Research Article - (2016) Volume 24, Issue 2
Hiroaki Takenaka, MD., FJSIM
Vice President, Takenaka Clinic, Japan
Nobutaro Ban
Professor, Department of General Medicine/Family & Community Medicine, Nagoya University Graduate School of Medicine, Japan
Tomio Suzuki
Professor, Division of General Medicine, Osaka Medical College, Japan
Hideki Tokuyama
Director, Division of Acute Medicine, Komaki Municipal Hospital, Japan
Juichi Sato
Assistant professor, Department of General Medicine/Family & Community Medicine, Nagoya University Graduate School of Medicine, Japan
Corresponding Author:
Hiroaki Takenaka
Takenaka Clinic, 3-16-19 Nippombashi-Higashi, Naniwa ward, OSAKA 556-0006, JAPAN
Tel: +81-6-6632-4707
Fax: +81-6-6632-4707
E-mail: ht69_nnw@aioros.ocn.ne.jp
Background: Previous work on physicians’ family approach has identified as “the Levels of Family Involvement (LFI) model” (e.g., Doherty and Baird). We also investigated frequency of each level on Japanese family physicians and nurses, but we found that they displayed lower levels of involvement than the previous work had suggested. This paper used a qualitative research method to focus on the various family approaches by Japanese general physicians.
Methods: Ten general physicians took part in a focus group discussion about attitudes to the family approach. To establish the trustworthiness of this research, we applied the four standards of credibility, transferability, dependability, and confirmability.
Findings: We found five phases in the perception and practice of the family approach, ranging from the practice of basic clinical skills and a simple recognition of the effect of the family on the patient, to higher stages of practice involving the recognition of the family as a coherent unit. Participants also identified two distinct stages of practice of the family approach: a haphazard or inconsistent approach, and a more systematic family approach.
Conclusions: Application of the family approach in the context of general practice in Japan is mediated through different phases and stages.
Keywords
Family, General Practice Physicians, Focus Groups
List of Abbreviations
FGD: focus group discussion; LFI model: the Levels of Family Involvement model
Introduction
In Japan, approximately 30% of outpatients receiving medical care from university hospitals,1 community hospital diabetic outpatient clinics,2 or community hospital surgical outpatient clinics have family issues;3 furthermore, approximately 45% of outpatients who receive medical care from four Japanese clinics present family issues.4 Thus, we regard family issues as a common problem affecting health.
How do general physicians treat family issues? Doherty and Baird identified five different levels of physician involvement with patients and their families5 (the Levels of Family Involvement (LFI) model), 6 and offer this as a basic model in family medicine. Level 1 involves a minimal emphasis on family, with interactions restricted to those necessary for practical or legal regulations. Level 2 is more collaborative, with the physician giving advice and information to family members and gathering information about the family. Teaching is tailored to fit the learning needs of specific families, but the provider does not intentionally inquire about family stress or emotional reactions. Level 3 involves an engagement with individual and family reactions to stress, empathy with the experiences, feelings, and needs of patients and other family members, and a sharing of knowledge about family stress and family coping. In Level 4, family systems theory is used to offer brief focused interventions to actively explore personal or family issues that affect the care of the patient, and to generate ways to resolve them. Providers offering Level 4 involvement have special training in family assessment and basic family interventions. Level 5 incorporates family therapy to help families cope with strong emotions.
Marvel and Morphew classified 251 videotaped resident– patient interviews according to Doherty and Baird’s five levels.7 In 55% of the interviews, there was no family involvement; 16.7% showed Level 1 involvement, in which the physician discusses family issues, but only with the individual patient, with no family members present. In 24.7% there was Level 2 involvement, but there was almost no Level 3, 4, or 5 involvement, indicating that planned family conferences or emotional support of family members seldom occurred.
Marvel, Schilling, Doherty, and Baird categorized videotaped interviews by ten faculty family physicians during 200 office visits. Most visits involved the lower three levels of physician involvement.8 Discussion of family context occurred in a majority (58.5%) of visits, primarily when another family member was in the room and during preventive care visits. Evidence of higher-level interaction was associated with longer visits, about three minutes more for each additional level.
