of transcription factor ETS-1 in HLF after 30 min incubation. Panel
A: Representative Western blot of a cell protein extract from HLF showing the time-dependent effect
of FGF-1 and heparin combined or alone on the ETS-1 activation. Panel B: Densitometric analysis of
the Western blots from panel a, comparing nuclear ETS-1 and lamin A/C as a loading control. FGF-1/H
significantly induced ETS-1 production (lane 3 vs 1). Lane 1: control cells. Lane 2: FGF-1. Lane 3: FGF-1/H.
Lane 4: heparin. Each bar represents the mean ± SD of 3 independent experiments. *p<0.01.
Figure 10: Schema summarizing the signaling pathways
activated by FGF-1/H in HLF to upregulate ETS-1,
MMP-1, and downregulate collagen type I, and
inhibit the TGF-β1-induced α-SMA upregulation. JNK,
MEK, and TGF-β/Smad signaling pathways mediate
the upregulation of MMP-1 induced by FGF-1/H, and
the inhibition of TGF-β1-induced α-SMA expression.
Collagen type I downregulation is induced by FGF-
1/H activation of MEK, p38, and PI3K signaling
pathways. Additionally, the ETS-1 transcription factor
expression is upregulated by FGF-1/H.
Discussion
FGF-1/H has been studied in our lab, and it exhibits potent antifibrosing
characteristics, antagonizing several effects mediated
by TGF-β1 [6-8], through mechanisms involving signaling
pathways that have not been widely studied. Therefore, for this
study we analyzed signaling pathways stimulated by FGF-1/H
to downregulate type I collagen and α-SMA, and to upregulate
MMP-1 in HLF. Heparin is a polyanionic, linear, and highly sulfated glycosaminoglycan that retards the degradation of FGF-
1 and that favors stabilization with the FGFR1 and subsequent
signaling cascades [11-13], integrated into a complex network of
signaling pathways activated by FGF-1, such as JNK, MEK, p38,
and MEK [9,13]. FGF-1 and heparin were not used alone in the
experiments because they have an incipient effect only, as we
have demonstrated previously [5,6], showing an effect on ETS-1
expression similar to the one observed in this work. The results
are summarized in Figure 10.
The activation of the JNK, MEK, and TGF-β/Smad signaling
pathways by FGF-1/H in HLF to downregulate MMP-1, observed
in Western blot and confirmed by RT-qPCR examination, has not
been demonstrated previously. However, these features have
been documented in other fibroblast types. For instance, the
activation of the JNK and MEK pathways has been documented
in fibroblasts derived from explant cultures of normal skin and
hypertrophic scars, where FGF-2 induces the expression of MMP-
1 in both types of cells [20]. The MEK pathway activation was also
demonstrated in four invasive melanoma cells lines constitutively
overexpressing MMP-1 via Ras/Raf/MEK/ERK, which, when
blocked, allows cells to proliferate, prevent collagenolysis, and
diminish their survival and metastatic potential [21]. The TGF-β/
Smad signaling pathway participation in the overexpression of MMP-1, has only been confirmed by FGF-2, that inhibits this
effect as part of an anti-scar mechanism in wound repair [22]; a
feature like the one observed in HLF with FGF-1/H.
We found that MEK, p38, and PI3K signaling pathways are
activated by FGF-1/H in HLF to decrease the type I collagen
synthesis, which was observed in Western blot and corroborated
in the RT-qPCR exploration. This effect has also not been seen
before in HLF. However, another member of the FGF family, FGF-2,
inhibits collagen I expression in human dental pulp cells, invasive
melanoma cells lines, and mouse osteoblastic cells (MC3T3-E1)
through MEK signaling pathway activation [20,23,24]. Regarding
the activation of the p38 and PI3K pathways by FGF-1/H and
diminishing type I collagen synthesis, there are no previous
reports on this issue and we show for the first time that this
biological role of FGF-1/H might be related to the antifibrogenic
role of this factor.
