Case Report - (2022) Volume 6, Issue 8
Gastric Leak Treated by Endoscopic Gastric Bypass with Metal Stent in Stent Technique in Normal Volume Stomach (Outside Bariatric Setting): First Case Report
Praneeth Moka1*,
Vijay Kumar L2,
Sarath Kumar Reddy A3,
Sharath Reddy A4,
Anil Krishna G4 and
Kiranmai Mynampati5
1Department of Gastroenterology, Medicover Hospitals, Telangana, India
2Department of Radiodiagnosis, Medicover Hospitals, Telangana, India
3Department of General Surgery, Medicover Hospitals, Telangana, India
4Department of Cardiology, Medicover Hospitals, Telangana, India
5Department of Radiodiagnosis, Medicover Hospitals, Telangana, India
*Correspondence:
Praneeth Moka,
Department of Gastroenterology, Medicover Hospitals, Telangana,
India,
Tel: +91-9968996285,
Email:
Received: 01-Aug-2022, Manuscript No. IPJCGH-22-14100;
Editor assigned: 03-Aug-2022, Pre QC No. IPJCGH-22-14100 (PQ);
Reviewed: 17-Aug-2022, QC No. IPJCGH-22-14100;
Revised: 22-Aug-2022, Manuscript No. IPJCGH-22-14100 (R);
Published:
29-Aug-2022, DOI: 10.36648/2575-7733.6.8.40
Abstract
A 35 year old gentleman, a citizen of Yemen, had multiple bullet injuries to the right side of his abdomen on 27th February
2022. He was operated in Yemen on the same day. As reported in the operative notes from Yemen; exploratory
laparotomy with splenectomy, gastric wall repair, duodenal wall repair, diaphragm repair and transverse loop colostomy
were done. Multiple drains were placed in the abdomen to evacuate hematomas and collections. A second
look laparotomy was performed on the 10th March 2022, in view of persistent purulent discharge from the drains
and also from the midline wound. And on 19th March 2022, the mid line wound was found to have dehisced, leading
to further re-exploration and debridement of left diaphragm region, colostomy site and left side chest wound
region. Computerised Tomography (CT) of abdomen done on 29th March 2022, in Yemen, revealed minimal amount
of fluid in the left subphrenic and peri gastric region. He presented to us in India, on 23rd April 2022, with nonhealing
midline abdominal and left chest wounds, with pus discharge. He complained that orally ingested food was coming
out immediately from the left side chest wound and from the midline wound in the abdomen, since the time he was
allowed oral diet after his initial surgery. Hence, he was placed on total parenteral nutrition (TPN) for most of the
time since the first surgery, at the end of February 2022. Despite being on parenteral nutrition, and nil oral intake,
the left chest wound continued to produce approximately 150 mL of pus per day, which was compounded by leaky
midline wound.
Keywords
Endoscopic; Metal Stent; Gastric leak; Esophagus
Introduction
On examination, he was thin built, conscious and oriented with
respiratory rate of 24 per minute and heart rate of 130 per minute.
His blood pressure was 100/70 mm Hg, and was afebrile.
The dehisced midline laparotomy wound was draining pus. The
colostomy bag on left side of abdomen was draining faces. The
left side chest wound was draining frank pus. Left pleural fluid
analysis revealed the presence of 70,000 White blood cells/
microL with neutrophil predominance and triglycerides of 94
mg/dL.