Recently, Miller referred objective structured clinical exercises (OSCE) in marriage and family therapy9, and Doherty, McDaniel, and Hepworth described how contemporary medical family therapy can contribute to a transformed health care system in four areas: the patient experience of health care, the health of the population, the containment of health care costs, and enhanced practice environments.10
We were interested in investigating and clarifying the kinds of approaches that Japanese general physicians took to familyoriented care. In 1998, we developed a questionnaire survey based on Doherty and Baird’s concept of the role of “skill” in physician involvement with families11 in order to evaluate family approaches by Japanese family physicians. However, we found that physicians displayed lower levels of involvement than previous work had suggested.
In the present study, we utilized a qualitative research method to explore in more depth the methods that Japanese general physicians employ to solve family issues with patients.
Methods
Selection of participants
Due to difficulties in recruiting Japanese family physicians in clinics, we recruited general physicians from the department of General Medicine, Nagoya University Hospital, Japan. Participants were General Medicine specialists, and had clinical experience in community settings. All participants were members of the Japanese Academy of Family Medicine (now the Japan Primary Care Association).
Ten participants took part in the research, from a total of twelve members of the department of General Medicine. Eight participants had five to ten years of experience as physicians. One participant was a professor and one an assistant professor. Nine of the participants were men. Two members of the department could not take part in this research because they were researchers involved in this study. Participants were divided into two groups, depending on their experience and daily working schedule, with six participants in the first discussion group and four in the second.
Ethical considerations
Written informed consent was obtained from all participants. The Institutional Review Board of Nagoya University approved the study protocol.
Conducting the focus group discussion
We considered focus group discussion (FGD) to be a suitable method for this study because our objective was to achieve consensus on Japanese general physicians’ attitudes towards family issues and many Japanese people are not good at talking about their personal opinions and experiences. The FGD is an established method for accessing personal experiences and encouraging people to formulate views through interaction with others. The aim of the FGD was to permit a more indepth exploration of physicians’ approaches and to provide those taking part with a greater sense of personal contact with the project, possibly encouraging them to become personally involved with taking action over the subjects raised in the group discussions.
The research was led by Dr. Takenaka, who works independently at a clinic in Osaka. He attempted to clarify when, where, who, what, whom, why, and how each participant’s approach was done. Two colleagues (Drs. Suzuki and Tokuyama) who had expertise in qualitative research and FDGs, and who did not participate in the FGDs, were active members of the research team.
Discussions were conducted in a private room, videotaped, and transcribed verbatim. All text was then coded.
Data analysis
The initial data analysis was inductive, and no categories were specified in advance. After careful reading and re-reading of transcripts, preliminary coding and categorization of the data were conducted independently by all three analysts, who independently recorded their ideas about emergent themes. The extent to which these categories and emergent theories corresponded was discussed. The initial analysis compared data between the two participant groups, and then compared the data with emergent theories. Using the constant comparative method, the emerging codes and theories were further discussed and refined through meetings of the three analysts until consensus was reached. Coding and categorizing frames were generated to examine the meaning of the contrasting views expressed by physicians.
Trustworthiness of the study
To establish the trustworthiness of this research, we applied the four standards of Guba and Lincoln, 12, 13 namely, credibility, transferability, dependability, and confirmability.
Credibility
The credibility criterion involves establishing that the results of qualitative research are credible or believable from the perspective of the participants. We asked participants to evaluate the results using a member check at the conclusion of the study.
Transferability
Transferability refers to the degree to which the results of qualitative research can be generalized or transferred to other contexts or settings. In this study, we could not precisely analyze transferability because we could not judge whether members of the department of General Medicine, Nagoya University Hospital represent all general physicians in Japan. Therefore, we only confirmed the participant’s place of practice and orientation to general practice.
Dependability
Dependability refers to the stability or consistency of the inquiry processes used over time. In this research, we maintained accuracy by incorporating participants’ data verbatim into the last category of results as accurately as possible.
Confirmability
Confirmability refers to the degree to which the results could be confirmed or corroborated by others. In this research, two of the three analysts were independent of the FGDs. We also checked whether there was any prejudice on the part of the analysts. Moreover, we adopted the discussion of the results from the convention of the 20th Japanese Academy of Family Medicine for external inspection.
Results
The themes presented here emerged from the FGDs, and are illustrated by quotes from participants.
The first FGD was held on July 15, 2002 and lasted for 90 minutes. The second FGD was held on November 3, 2002 and lasted for 70 minutes.