To determine which pathway is inhibited by FGF-1/H to lower
the expression of α-SMA, as spontaneous inhibition in basal cells
was inconclusive (data not shown), and to confirm that α-SMA is
expressed, we performed an assay stimulating α-SMA-expression
with TGF-β1 addition. Afterwards, these cells were incubated
with selective pharmacological signaling pathway inhibitors
and FGF-1/H. Our results demonstrated that the JNK, MEK, and
TGF-β, Smad signaling pathways mediate the FGF-1/H-induced
inhibition of TGF-β1-induced α-SMA expression, because their
inhibition restored the α-SMA expression to the levels of cells
incubated with TGF-β1 only.
The direct activation of the MEK pathway by FGF-1/H to inhibit
the TGF-β1-induced α-SMA expression has been observed with
the soluble ectodomain of fibroblast growth factor receptor-IIIc (sFGFR2c), which binds to fibroblast growth factor (FGF)
ligands to block the activation of the FGF-signaling pathway,
dramatically diminishing lung fibrosis in vitro and in vivo through
the upregulation of α-SMA induced by TGF-β1 in fibroblasts by
means of the activation of the MEK/ERK pathway [25].
We previously showed that FGF-1/H blocks TGF-β1-
induced α-SMA expression and that this is accompanied by the
inhibition of Smad2 phosphorylation in HLF (7), and also, through
experiments conducted in vivo via the prolonged transient
overexpression of FGF-1 (AdFGF-1) in HLF, it was found that α-SMA
is inhibited through the reduction of Smad2 phosphorylation,
and also that AdFGF-1 attenuates an increase in TBRI protein
and mRNA levels in HLF and alveolar epithelial cells in vitro [8].
Additionally, in the TGF-β/Smad pathway, an inhibitory effect of
FGF-1/H on α-SMA down regulation has been reported with the
FGF-2 inhibition of TGF-β1-induced α-SMA in airway smooth muscle
cells in vitro through the inhibition of TBRI [26].
The inhibitory effects of FGF-1/H on α-SMA (downregulation)
through the JNK pathway has not been reported in HLF, which
suggests that the activation of these signaling pathways by
TGF-β1-induced α-SMA must be analyzed further using an
experimental approach.
The direct activation of the TGF-β1/Smad pathway by FGF-
1/H in HLF has not been demonstrated. However, some cross
talk between signaling pathways has been described in the
TGF-β induction of FGF-2 expression in stromal cells that needs
integrated Smad3 and MAPK pathways signaling cascades to
operate an antifibrogenic mechanism in a prostate fibroblast cell
line [27]. Probably, this might occur in our HLF also, although it
must be studied further to be better understood.
Experiments on kinetic activation through the phosphorylation
of ERK1, JNK1, AKT1, and p38 proteins confirm that FGF-1/H
effectively activates corresponding pathways in HLF. It is important
to notice that some of these molecules may be activated by
canonical or crosstalk mechanisms occurring between signaling
pathways [28,29]. However, poorly understood features
regarding crosstalk dependent on signaling pathways that can
activate or inhibit some other pathways and their specific target
genes, some of which have been documented in the family of
fibroblast growth factors (FGFs) relative to receptors (FGFR), but
also in relation to growth factors like TGF-β1 and Wnt [30-32],
must be considered.
