- (2009) Volume 10, Issue 1
John David Horwhat1, Henning Gerke2, Ruben Daniel Acosta1, Darren A Pavey3, Paul S Jowell3
1Gastroenterology Service, Department of Medicine, Walter Reed Army Medical Center. Washington, DC, USA
2Division of Gastroenterology, Department of Medicine, University of Iowa Hospitals and Clinics. Iowa City, IA, USA.
3Division of Gastroenterology, Department of Medicine, Duke University Health System. Durham, NC, USA
Received October 10th, 2008 - Accepted November 14th, 2008
Context The role of EUS to evaluate subtle radiographic abnormalities of the pancreas is not well defined. Objective To assess the yield of EUS±FNA for focal or diffuse pancreatic enlargement/fullness seen on abdominal CT scan in the absence of discrete mass lesions. Design Retrospective database review. Setting Tertiary referral center. Patients and interventions Six hundred and 91 pancreatic EUS exams were reviewed. Sixty-nine met inclusion criteria of having been performed for focal enlargement or fullness of the pancreas. Known chronic pancreatitis, pancreatic calcifications, acute pancreatitis, discrete mass on imaging, pancreatic duct dilation (greater than 4 mm) and obstructive jaundice were excluded. Main outcome measurement Rate of malignancy found by EUS±FNA. Results FNA was performed in 19/69 (27.5%) with 4 new diagnoses of pancreatic adenocarcinoma, one metastatic renal cell carcinoma, one metastatic colon cancer, one chronic pancreatitis and 12 benign results. Eight patients had discrete mass lesions on EUS; two were cystic. All malignant diagnoses had a discrete solid mass on EUS. Conclusions Pancreatic enlargement/fullness is often a benign finding related to anatomic variation, but was related to malignancy in 8.7% of our patients (6/69). EUS should be strongly considered as the next step in the evaluation of patients with focal enlargement of the pancreas when clinical suspicion of malignancy exists.
Diagnostic Techniques, Digestive System; Endosonography; Pancreatic Neoplasms
The significance of focal enlargement or fullness of the pancreas as the only finding on CT scan in patients lacking other objective signs or symptoms of pancreatic disease has not been well established. Unfortunately, based on radiographic imaging alone, malignancy cannot be definitively ruled out in these patients and additional diagnostic modalities are indicated to reliably discern a malignant cause from other potentially benign diagnoses to include prominent ventral anlage, acute and chronic pancreatitis, pancreas divisum, lipomatous pseudohypertrophy and granulomatous disease [1, 2, 3, 4, 5, 6].
When considering the most appropriate next test to follow an inconclusive CT, it is important to evaluate how such a test compares to a gold standard: surgical pathology or long term follow-up. EUS has previously been shown to be superior to CT in the evaluation of pancreatic cancer, with EUS demonstrating greater accuracy than both dynamic CT and MRI in the diagnosis of pancreatic tumor, and better sensitivity and specificity, particularly for tumors less than 3 cm in diameter [7]. EUS is also highly sensitive in detecting pancreatitis [8] and even small pancreatic masses that are overlooked on other cross sectional imaging modalities [9]. The performance characteristics of EUS-FNA demonstrate superiority even after other evaluations fail to yield a diagnosis. It has been suggested that EUS-FNA may play a role in the evaluation of a pancreatic mass, when results of other biopsy methods are negative, but pancreatic cancer remains highly suspected. A study of EUS-FNA in patients suspected of pancreatic cancer by Gress et al. demonstrated a posterior probability of pancreatic cancer after a definitely positive result of 93.5%, and after a definitely negative result of 6.9% [10]. EUS does have limitations in the setting of chronic pancreatitis and in these patients it may be difficult to accurately differentiate between benign and malignant lesions [11].
False negative EUS examinations are very rare, and in the absence of chronic or recent acute pancreatitis a normal EUS typically excludes pancreatic cancer with confidence [11, 12, 13]. At our institution, we noted an increasing demand for EUS to investigate subtle radiographic abnormalities of the pancreas. Interestingly, the utility of EUS for investigating focal pancreatic enlargement or fullness on CT in the absence of other findings suggesting pancreatobiliary disease has not well been studied. This prompted us to analyze our experience with EUS for this indication.
