- (2011) Volume 12, Issue 2
Nicholas S Solanki, Savio George Barreto*
Department of Surgery, Royal Adelaide Hospital, South Australia
Received February 14th, 2011 Accepted February 15th, 2011
Dehydration; Evidence-Based Medicine; Resuscitation; Therapeutics
Dear Sir,
Acute pancreatitis is an acute inflammation of the pancreas associated with a high morbidity and even the risk of mortality [1, 2]. To date, there exists no specific treatment for this disease [3, 4, 5] and fluid therapy forms the cornerstone of management of these patients who present acutely to emergency departments around the world. There is a need to review the data on fluid resuscitation in acute pancreatitis to aid the development of evidence-based guidelines.
A systematic search of the scientific literature was carried out using EMBASE, PubMed/MEDLINE, and the Cochrane Central Register of Controlled Trials for the years 1965-2011 to obtain access to all publications, especially randomized controlled trials, systematic reviews, and meta-analyses involving the various factors related to the use of fluid resuscitation in acute pancreatitis.
The search strategy was that described by Dickersin et al. [6] with the appropriate specific search terms, namely, “acute pancreatitis”, “fluid resuscitation”, “haemoconcentration”, “hemoconcentration”, “fluids”, “pancreatitis”, “systematic”, and “randomized controlled trials”. All available major publications from the past 45 years were considered.
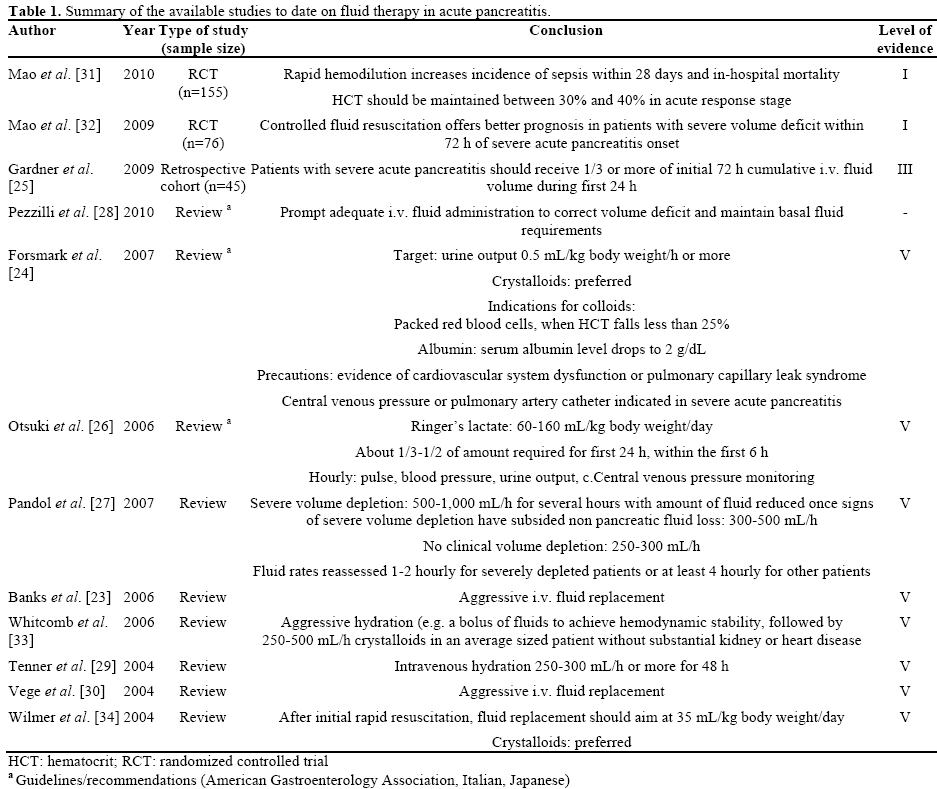
Using the above search strategy, a total of 12 studies were identified describing regimens for fluid therapy. These included two randomized controlled trials, one retrospective cohort study, and 9 reviews.
The impact of retroperitoneal fluid losses and dehydration on the development of hypovolemia seen in patients with severe acute pancreatitis resulting in high mortality was recognized in the 1950s [7, 8]. Although, this fluid loss was largely shown to respond to intravenous fluid therapy [9, 10, 11], the initial understanding was that the shock was mainly due to a loss of red blood cells [12]. Thereafter, despite the link between hemoconcentration at admission and mortality in acute pancreatitis being suggested by Davis et al. [13] and Gray et al. [14], a reduction in hematocrit in the first 48 hours was considered a poor risk factor in acute pancreatitis [15, 16] as evidence by the scoring system proposed by Ranson et al. [11]. Ranson et al. [11] attributed the low hematocrit to pre-existing anemia encountered in alcoholics while Trapnell [16] founds the fall in hematocrit to correlate with internal hemorrhage. The early use of fluid therapy has certainly reduced early mortality in acute pancreatitis associated with hypovolemia. In the 1990s, the importance of hemoconcentration was re-visited by the group from the Brigham and Women’s Hospital in Boston [17, 18]. Since then, hemoconcentration based on a serum hematocrit level at admission has been consistently demonstrated to be linked to the development of pancreatic necrosis [19, 20, 21, 22]. Pancreatic microcirculation depends on circulating volume and responds poorly to other influences.