On the other hand, looking for one of the major transcription
factors involved in the regulation of genes of the ECM metabolism,
ETS-1 was chosen [17]. It was upregulated by FGF-1/H, and their
expression was significantly higher than that observed for FGF-
1 or heparin alone, confirming the synergy between FGF-1 and
heparin on the physiological effects stimulated by FGF-1. This
phenomenon has been well documented [6,7,11-13]. ETS-1 was
upregulated efficiently by FGF-1/H; this is consistent with the fact
that this transcription factor may be activated by several members
of the FGF family to regulate genes involved in ECM metabolism
as proteinases wall as proteins [17], playing a critical role in cell migration and tumor invasion; importantly, ETS-1 mediates the
upregulation of MMP-1 expression in cultured endothelial cells
[19]. Additionally, ETS-1 stimulates angiogenesis in chorioallantoic
membrane in an in vivo model in chick through a system involving
the regulation of the PI3K/AKT/MMP-1 pathway, suggesting that
Ets-1 activation is a requisite for FGF-1-mediated angiogenesis in
vivo; thus Ets-1 might be a potential target for the generation of
inhibitor drugs for the treatment of FGF-dependent pathological
angiogenesis such as metastatic tumors, rheumatoid arthritis
and diabetic retinopathy [33,34], but also to fibrosing diseases,
were it down regulates several genes, including collagen type 1
and other ECM molecules in stromal fibroblasts [17]; however,
its FGF-1/H-induced upregulation in HLF requires further studies.
That FGF-1/H signaling pathways can be used as a therapeutic
means to target fibrosis diseases was demonstrated by Shimbori
et al. who analyzed anti-fibrogenic effects of FGF-1 on pulmonary
fibrosis in vitro and in vivo through the prolonged transient
overexpression of FGF-1 from adenoviral vectors (AdFGF-1) and
TGF-β1 AdTGF-β1. Their results showed also that FGF-1 induces
decrements in α-SMA accompanied with TBR1 downregulation,
increments collagen degradation and MMP-1 expression in
TGF-β1-treated cells and alveolar epithelial cells as part of the
inhibition of TGF-β1 activation of the signaling pathway Smad2/3,
and FGFR1 upregulation induced by FGF-1. Furthermore, these
authors were able to establish an in vivo model of pulmonary
fibrosis that was reduced by FGF-1. Moreover, it has been
recognized that FGF-1 levels are increased in the serum of IPF
patients relative to control subjects´ serum [8]. FGF-1 was
also incremented in lungs of a rat lung fibrosis model induced
by paraquat plus hyperoxia, and in human lung tissue with IPF
FGF-1 colocalized with the receptor FGFR1; interestingly, FGF-
1 concentration was especially higher in tissue areas with no
inflammation or damage associated with fibrogenic lesions
[35]. These facts may reflect FGF-1-related systemic protective
antifibrogenic responses in IPF patients, though this assumption
requires further examination.
At this point, it is pertinent to mention that HLF cells were used
instead of fibroblasts derived from human lungs with IPF because
they constitute a reliable surrogate model for the study of this
ailment. In this regard, we have shown that lung fibroblasts
with IPF contain 62.8 ± 25.2 (n=5) α-SMA positive cells, while
those derived from HLF 14.8 ± 11.6 (n=5) [4]. We consider that
both fibroblasts and myofibroblasts contained in these HLF
cells responded to the stimulation of FGF-1, as can be seen in
the various experiments shown. However, the effect seems
to be most noticeable when cells were previously stimulated
with recombinant TGF-β1 in vitro, or with the viral transfection
vector AdTGF-β1, followed by AdFGF-1 in vivo [8]. In this regard,
the assessment the expression of α-SMA in vivo seems to show
better the fact that both cell populations actually responded to
the stimulation by FGF-1 when pulmonary fibrosis was induced
with bleomycin in female Sprague-Dawley rats by AdTGF-β1, and
reversed with AdFGF-1. This evidence confirms that both cell
populations respond in vitro and in vivo, further corroborating
the antagonism between FGF-1 and TGF-β1.
Regarding the use of other anti-fibrotic agents against IPF, another
member of the FGF family, FGF-2 must be mentioned. This factor
has shown a therapeutic potential very similar to that evidenced
for FGF-1 in HLF, as well as in bleomycin-induced pulmonary
fibrosis in mice [26,36,37]. Both factors have been reported to be
increased in lungs of patients with IPF in comparison to those of
normal subjects [8,38].
