Case Report - (2017) Volume 18, Issue 2
1Institute of Gastroenterology, 2Departments of Internal Medicine A, 3Internal Medicine E, 4General Surgery in Galilee Medical Center and 5Administration of Galilee Medical Center, 6Faculty of medicine in the galilee, safed, Israel
Received December 13th, 2016 - Accepted January 06th, 2017
Percutaneous endoscopic gastrostomy has become the preferred method to provide nutritional support for patients requiring long term enteral feeding due to its ease and safety of placement. The estimated prevalence is about 18-34% among nursing home residents with advanced cognitive impairment. Complications of percutaneous endoscopic gastrostomy placement may be minor or major but the most are minor with average rates of 16-70% in different reports. Procedure related mortality rate is 0-0.2%. In this paper we present a case of 46 nursing home resident who was fed through percutaneous endoscopic gastrostomy for several years which was replaced by Foley catheter due to accidental dislodgement of the tube several weeks ago. She was admitted to internal medicine ward for black colored vomiting and impacted nonfunctional Foley catheter. Vital signs were normal at her admission and abdominal tenderness at the epigastric region was found. Blood tests revealed elevated Liver Enzymes and elevated LIPASE X 8 of upper Normal limit. She was diagnosed with pancreatitis and treated with NPO and IV Saline. Abdominal computed tomography revealed dilated gall bladder, with prominent Wirsung and common bile ducts and a peripancreatic fluid around the pancreatic tail. A replaced catheter tip was seen in the descending duodenum with no evidence of bowel obstruction. Fluoroscopy showed contrast in the small bowel with feeding tube tip in the same region. Gastroscopy revealed migration of the Foley catheter distally to the second portion of the duodenum with catheter balloon stuck to the major papilla causing a pressure ulcer in the papilla. The balloon was deflated and the catheter was replaced by balloon replacement tube gastrostomy. Biopsies taken from the ulcerated papilla showed ulcerated small bowel mucosa with acute and chronic inflammatory cells. Two days later, enteral feeding and her chronic medications were resumed with no complications and she was disharged home. Received December
Pancreatitis
CT computed tomography; NPO nil per os; PEG percutaneous endoscopic gastrostomy
Since its first description by Guadener in 1980 [1], percutaneous endoscopic gastrostomy – PEG placement, has become the preferred method to provide nutritional support for patients requiring long term (more than 4-6 weeks ) enteral feeding, due to its ease and safety of placement [2]. The prevalence of PEG tube placement is increasing [3]. Its estimated prevalence among nursing home residents with advanced cognitive impairment is about 18-34% [4, 5, 6]. Complications of PEG placement may be minor (wound infection, minor bleeding) or major (necrotizing fasciitis, colocutaneous fistula), but most of the complications are minor. The reported rates of complications following PEG placement vary from 16- 70% in different reports [7, 8, 9, 10, 11]. They are more likely to occur in older adults with comorbid illnesses, particularly those with an infectious process or who have a history of aspiration [10]. The procedure related mortality is 0-0.2% [8]. Complications may be early, seen immediately following PEG tube placement, late seen after the gastrostomy tract has matured, or complications that may occur at any time and they include tube dysfunction, infection, bleeding, peristomal leakage, ulceration, gastric outlet obstruction and inadvertent gastrostomy tube removal [7, 8, 9, 10, 11].
A Forty-six-year-old female, a resident of a nursing home who suffers from primary amyloidosis, dementia and status post cerebrovascular accident with left hemiplegia, has been nourished through percutaneous gastrostomy tube in the last several years, which was replaced by Foley catheter due to accidental dislodgement of the tube several weeks ago. Her chronic medications are proton pump inhibitors (PPI), Benzodiazepines & anti epileptics with no recent use of any other drug. She was admitted to the internal medicine ward for evaluation of black colored vomiting and impacted nonfunctional Foley catheter used as feeding tube without melena or fever. At admission her vital signs were normal, and abdominal tenderness at the epigastric region was found with no pathologic bowel sounds.