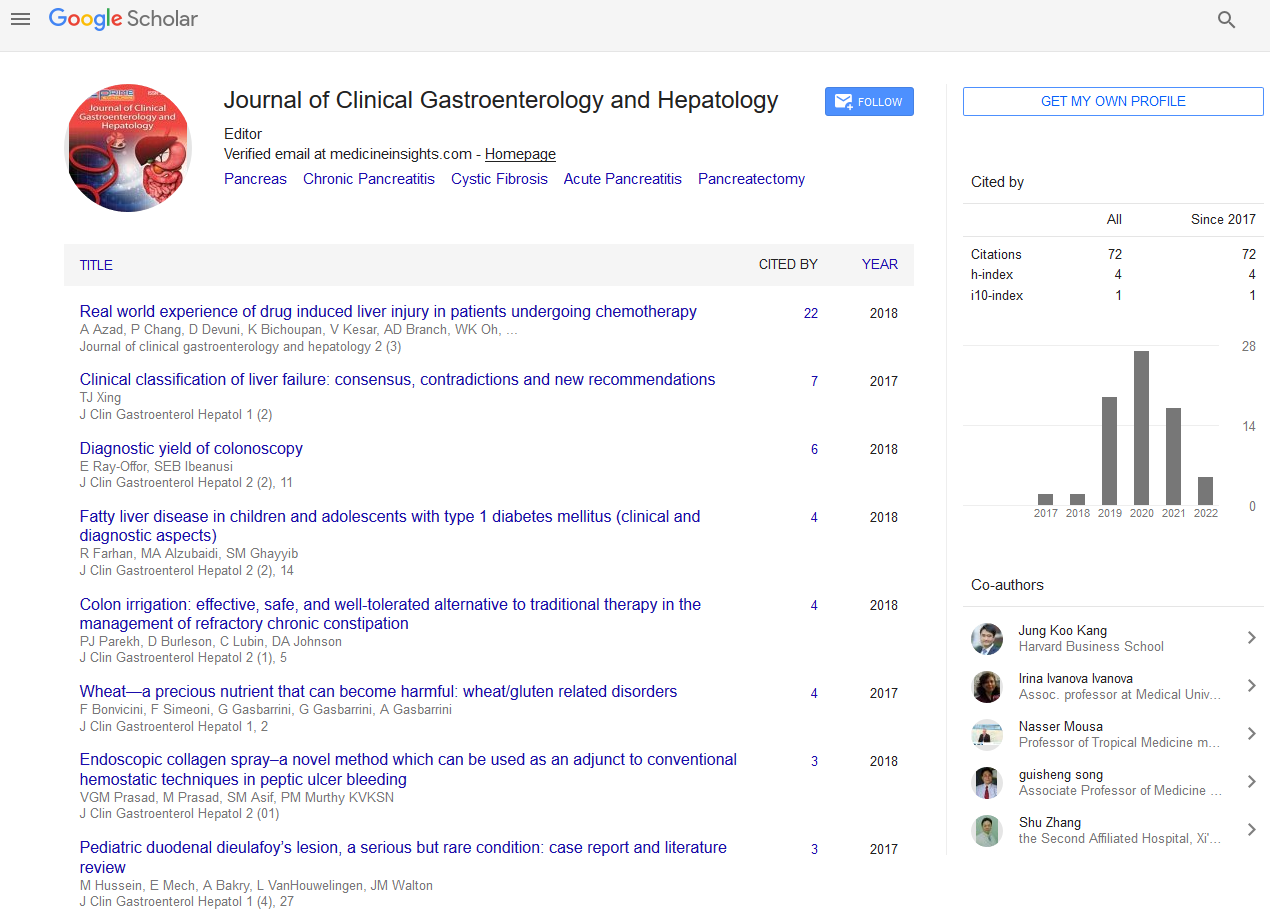
CT abdomen performed on 23rd April 2022, revealed a large defect at greater curvature of body of stomach with contrast leaking
into peritoneal cavity, which was extending inferiorly in the
left paracolic region up to the colostomy site (Figure 1). Thick
walled peripherally enhancing fluid collections with significant
inflammatory changes were noted in the left paracolic region
and in the pelvis.

Figure 1: CT abdomen shows leak of orally ingested contrast from gastric defect in A) axial view.
On 26th April 2022, Upper Gastrointestinal (UGI) endoscopy revealed
a large defect (of nearly 4 cm), with surrounding gross
edema and necrosis, in greater curvature of stomach, in the
mid aspect of body region, communicating with peritoneal
cavity. There was pus seen draining from stomach to peritoneal
cavity. The endoscope could easily pass into the peritoneal
cavity. The size of the defect or gastric fistula was large. A prolonged
period of conservative therapy, with nil oral intake and
total parenteral nutrition was ineffective. Surgery was considered
difficult. Potential alternative option of endoscopic management
was considered.
Case Presentation
On 26th April 2022, Ovesco over the Scope (OTS) clip (Ovesco
Endoscopy AG, Tuebingen, Germany) Size 11, was applied over
the defect, with the help of a twin grasper. Two Olympus EZ
clips (Olympus Medical Systems India Pvt Ltd) were also applied
over the margins of the defect. The pus was still draining
into the peritoneal cavity freely. A guidewire was introduced
through the endoscope up to duodenum. Over the guidewire,
the Niti-S Mega Gastrointestinal stent (TaeWoong Medical,
Gyeonggi-do, South Korea) sized 24 × 230 mm was placed over
the guidewire up to distal body of the stomach. Two Olympus
EZ clips were applied to connect the proximal edge of the mega
esophageal stent to the esophageal mucosa.
On the day after endoscopic intervention, the patient had persistent
leak from chest wound, draining approximately 80 mL
of pus and continued leaky wet midline abdominal wound. The
patient also had regurgitation and vomiting. CT abdomen, repeated
on 26th April 2022, revealed persistent leakage of oral
contract from the gastric defect, and continued leakage from
midline wound and also from the wound in the left side of
chest. The patient was continued on TPN for next 5 days. His
regurgitation decreased over the next few days. The patient
then developed fever (maximum temperature: 102°F). Blood
culture revealed Enterococcus fecium sensitive to Linezolid.