Human Studies
Table 1 lists the articles/studies involving fluids in acute pancreatitis [23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34], their conclusions, as well as, the level of evidence [35].
The only two randomized controlled trials till date have been based on studies conducted by Mao et al. [31, 32] In their first randomized controlled trial published in 2009, Mao et al. [32] randomized 76 patients within 72 hours of onset of severe acute pancreatitis to undergo either rapid fluid expansion (Group I; n=36) or controlled fluid expansion (Group II; n=40). They found that the patients in Group I had poorer outcomes based on measures such as higher APACHE II scores on days 1, 2, and 3 (P<0.05), greater need for mechanical ventilation (94.4% versus 65%; P<0.05), higher incidence of abdominal compartment syndrome and sepsis (P<0.05), and an overall lower survival rate (69.4% versus 90%; P<0.05).
In the second randomized controlled trial [31], Mao et al. randomized 115 patients within 24 hours of onset of severe acute pancreatitis to either undergo rapid hemodilution (hematocrit less than 35%; n=56) or slow hemodilution (hematocrit equal to 35% or more; n=59) over the next 48 hours. They found a higher incidence of sepsis in the rapid hemodilution group compared to the slow hemodilution group (P<0.01) with significant differences in the time interval to development of sepsis (7.4±1.9 days versus 10.2±2.3 days; P<0.01) in the first 28 days. The survival rate of the slow hemodilution group was also better (84.7% versus 66.1%; P<0.05).
The type of fluids used in the two studies included a combination of crystalloids (normal saline and/or lactated Ringer’s solutions) and colloids (plasma and 6% hydroxyl ethyl starch).
A retrospective cohort study by Gardner et al. [25] examined primary clinical outcomes including mortality, development of organ failure and duration of hospitalization in patients who received more than 33% (early resuscitation; n=17) or less than 33% (late resuscitation; n=28) of their cumulative 72-hour intravenous fluid volume within the first 24 h of presentation. They found that patients in the “late resuscitation” group experienced greater mortality than those in the “early resuscitation” group (18% versus 0%; P< 0.04) and demonstrated a trend toward greater rates of persistent organ failure (43% versus 35%; P=0.31).
Animal Studies
Animal studies conducted over the last four decades [36, 37, 38, 39, 40, 41] have aided our understanding of fluid resuscitation in overcoming microcirculatory disturbances in acute pancreatitis and attenuating endorgan injury. However, in the context of aiding the decision on the choice of fluid in the clinical setting, the results have not been particularly helpful.
Based on the review of literature we can conclude that hemoconcentration in a patient with acute pancreatitis (based on serial measurements of hematocrit) within the first 48 hours of admission is a marker of poor prognosis and indicates the need for fluid resuscitation. The ideal cut-off level for serum hematocrit (44% or 47%) remains to be determined. What can also be concluded from the available literature is that fluid therapy remains the cornerstone in the early management of acute pancreatitis and especially in the prevention of severe acute pancreatitis. In patients who go on to develop severe acute pancreatitis either due to a late presentation or despite resuscitation, fluid therapy has the potential to reduce the progression of pancreatic necrosis and its associated risk of mortality.
In 2008, Gardner et al. [42] reviewed the available evidence on fluid resuscitation in acute pancreatitis and found that there was a paucity of evidence to support clinical recommendations at that time. To date, there continues to be a lack of high-level evidence to guide the ideal “initial” fluid strategy for all patients presenting with acute pancreatitis in terms of choice of fluid, namely crystalloids and/or colloids, and if crystalloids, Ringer’s lactate or normal saline, as well as in terms of rate of administration. While crystalloids appear to be the ideal choice based on expert opinion and the guidelines/recommendations from America, Italy and Japan [23, 24, 26, 27, 28, 29, 30, 33, 34], these recommendations are not based on high-level evidence in patients with acute pancreatitis. In patients with severe acute pancreatitis, the two randomized trials available [31, 32] used a combination of crystalloids and colloids, and favored controlled resuscitation over rapid infusion within the first 72 hours. Considering that both these trials were performed by the same group, these results need to be validated by other groups.
There has been no further impetus even in animal studies since the last major review by Gardner et al. [42]
In conclusion, fluid therapy remains the mainstay of early management of patients with acute pancreatitis and severe acute pancreatitis. High-level evidence is lacking to guide protocols for fluid resuscitation in patients presenting with acute pancreatitis. In those patients with severe acute pancreatitis, the available evidence indicates that controlled fluid resuscitation with crystalloids and colloids offers the best outcome. Hematocrit remains a useful marker to guide fluid resuscitation in acute pancreatitis. However, the timing and ideal “cut-off” level needs to be determined.
None declared