We reviewed our endoscopic database for patients that were referred to us for pancreatic EUS exams performed from January 1998 to November 2003 for the following indications: focal or diffuse fullness of the pancreas on abdominal computed tomography (CT) or trans-abdominal ultrasound exam. After collecting these examinations, we carefully reviewed the clinical notes that were available for these patients. We sought to specifically analyze those patients where the initial imaging studies performed by the referring physicians were not strongly suggestive of malignancy and EUS was being used to investigate for other heretofore undiagnosed pancreatic pathology. Patients with a known history of chronic pancreatitis, pancreatic calcifications, recent acute pancreatitis (within the previous 6 weeks), discrete mass (solid or cystic) on radiographic imaging, pancreatic duct dilation (greater than 4 mm) and obstructive jaundice were excluded. EUS reports were then reviewed and classified as negative (no evidence of pancreatic disease), pancreatic mass, acute/chronic pancreatitis according to previously published EUS criteria [8], or minimal pancreatic parenchymal changes. The patients’ past medical history, clinical presentation, laboratory tests (liver associated enzymes, amylase and lipase), and prior imaging (ERCP, trans-abdominal ultrasound, MRI) were obtained from review of the patient’s electronic and paper charts held in the DUMC Gastroenterology Division.
Patients with normal EUS or minimal non-specific parenchymal changes such as hyperechoic foci, hyperechoic strands or lobularity (but no mass lesion) were mailed a follow-up questionnaire asking patients whether they had any additional evaluation for their pancreas since originally seen by the DUMC EUS service, and if so, what was found. A stamped envelope with the DUMC EUS Service address was included with the questionnaire for the purpose of collecting this information.
Our endoscopic database was reviewed after approval by the Duke University Medical Center (DUMC) Investigational Review Board.
Data from the electronic data base, chart review and returned follow-up questionnaires were placed into a Microsoft Excel database and correlated with the EUS findings. Mean, standard deviation (SD), range and frequencies were used as descriptive statistics. For comparison of proportions the Fisher’s exact test was used. A two-tailed P value less than 0.05 was considered significant.
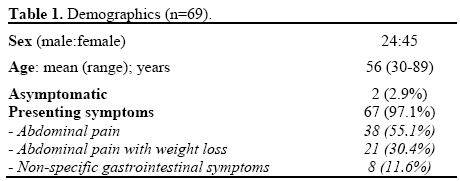
We reviewed 691 patient records with 69 meeting inclusion criteria. Exactly 34.8% (24/69) were male with a mean age of 56 years (range 30-89 years). Presenting symptoms were predominantly abdominal pain alone (n=38, 55.1%) or abdominal pain with weight loss (n=21, 30.4%). Non-specific GI symptoms were present in 8 patients (11.6%) with an additional 2 patients (2.9%) endorsing no abdominal symptoms at all (their CT scans were done for other purposes and the pancreatic findings of fullness were incidental) (Table 1).