The therapeutic potential of FGF-1 in IPF seems promising,
given the fact that the drugs currently used are nintedanib and
pirfenidone, that do not stop fibrogenic progress or reverse the
disease, but improve decreased lung function (FEV1) and patient
survival [39,40]. Further investigation to define the precise
therapy for IPF through FGF-1 alone or in combination with
other drugs that could show satisfactory therapeutic efficacy is
evidently needed.
In relation to other molecules with antifibrotic potential, two
inorganic salts were used at very low doses both in vitro in HLF
cells, and in vivo through a bleomycin model in mice. Arsenic
trioxide (ATO) and sodium arsenite (SA) showed effects similar
to those of FGF-1 and some of FGF-2; they inhibit the TGF-β1-
induced expression of α-SMA, of collagen type I protein and
mRNA, as well as the phosphorylation of ERK and Smad2/3
[41,42]. Seemingly, these salts possess interesting therapeutic
potential that could include a combination of FGF1 and/or FGF-2,
together with ATO and/or SA.
Our analysis shows that the results obtained are consistent with
our hypothesis, thus offering new insights on signaling pathways
inactivated by FGF-1/H to upregulate MMP-1, to downregulate
type I collagen and to inhibit TGF-1-induced α-SMA expression in
HLF. Characterization of the intracellular signaling pathways that
participate in FGF-1-induced decrement in fibrosis may certainly
prove useful for novel therapeutic targeting of fibrosing diseases
such as IPF.
Conclusion
This paper describes that FGF-1/H upregulates MMP-1 principally
through the JNK, MEK, and TGF-β/Smad signaling pathways and
downregulates type I collagen chiefly through expression by JNK,
MEK, and TGF-β/Smad pathways. In addition, FGF-1/H induces
downregulation in TGF-β1-induced α-SMA expression chiefly
through the JNK, MEK, and TGF-β/Smad signaling pathways,
phosphorylating ERK1, AKT1, JNK1, and p-38, and upregulating
transcription factor ETS-1 in fibroblasts derived from human lung.
References
- Kendal RT, Feghali-Bostwick CA (2014) Fibroblasts in fibrosis: Novel roles and mediators. Front Pharmacol 5: 123.
- Selman M, King TE, Pardo A (2001) Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy. Ann Intern Med 134: 136-151.
- Selman M, Pardo A (2006) Role of epithelial cells in idiopathic pulmonary fibrosis. From innocent targets to serial killers. Proc Am Thorac Soc 3: 364-372.
- Ramos C, Montaño M, García-Alvarez J, Ruiz V, Uhal BD, et al. (2001) Fibroblasts from idiopathic pulmonary fibrosis and normal lungs differ in growth rate, apoptosis, and tissue inhibitor of metalloproteinases expression. Am J Respir Cell Mol Biol 24: 591-598.
- Habiel DM, Hogaboam C (2014) Heterogeneity in fibroblast proliferation and survival in idiopathic pulmonary fibrosis. Front Pharmacol 5: 2.
- Becerril C, Pardo A, Montano M, Ramos C, Ramirez R, et al. (1999) Acidic fibroblast growth factor induces an antifibrogenic phenotype in human lung fibroblasts. Am J Respir Cell Mol Biol 20: 1020-1027.
- Ramos C, Montaño M, Becerril C, Cisneros-Lira J, Barrera L, et al. (2006) Acidic fibroblast growth factor decreases alpha smooth muscle actin expression and induces apoptosis in human normal lung fibroblasts. Am J Physiol Lung Cell Mol Physiol 291: L871-L879.
- Shimbori C, Bellaye PS, Xia J, Gauldie J, Ask K, et al. (2016) Fibroblast growth factor‐1 attenuates TGF‐β1‐induced lung fibrosis. J Pathol 240: 197-210.
- Ornitz DM, Itoh N (2015) The fibroblast growth factor signaling pathway. Wiley Interdisciplinary Reviews: Developmental Biology 4: 215-66.
- Somogyi V, Chaudhuri N, Torrisi SE, Kahn N, Müller V, et al. (2019) The therapy of idiopathic pulmonary fibrosis: what is next?. European Respiratory Review 28: 153.