Differences in approach: Phases and Stages (Figure 1)
“I imagine that the family approach is carried out in a stepwise method. The phases are changeable and determined by the condition and context of the patient and family.” (F-48)
Phase 1 referred to the basic clinical skills for all doctors involved in the family approach, including “Taking a family history” (X-2), “Providing medical information to the family” (M-37), and “Explaining the medical conditions of the patient to their family. It contains the prognosis and what happens to the patient.” (H-43)
Phase 2 referred to considering the family’s effect on the patient; this is thought to be a core skill for general physicians. Practically, it involves meeting the family and obtaining their cooperation.
“Considering the influence of the stance of the family on the patient.” (A-8)
Phase 3 referred to considering the effect of the patient’s illness on the family.
“One of the roles of family physicians is to treat the effects of the patient’s disease on the family.” (A-8)
“When a patient becomes ill, their family experiences various problems. This phase focuses on aspects of partner care, such as alcoholism, sexually transmitted diseases, anticipatory guidance, empathetic family care, and other factors.” (P-37)
Phase 4 involved considering the family as a unit. This means considering familial illnesses and influencing family dynamics through an individual approach.
“It means comprehensive family health management through patient care.” (T-19)
“When patients need to improve their lifestyle, it is very difficult for their family to, for instance, make a different special meal for the patient. Therefore, the family should make the patient’s special meals their common meal, not only for the patient but to help maintain everyone’s health.” (D-7)
Phase 5 exemplified a more specialized approach with advanced skills, theory, and techniques applied by specially trained physicians.
“It’s at the specialist’s level.” (A-9)
“Issues that affect a patient’s daily life are probably beyond the control of family physicians.” (A-11)
“I agree with you, but I feel that there are no specialists. It’s a severe problem.” (F-20)
In the FGD, the interviewer felt that these results were similar to the levels of physician involvement with families identified by Doherty and Baird.5 However, some aspects of their findings did not correspond with our results. In the present study, the interviewer discussed this theme with the participants. After discussion, we identified the key theme of the “systematic approach.”
“I have not yet carried out a systematic family approach.” (M-26)
This theme seemed to refer to an independent concept of the levels through which physicians approach the family. Therefore, we referred to this concept as a “stage”; another axis by which we can understand the family approach of general physicians. The identity of this concept was confirmed through the member checking.
Stage 1 indicated a haphazard or inconsistent family approach. In this stage, the physician allowed issues to go unheeded, approaches situations unconsciously, and might even fail to approach the family.
“Anyway, I was seized with a need to do something. So I asked the family to come.” (H-63)
“I did it on trial and error, not systematically.” (H-63)
Stage 2 represented a more systematic family approach. In this phase, physicians have their own style and their approach is more consistent.
“[This refers to] utilizing something in a more systematic way.” (H-63)
“We can take a more active and systematic approach on demand.” (M-48)
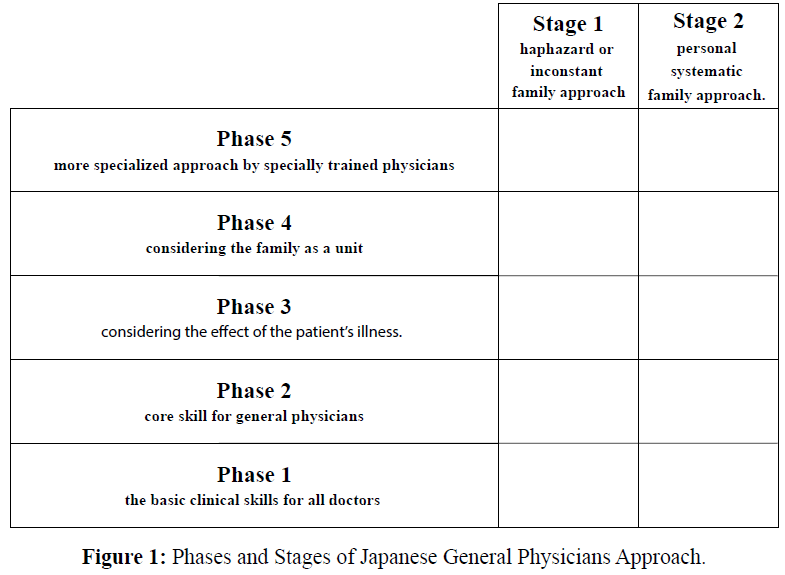
Figure 1: Phases and Stages of Japanese General Physicians Approach.