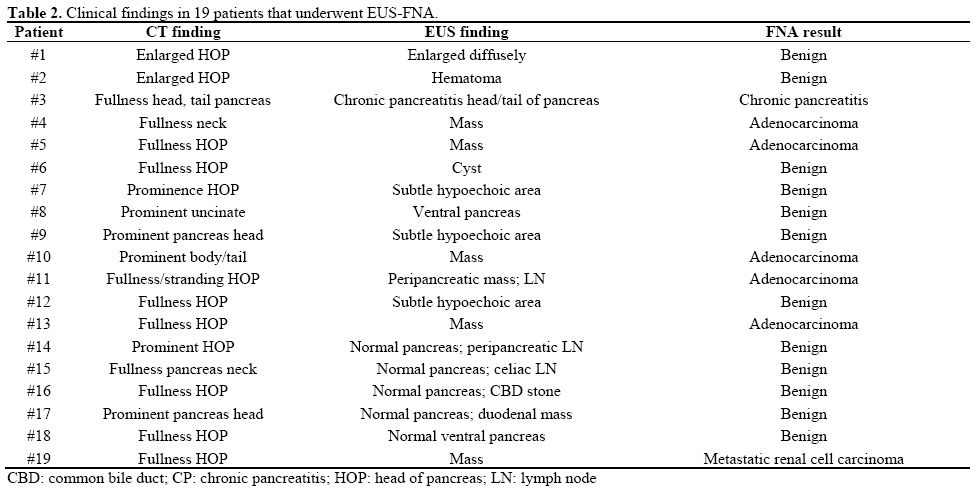
Fine needle aspiration was performed in 19 patients (27.5%; Table 2). An on-site cytopathologist is standard for our facility, and all specimens were deemed adequate for interpretation prior to termination of the procedure. Indications for FNA included the appearance of a discrete solid mass during EUS in 6 patients (31.6%), cystic lesion in one patient (5.3%) and nonspecific parenchymal abnormalities in the remaining majority (n=12; 63.2%). Following EUS FNA, 4 (21.1%) new diagnoses of pancreatic adenocarcinoma, one (5.3%) metastatic renal cell carcinoma, one (5.3%) metastatic colon cancer and one (5.3%) chronic pancreatitis, were made; therefore, 12 patients undergoing EUS FNA had benign histopathologic results (63.2%). The majority of our patients with EUS features consistent with chronic pancreatitis (8 of 9, 88.9%) did not have a mass lesion or features suspicious enough to warrant FNA.
Despite the suggestion of pancreatic fullness or enlargement on cross sectional imaging, the majority of our cohort (45/69; 65.2%) had a normal EUS examination of the pancreas (Figure 1). In contrast, all new diagnoses of malignancy were associated with a discrete mass lesion on EUS. There was no difference seen among those patients that had had contrastenhanced pancreatic CT scan from those that had a non-contrast CT scan: 5 of the malignancies (8.3%) that were detected at EUS were from 60 i.v. contrastenhanced CT scans versus one malignancy (11.1%) from 9 non-contrast CT scans (P=0.582).
Clinical follow-up in the form of returned questionnaires, telephone interview, or review of patient records was available on 31/69 patients (44.9%) with a mean (±SD) follow-up time of 31.5±13.4 months. Long term clinical follow-up for these patients - which includes 4 of the 12 patients with benign EUS FNA results - revealed no new interval diagnoses. Follow-up was considered complete for the 6 patients that had malignancy diagnosed during the initial EUS examination and these patients were not mailed followup questionnaires.
The discovery of malignancy in 8.7% (6/69) of our cohort was nearly identical to the data from a recent study by Ho et al. who reported that the majority of patients presenting with “fullness” or enlargement of the pancreas had benign disease, but 8% had pancreatic cancer. Elevated CA 19-9 and weight loss were predictive of pancreatic malignancy. Based on this study, they concluded that EUS and EUS-FNA are safe and accurate diagnostic tests that play an important role in evaluating patients with this clinical concern [14]. While our follow-up was not as complete as the cohort studied by Ho et al., the similar findings lend credibility to our results and favor a more generalized applicability to the use of EUS for patients with fullness of the pancreas. Both the study by Ho et al. and ours used criteria that served to exclude patients with obvious radiographic signs of pancreatic cancer. In contrast to the recent studies by Walker et al. [15] and Agarwal et al. [16] we made specific efforts to exclude patients where biliary obstruction, a dilated pancreatic duct, a cystic lesion or other features that carry a strong association with an underlying mass were present. Since it is not unusual for pancreatitis to lead to diffuse or focal enlargement of the pancreas, patients with strong indicators for chronic or recent acute pancreatitis were excluded as well. Thus, we studied a cohort of patents in whom there was no obvious explanation for the pancreatic enlargement or fullness.
While conducting this database analysis, the Duke Biliary Service had recently concluded a prospective randomized study comparing CT-guided FNA to EUSguided FNA in the evaluation of pancreatic masses, and a notable finding of this work was the ability for EUS to discern small masses that were sometimes overlooked on other radiographic studies like CT [17]. The results from this study demonstrated to us that some malignancies may not be readily apparent to the radiologist and subtleties such as fullness or an irregular border may be the only manifestations of underlying malignancy on CT scan. This was, in part, the impetus for our current study. It is interesting to note, therefore, that all of the cancers diagnosed by EUS FNA were seen as a discrete mass by EUS. Taking the time to review a CT scan with an expert gastrointestinal radiologist is of paramount importance and may lead one to pursue additional studies such as EUS rather than accepting a study as a variation of normal [18].