- Robinson CJ, Harmer NJ, Goodger SJ, Blundell TL, Gallagher JT (2005) Cooperative dimerization of fibroblast growth factor 1 (FGF1) upon a single heparin saccharide may drive the formation of 2:2:1 FGF1. FGFR2c heparin ternary complexes. J Biol Chem 280: 42274-42282.
- Zakrzewska M, Wiedlocha A, Szlachcic A, Krowarsch D, Otlewski J, et al. (2009) Increased protein stability of FGF1 can compensate for its reduced affinity for heparin. J Biol Chem 284: 25388-25403
- Raju R, Palapetta SM, Sandhya VK, Sahu A, Alipoor A, et al. (2014) A network map of FGF-1/FGFR signaling system. J Signal Transduct 2014.
- Ramos C, Becerril C, Montaño M, García-De-Alba C, Ramírez R, et al. (2010). FGF-1 reverts epithelial-mesenchymal transition induced by TGF-β1 through MAPK/ERK kinase pathway. Am J Physiol Lung Cell Mol Physiol 299: L222-L231.
- Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C T method. Natureprotocols 3: 1101.
- Vang A, Clements RT, Chichger H, Kue N, Allawzi A, et al. (2017) Effect of nicotinic acetylcholine receptor activation on cardiac fibroblasts: A mechanism underlying RV fibrosis associated with cigarette smoke exposure. Am J Physiol Lung Cell Mol Physiol 312: L748-L759.
- Hahne JC, Okuducu AF, Fuchs T, Florin A, Wernert N (2011) Identification of ETS-1 target genes in human fibroblasts. Int J Oncol 38: 1645-1652.
- Tsai NP, Lin YL, Tsui YC, Wei LN (2010) Dual action of epidermal growth factor: Extracellular signal-stimulated nuclear–cytoplasmic export and coordinated translation of selected messenger RNA. J Cell Biol 188: 325-333.
- Naito S, Shimizu S, Matsuu M, Nakashima M, Nakayama T, et al. (2002) Ets-1 upregulates matrix metalloproteinase-1 expression through extracellular matrix adhesion in vascular endothelial cells. Biochem Biophys Res Commun 291:130-138.
- Eto H, Suga H, Aoi N, Kato H, Doi K, et al. (2012) Therapeutic potential of fibroblast growth factor-2 for hypertrophic scars: upregulation of MMP-1 and HGF expression. Lab Invest 92: 214.
- Huntington JT, Shields JM, Der CJ, Wyatt CA, Benbow U, et al. (2004) Overexpression of collagenase 1 (MMP-1) is mediated by the ERK pathway in invasive melanoma cells role of BRAF mutation and fibroblast growth factor signaling. J Biol Chem 279: 33168-33176
- Shi HX, Lin C, Lin BB, Wang ZG, Zhang HY, et al. (2013) The anti-scar effects of basic fibroblast growth factor on the wound repair in vitro and in vivo. PLoS One 8: e59966.
- Chang YC, Chang MC, Chen YJ, Liou JU, Chang HH, et al. (2017) Basic fibroblast growth factor regulates gene and protein expression related to proliferation, differentiation, and matrix production of human dental pulp cells. J Endod 43: 936-942.
- Chaudhary LR, Avioli LV (2000) Extracellular-signal regulated kinase signaling pathway mediates downregulation of type I procollagen gene expression by FGF‐2, PDGF‐BB, and okadaic acid in osteoblastic cells. J Cell Biochem 76: 354-359.
- Ju W, Zhihong Y, Zhiyou Z, Qin H, Dingding W, et al. (2012) Inhibition of α-SMA by the ectodomain of FGFR2c attenuates lung fibrosis. Mol Med 18: 992-1002.
- Schuliga M, Javeed A, Harris T, Xia Y, Qin C, et al. (2013) Transforming growth factor–β–induced differentiation of airway smooth muscle cells is inhibited by fibroblast growth Factor-2. Am J Respir Cell Mol Biol 48: 346-353.