Intravenous Linezolid and change of central venous catheter
helped fever to settle in the following 3 days. The patient and
family were counselled regarding a further endoscopic attempt
to control the deteriorating clinical situation.
On 3rd May 2022, Olympus CV-150 colonoscope was introduced
through the existing esophagogastric stent up to distal body of
the stomach. A guidewire was introduced up to the second
part of duodenum. The Niti-S™ Esophageal TTS (Through The
Scope) Stent (TaeWoong Medical, Gyeonggi-do, South Korea)
(18 mm × 120 mm), with 24 mm wide flares, was placed up to
first part of duodenum, with proximal part of stent positioned
at the level of 2 cm inside the distal part of previously placed
stent. Three Olympus EZ clips (Olympus Medical Systems India
Pvt Ltd), were applied at the edges of the two stents at the site
of approximation of stents.
On 4th May 2022, a day after the latest endoscopic stenting,
clinically the chest wound output and leak from the abdominal
wound stopped completely. CT abdomen, repeated on 4th
May 2022, showed two stents together from esophagus to D1,
with only minimal extravasation of oral contrast (Figure 2). The
patient was allowed oral diet from 4th May 2022. There was no
leak of orally ingested contents. His wounds became dry. He
was discharged on 7th May 2022. His wound outputs remained
nil, and both the abdominal and chest wounds showed significant
healing. On 28th June 2022, both the stents were removed
endoscopically. There was no extravasation of oral contrast.
The wounds remained dry. CT abdomen, repeated on 29th June
2022 showed no abdominal collections and no extravasation of
contrast (Figure 3). The patient underwent colostomy closure
on 6th July 2022. The patient is asymptomatic at follow-up.

Figure 2: CT image shows stent-in-stent from esophagus to duodenum, with minimal extravasation of contrast through the gastric defect, in A) Axial and B) Sagittal views.

Figure 3: CT image shows no extravasation of oral contrast (after removal of stents), in A) Coronal and B) Axial views.
Results and Discussion
Gastric leak is a complication known to occur in 0.5%-3% of
patients after laparoscopic sleeve gastrectomy, due to a long staple line and high intraluminal pressure [1]. Gastric leak is
encountered in 0.7% of patients after Roux-En-Y Gastric Bypass
(RYGB) [2]. Postoperative gastro-jejunal anastomotic leak has
been reported in 1%-10% of patients after gastrectomy [3].
Gastric perforation has also been reported to complicate splenectomy
[4]. Leakage of orally ingested food through abdominal
wounds suggested the presence of communication of the
wound with upper gastrointestinal tract (GIT), and not merely
a surgical site infection. The leak of orally ingested contents
and of salivary and gastric secretions, into left chest and midline
wound, might be the reason for dehiscence of laparotomy
wound and nonhealing chest wound. The leak did not heal even
though the patient was not given anything by mouth since the
time of injury. Treating this leak successfully, and allowing oral
intake subsequently, had the potential to heal the wounds.
The possible reasons for gastrocutaneous fistula (or gastric
leak) could be ischemia during splenectomy, hematoma, staple
misfiring, or less likely due to direct damage to the stomach
by the bullet, needing intervention on the stomach. Laparotomy
for abdominal trauma, especially for multiple gunshot
wounds, requiring a damage control surgery, added by the
need for emergency splenectomy due to hemoperitoneum,
could potentially compromise operative field visibility, leading
to damage to short gastric arteries and left gastro epiploic artery
branches [5]. Also, poor visibility due to the presence of lot
of blood, intraoperatively, could have resulted in gastric tissue
being crushed by forceps, causing tissue ischemia and necrosis.
Allowing oral diet, too soon after surgery, could have aggravated
the potentially compromised or injured area, leading to the
formation of a gastric fistula.
Surgery, to close the gastric defect, was deemed to be risky,
due to the presence of extensive adhesions in the abdominal
cavity related to recent laparotomies and a dehiscent midline
laparotomy wound draining pus. Surgery, at this point of time,
might cause more fistulations and further injury to organs.
Feeding jejunostomy was also difficult. Even if feeding jejunostomy
alone were done, gastric secretions and saliva would still
leak through the gastric defect leading to no significant clinical
benefit. OTSC system was considered a promising endoscopic
approach for management of post-laparoscopic sleeve gastrectomy
(LSG) leaks in selected patients [6]. The surfaces of the
peritoneal cavity had chronic inflammation with friable granulation
tissue. Hence, satisfactory clipping was not possible,
and the defect was still evident. The defect was too large to
be clipped.