Blood tests were as follows - Hct=41.6 (36-54), Hb=13.7 g/dL (12-16 g/dL), WBCs=8.9 × 103/μL (4-10 × 103/μL), PLT=215 × 109/L (130-400), BUN=17 mg/dL (7- 18 mg/dL), Creatinine= 0.4 mg/dl (0.5-1.02 mg/dl), K=4 mEq/L (3.5-5.1 mEq/L), Na=141 mEq/L (135-145 mEq/L), Cl=106 mEq/L (98-107 mEq/L), ALT=199 U/L (0-55 U/L), AST=178 U/L (5-34 U/L), ALP=185 U/L (40-150 U/L), GGT=200 U/L (9-36 U/L), Lipase=636 U/L (8-78 U/L), BILIRUBIN=0.3 mg/dL (0.3-1.2 mg/dL)
In a presumptive diagnosis of acute pancreatitis she was treated with nil per os (NPO) and intravenous (IV) normal saline. In the second hospitalization day a contrast enhanced abdominal computed tomography (CECT) was done (Figures 1, 2), and revealed dilated gall bladder, with prominent Wirsung and common bile ducts, a peripancreatic fluid around the pancreatic tail as a sign of acute pancreatitis without pancreatic necrosis. There was no cholelithiasis or choledocholithiasis. A replaced catheter tip was seen in the descending duodenum with no evidence of bowel obstruction. The Balthazor grade of pancreatitis was D and the computed tomography severity index (CTSI) was 3 points.
Fluoroscopy (Figure 3) was done one day later, and showed contrast in the small bowel with feeding tube tip in the same region. Id the same day a gastroscopy (Figures 4, 5, 6) was done and it revealed migration of the Foley catheter passing through the pylorus distally to the second portion of the duodenum with catheter balloon stuck to the major papilla and causing a pressure ulcer in the papilla.
The balloon was deflated and the catheter was removed and replaced by balloon replacement tube gastrostomy. Biopsies taken from the ulcerated papilla showed ulcerated small bowel mucosa with acute and chronic inflammatory cells, granulation tissue and necrotic inflamed material from ulcer base. Her medical condition improved dramatically without vomiting or fever and her vital signs were normal. Hemoglobin was within normal range, and lipase normalized.
Two days later, enteral feeding and her chronic medications were resumed with no complications, and the day after she was discharged with a diagnosis of acute pancreatitis due to mechanical compression of the papilla from migrating Foley catheter introduced to feed the patient instead of inadvertently dislodged tube.
PEG placement; has become the modality of choice of enteral feeding for patients requiring long term enteral feeding. Its placement is considered easy and safe [2], and a growing number of nursing home residents and Medicare patients over the age of 85 years are being fed by PEG [2].
This procedure, though considered safe, can be complicated with early, late, minor and major complications and complications that may occur at any time [7, 8, 9, 10, 11].
One complication that may occur at any time is gastrostomy tube inadvertent removal if traction is placed on tube. This common complication usually occurs in a combative or confused patient who may pull the tube. If the gastrostomy tube has time to mature (i.e. at least four weeks old), and a dedicated replacement tube is not available, a Foley catheter may be placed through the gastrostomy tract as a temporary replacement for the gastrostomy tube in order to prevent tract closure would otherwise begin within 24 hours.
Ulceration related to the gastrostomy tube can occur at any time and may develop underneath the internal bolster, or on the contralateral gastric wall from the site of the gastrostomy tube with balloon gastrostomy replacement tubes [12].
Gastrostomy tubes can migrate forward into the duodenum at any time after PEG placement, and cause gastric outlet obstruction [13]. This occurs if the external bolster on the gastrostomy tube is not attached to the abdominal wall allowing the gastrostomy tube to slide forward through the gastrostomy tract into the duodenum. A similar problem has been reported with balloon gastrostomy tubes where the inflated balloon is allowed to migrate through the pylorus resulting in obstruction [14]. Migration also has been associated with using tubes without external bumpers, or using Foley catheter G-tubes. The underlying mechanism of tube migration is thought to be intestinal peristalsis which carries the tube through the duodenum [15].