Differences in perceived role of general physicians
The analysis showed that participants sometimes defined the role of general physician quite differently. The main focus of inquiry when we began the FGDs was “What is the family approach used by Japanese general physicians?” However, participants differed in how they defined the role of the physician. One participant said, “We have a responsibility for not only the patient but also the health of the whole family if we take the stance of a family physician,” (F-10) while another said, “I am just a general physician, and do not assume the role of family physician.” (E-9)
Differences of clinical setting (Figure 2, 3)
Interestingly, the same participant might change their approach depending on the clinical setting. In relation to this theme, the FGD included a discussion of differences between university hospitals and clinics.
“At a university, I separated medical care and life. The family approach in a university is that the doctor only calls the family.” (B-31)
“We have little relationship with the family, even at hospitals with comparatively easy access.” (TX-3)
In relation to practicing in a clinic, participants made the following points:
“It is an old familiar relationship between physician and family, which has developed through time. We can regard it as a history of their relationship.” (H-2)
One participant, however, highlighted a much broader distinction in modes of practice:
“I think there is a difference between urban and rural settings. I am not sure that it is a difference between university hospitals and clinics.” (Y-3)
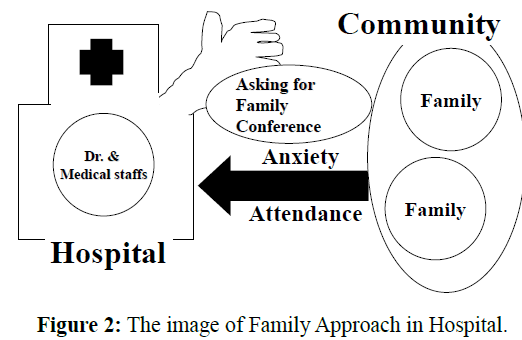
Figure 2: The image of Family Approach in Hospital.
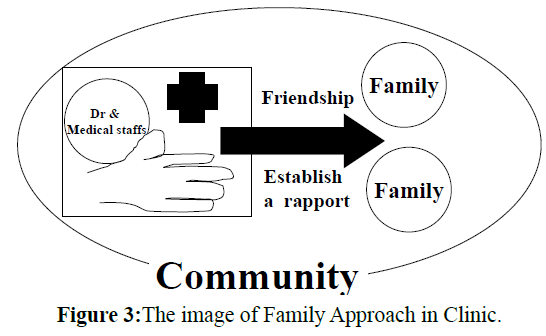
Figure 3: The image of Family Approach in Clinic.
Education in relation to the family approach
There was general consensus that the family approach as a methodology was not taught. This made it difficult to practice, especially considering the lack of formal training in the methodology.
“Individual care is regarded as more important in medical care. Therefore, I think that the family approach should be taught as one medical method.” (P-62)
“The family approach is not often carried out, and the methodology is not taught either. I think that the family approach has enough useful elements. I think that the methodology is still in its infancy, but it contains a lot of useful domains.” (P-66)
Discussion
Ultimately, we were unable to reach consensus about the type of family approach taken by Japanese general physicians, because Japanese general practice encompasses various clinical settings. In addition, individual physicians practice different levels of the family approach.
In some ways, our results resembled the levels of physician involvement with families reported by Doherty and Baird.5 However, in our study, physicians with high-level skills did not take a high-level approach to all patients and families. The appropriate approach may be Level 3 if a patient comes to a physician for care of a common cold. However, if a patient has a complicated family issue, a Level 5 approach may be needed. In other words, it is not appropriate to assume that Level 3 is necessarily inferior to Level 5. For this reason, we have used the term “phase” rather than “level” to describe the type of approach.
Our analyses also identified a second explanatory axis, which we designated “stage.” This was not reflected in the Doherty and Baird study.5 We identified two such stages of a family approach: one embodied an inconsistent approach to family issues, and the other represented a more systematic approach. Stage 2 appeared to be divided into three or more stages, which we examined in more depth through the process of member checking. We named these three substages 2.1, 2.2, and 2.3 (Figure 4).