- Strand DW, Liang YY, Yang F, Barron DA, Ressler SJ, et al. (2014) TGF-β induction of FGF-2 expression in stromal cells requires integrated smad3 and MAPK pathways. Am J Clin Exp Urol 2: 239-248.
- Luo K (2017) Signaling cross talk between TGF-β/Smad and other signaling pathways. Cold Spring Harb Perspect Biol 9: a022137.
- Nishi H, Demir E, Panchenko AR (2015) Crosstalk between signaling pathways provided by single and multiple protein phosphorylation sites. J Mol Biol 427: 511-520.
- Mori S, Takada Y (2013) Crosstalk between Fibroblast Growth Factor (FGF) Receptor and Integrin through Direct Integrin Binding to FGF and Resulting Integrin-FGF-FGFR Ternary Complex Formation. Med Sci 1: 20-36.
- Katoh M, Katoh M (2006) Cross-talk of WNT and FGF signaling pathways at GSK3ß to regulate ß-catenin and SNAIL signaling cascades. Cancer Biol Ther 5: 1059-1064.
- Ruiz-Camp J, Morty RE (2015) Divergent fibroblast growth factor signaling pathways in lung fibroblast subsets: Where do we go from here?. Am J Physiol Lung Cell Mol Physiol 309: L751-L755.
- Forough R, Weylie B, Collins C, Parker JL, Zhu J (2006) Transcription factor Ets-1 regulates fibroblast growth factor-1-mediated angiogenesis in vivo: Role of Ets-1 in the regulation of the PI3K/AKT/MMP-1 pathway. J Vasc Res 43: 327-337.
- Newberry EP, Willis D, Latifi T, Boudreaux JM, Towler DA (1997) Fibroblast growth factor receptor signaling activates the human interstitial collagenase promoter via the bipartite Ets-AP1 element. Mol Endocrinol 11: 1129-1144.
- Barrios R, Pardo A, Ramos C, Montaño M, Ramírez R, et al. (1997). Upregulation of acidic fibroblast growth factor during development of experimental lung fibrosis. Am J Physiol Lung Cell Mol Physiol 273: L451-L458.
- Koo HY, El-Baz LM, House S, Cilvik SN, Dorry SJ, et al. (2018) Fibroblast growth factor 2 decreases bleomycin‐induced pulmonary fibrosis and inhibits fibroblast collagen production and myofibroblast differentiation. J Pathol 246: 54-66.
- Guzy RD, Stoilov I, Elton TJ, Mecham RP, Ornitz DM (2015) Fibroblast growth factor 2 is required for epithelial recovery, but not for pulmonary fibrosis, in response to bleomycin. Am J Respir Cell Mol Biol 52: 116-128.
- Li L, Zhang S, Wei L, Wang Z, Ma W, et al. (2018) FGF2 and FGFR2 in patients with idiopathic pulmonary fibrosis and lung cancer. Oncol Lett 16: 2490-2494.
- Nathan SD, Costabel U, Albera C, Behr J, Wuyts WA, et al. (2019) Pirfenidone in patients with idiopathic pulmonary fibrosis and more advanced lung function impairment. Respir Med 153: 44-51.
- Ryerson CJ, Kolb M, Richeldi L, Lee J, Wachtlin D, et al. (2019) Effects of nintedanib in patients with idiopathic pulmonary fibrosis by GAP stage. ERJ Open Res 5: 00127-2018.
- Jiao H, Song J, Sun X, Sun D, Zhong M (2019) Sodium Arsenite Inhibits Lung Fibroblast Differentiation and Pulmonary Fibrosis. Pharmacology 104: 367-375.
- Luo F, Zhuang Y, Sides MD, Sanchez CG, Shan B, et al. (2014) Arsenic trioxide inhibits transforming growth factor-β1-induced fibroblast to myofibroblast differentiation in vitro and bleomycin induced lung fibrosis in vivo. Respir Res 15: 51.