Niti S Mega Esophageal stent was considered to bypass the
gastric leak as it was previously reported to be successful in
the setting of gastric leaks after sleeve gastrectomy, to bypass
the defects in a tubular shaped stomach [7]. Our patient did
not undergo bariatric surgery. The volume of the stomach in
this case was normal/higher than normal. The stomach was not
tubular in shape. The guidewire and the stent had to go in a
tortuous path along the surface of the stomach and hence, the
stent could not be passed beyond the antrum region, leading
to persistent leakage. Due to the risk of migration of the mega
esophageal stent with reintervention, the next endoscopic intervention
was delayed by five days. A through the scope (TTS)
metal stent was chosen, as the scope was inserted through the
already placed Mega stent. The stent could be placed through the scope. The fully covered stent with the flares as wide as the
previously placed stent, was chosen for relatively tight approximation.
Migration rate of these stents is reported to be as high as 30%
[8]. Even with minimal migration, of either the first or second
placed stents, the leak might not have settled or potentially
could recur. This patient did not have migration of stents, likely
due to the placement of Olympus EZ clips at the edges of stents.
Previously, stents were successfully placed from esophagus to
duodenum to bypass the gastric defects in tubular stomach after
bariatric surgery [7]. To our knowledge, this is the first case
of endoscopic gastric bypass by metal stenting, with stent in
stent technique, from esophagus to duodenum to bypass the
defect in the normal volume stomach.
Conclusion
In summary, our report indicates that if 6-7 weeks period of
conservative treatment for gastric fistula has been ineffective
and if peritonitis is minimal and if margins of the large gastric
defect are edematous and necrosed, endoscopic stent placement
is a good choice of treatment. This technique has the advantages
of decreased procedure time and far lesser complications,
reduced hospital time and is effective in the treatment of
gastric fistula. It is possible and necessary to stent from esophagus
to duodenum to bypass the gastric defect, especially if the
margins of the defect are edematous and necrosed, even if the
volume of stomach is normal (and not reduced as in the case of
sleeve gastrectomy).
Acknowledgement
None.
Conflict of Interest
Authors declare no conflict of interest.
REFERENCES
- Aurora AR, Khaitan L, Saber AA (2012) Sleeve gastrectomy and the risk of leak: A systematic analysis of 4,888 patients. Surg Endosc. 26(6):1509-1515.
[Crossref] [Google Scholar] [PubMed]
- DeMaria EJ, Pate V, Warthen M, Winegar DA (2010) Baseline data from american society for metabolic and bariatric surgery-designated bariatric surgery centers of excellence using the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 6(4):347-355.
[Crossref] [Google Scholar] [PubMed]
- Li Z, Bai B, Xie F, Zhao Q (2018) Distal versus total gastrectomy for middle and lower-third gastric cancer: A systematic review and meta-analysis. Int J Surg Lond Engl. 53:163-170.
[Crossref] [Google Scholar] [PubMed]
- McClenathan JH (1991) Gastric perforation as a complication of splenectomy: Report of five cases and review of the literature. Can J Surg J Can Chir. 34(2):175-178.
[Google Scholar] [PubMed]
- Yu J, Zhou CJ, Wang P, Wei SJ, He JS, et al. (2018) Endoscopic titanium clip closure of gastric fistula after splenectomy: A case report. World J Clin Cases. 6(15):1047-52.
[Crossref] [Google Scholar] [PubMed]
- Shoar S, Poliakin L, Khorgami Z, Rubenstein R, El-Matbouly M, et al. (2017) Efficacy and safety of the over-the-scope clip (OTSC) system in the management of leak and fistula after laparoscopic sleeve gastrectomy: A systematic review. Obes Surg. 27(9):2410-2418.
[Crossref] [Google Scholar] [PubMed]
- Klimczak T, Klimczak J, Szewczyk T, Janczak P, Jurałowicz P (2018) Endoscopic treatment of leaks after laparoscopic sleeve gastrectomy using MEGA esophageal covered stents. Surg Endosc. 32(4):2038-2045.
[Crossref] [Google Scholar] [PubMed]
- Shehab H, Abdallah E, Gawdat K, Elattar I (2018) Large bariatric-specific stents and over-the-scope clips in the management of post-bariatric surgery leaks. Obes Surg. 28(1):15-24.
[Crossref] [Google Scholar] [PubMed]
Citation: Moka P, Kumar VL, Reddy SKA, Reddy SA, Krishna AG, et al. (2022) Gastric Leak Treated by Endoscopic Gastric Bypass
with Metal Stent in Stent Technique in Normal Volume Stomach (Outside Bariatric Setting): First Case Report. J Clin Gastroenterol
Hepatol. 6:40.
Copyright: © 2022 Moka P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source
are credited.