We acknowledge that a limitation of our study was its reliance upon the quality of records sent by referring physicians. In these instances, radiographic reports did not always allow us to ascertain whether the imaging study was conducted on a multi-detector array (spiral) CT scanner (MDCT) or whether the protocol of the exam was with fine cuts and an appropriately timed intravenous contrast bolus (i.e. the “pancreatic protocol” study). Included in our analysis were 9 patients that had non-contrast CT scans (one of whom had a malignancy found at EUS). Although we found no significant difference between the rate of malignancy detected on contrast-enhanced versus noncontrast CT studies, we acknowledge that it is unfair to report superiority for EUS over a non-contrast CT of the pancreas. In fact, it is even possible that future refinements in CT imaging (respiratory-gated or 4- dimensional imaging) may even reduce the benefit that is seen with EUS over CT scan in this study. However, even with MDCT some tumors may remain isodense to the surrounding pancreas and therefore difficult to detect with this modality. While, for the sake of research, the radiographic limitations of our study may appear a weakness, in fact, these issues more likely reflect the real-life practice for the majority of gastrointestinal physicians that are asked to consult on patients with vague pancreatic abnormalities and for whom our results may therefore have even greater significance.
We acknowledge that the retrospective nature of this study is an additional limitation and the findings are prone to selection bias. In the absence of definitive FNA results on all 69 patients, repeat EUS FNA or surgical pathology, we tried multiple times to contact the patients that had undergone EUS with a normal or non-malignant FNA. Unfortunately, due to the distances that patients often traveled to reach our institution, insurance issues, or patient satisfaction that their prior symptoms had resolved, we were unable to obtain additional follow-up information from the majority of the 63 patients that did not have malignancy. The patients that give the greatest cause for concern are those in whom chronic calcific pancreatitis is present and a mass lesion may be difficult to appreciate. Only 1 of our 9 patients with chronic pancreatitis diagnosed by EUS criteria had clinical suspicion to warrant EUS FNA. No mass was present. In the absence of chronic pancreatitis, pancreatic cancer is rarely missed on EUS [11], and in two studies the negative predictive value of a normal EUS was 100% [12, 13]. We submit that based on this evidence it is not unreasonable to assume that our 45 patients with a normal EUS did not have cancer, and one might argue that confirmatory follow-up information would not be required in such a patient. If, however, occult malignancy was present and somehow missed by our initial EUS (i.e. false negative EUS FNA), the rate of malignancy due to enlargement or fullness at CT scan may be even higher than the 8.7% that we report. We suggest an algorithm (Figure 2) that addresses the need for continued surveillance in patients with non-specific findings (to include those with chronic pancreatitis).
An additional criticism of our study may be the highly selective nature of our population. We would argue, however, that our study population exemplifies exactly the type of patients that would be presenting to a physician for abdominal imaging (unexplained abdominal pain, with or without weight loss was present in 85.5% of our cohort). Certainly the decision to undergo an exploratory surgery for the suspicion of possible occult malignancy in the context of a dilated pancreatic duct, underlying chronic pancreatitis or coexisting dilated bile duct (“double duct”) is far easier to justify than for mere fullness or focal enlargement. Prior to this study, it can be argued whether one would have considered the likelihood of an 8.7% chance of underlying malignancy. In our opinion, excluding patients with characteristics that are more likely to be associated with an underlying pancreatic malignancy only serves to strengthen the conclusion that EUS serves a useful purpose “especially” in patients with vague cross-sectional imaging studies.
In summary, despite its limitations, this study represents the largest cohort to date investigating the relevance of non-specific enlargement or fullness of the pancreas on CT scan. In agreement with previously published data, our results support the value of EUS±FNA for this indication. We strongly recommend considering EUS as the next step in the diagnostic evaluation, if there is not an otherwise obvious explanation for the CT finding that would indicate the need for surgical exploration.
The authors have no potential conflicts of interest. The views expressed in this article are those of the author(s) and do not reflect the official policy of the Department of Army, Department of Navy, Department of Defense, or U.S. Government