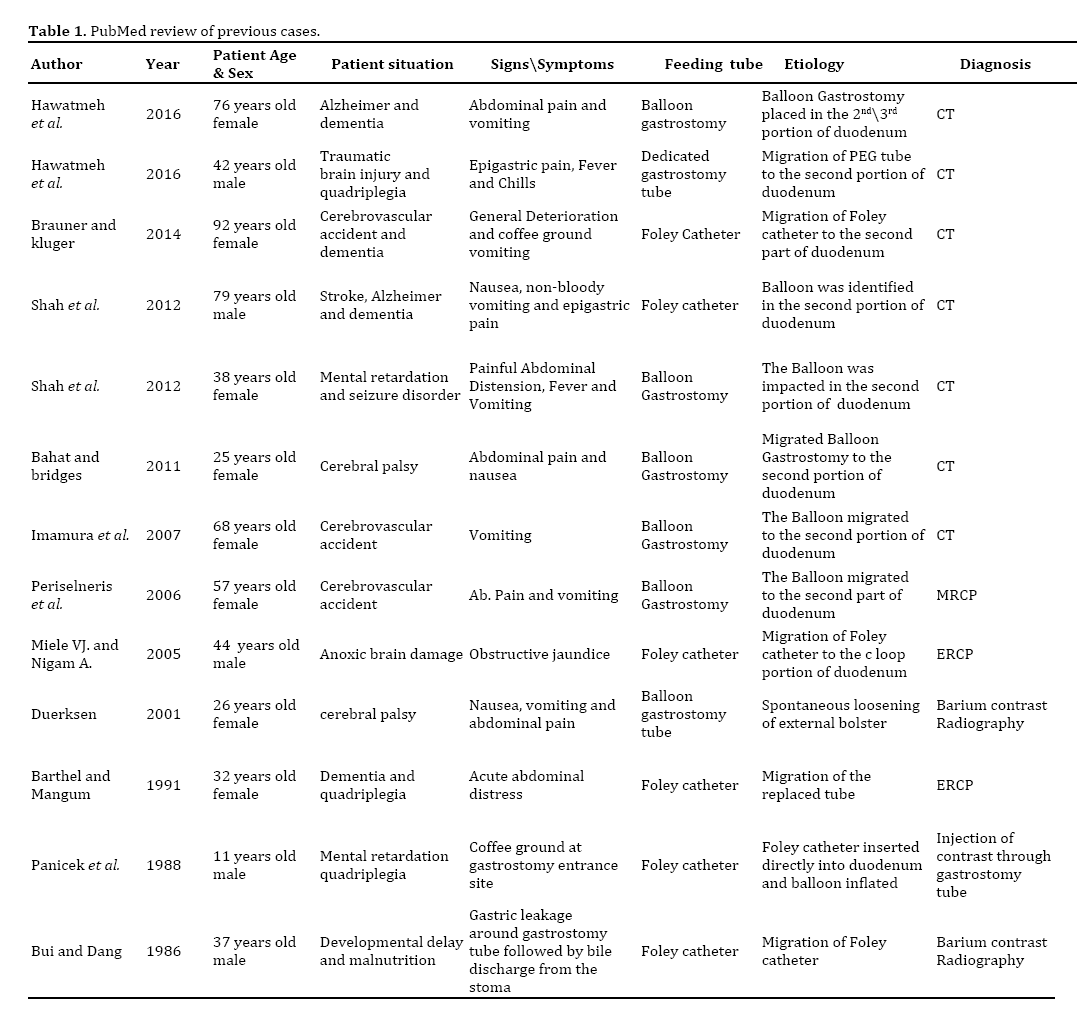
Acute pancreatitis caused by mechanical obstruction of the major papilla secondary to G-tube migration seems to be rare and infrequently reported entity in the English literature. In 1986 Bui and Dang reported the first case of acute pancreatitis caused by inflated balloon of a Foley catheter G-tube migrating into the duodenum [16]. A PubMed search identified 12 cases since their first report (Table 1) [17, 18, 19, 20, 21, 22, 23, 24, 25, 26].
This rarely reported complication appears to be more common when a balloon type placement gastrostomy tube is used, and even more common when a Foley catheter is used as a replacement tube [24, 25]. The presence of a water filled balloon on the end of the gastric tube allows the gastric peristalsis to propel the balloon and forward the tube. Foley catheters tend more to migrate because they lack the external bumper which secures the tube to the abdominal wall, and they lack markings on the catheter surface that allows measuring the depth of balloon placement which may lead to inadvertent inflation of the balloon on the duodenum [24].
The case presented here highlights the recommendation made by others [24, 25] to prevent this complication by using Foley catheters only as temporary replacement tube where dedicated tubes are lacking in order to maintain the integrity of the tract, and to replace it with a dedicated tube as soon as possible. In cases where Foley catheters are used, they should be marked to determine the depth of insertion prior to inflation and be secured to the abdominal wall. A radiographic confirmation of the tube is recommended before initiation of feeding, if there is a doubt about its location [24].
Expert guidelines recommend avoiding placement of catheters or tubes not intended for use as enteral feeding devices, such as urinary or gastrointestinal drainage tubes which usually are without external anchoring device. Their use leads to internal misconnection and tube migration [27]. This rare complication of acute pancreatitis caused from migrating feeding tube is scarcely reported in the English literature. To the best of our knowledge, this is the first case to document endoscopically the mechanical obstruction of the major papilla by the G-tube balloon and a papillary ulcer produced by the balloon with biopsy proven inflammation.
In summary, most of these cases could be prevented by using dedicated feeding tubes, and in cases where it is not available, the use of Foley catheter should be temporary and must be replaced by a dedicated tube as soon as possible. In any doubt about the location of the tube tip, a gastrografin film should be done to confirm its location before initiating feeding. Awareness to this potentially fatal complication is very important since early diagnosis and treatment can be crucial.
The authors declare that they have no competing interests.