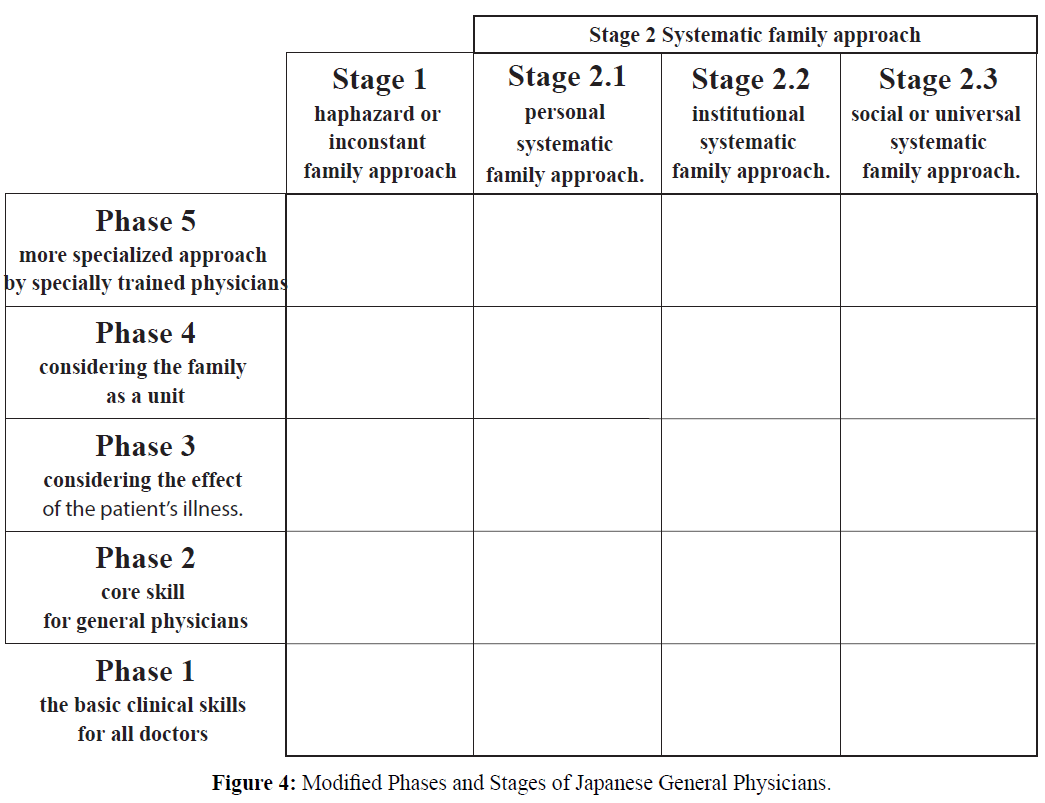
Figure 4: Modified Phases and Stages of Japanese General Physicians
Stage 2.1 represents a personal systematic family approach; physicians have their own style and their approach is thus consistent. Stage 2.2 is the institutional systematic family approach. In this stage, everyone belonging to an institution employs the same family approaches and screens cases thoroughly. Stage 2.3 is the social or universal systematic family approach. In this stage, the skills employed are regarded as exemplifying a more common sense approach. Although subdivision of these stages is valuable at a societal and/or training-program level, it is perhaps not needed for individual training or learning. It is enough to determine whether a physician’s approach is systematic or not at the personal level.
Our analyses showed that physicians oriented to general internal medicine and diagnosis dealt with family dynamics in a more passive way, and tended to adopt a Phase 2 approach, while physicians oriented to family practice and care were more positive in considering family dynamics an essential component of their medical practice and regarded a Phase 3 approach as their standard. Development of training programs targeting both types of general physician may be necessary in Japan, because family physicians and general physicians (hospitalists) tend to belong to the same society and take the same training courses.
At the present time, the family approach in Japan appears to overemphasize family therapy. However, it is difficult for family physicians to find the time to perform family therapy. We recommend more frequent use of personal interviews employing family dynamics, which can help create “ripple effects” that lead to more substantial changes.
There is an increasing need for training in the family approach for Japanese physicians. One solution would be more use of simulated family interactions to aid learning in family dynamics, together with a clarification of outcomes for standardized training. We intend to develop the family approach training workshops we provide for primary care staff using some of the techniques and aids discussed here.
Our study had several potential biases and limitations. One potential problem was the influence of the more senior colleagues on the FGDs. Their input tended to be too dominant, leading to a potential influence on participants of the existing medical hierarchy. The chairman (Dr. Takenaka) was careful in this regard in dealing with the participants.
Another limitation is the loss in meaning in translating our findings into English from Japanese, which may lose the subtle nuances of the participants' meanings. Furthermore, it has resulted in a substantial gap in between our publication and the data collection period, which may mean the results are not applicable currently.
One common limitation of FGDs concerns the validity of the subliminal categories generated. In the present study, we found that these could not be analyzed by member checking, and so it was difficult to ascertain their validity. The reliability of participants’ impromptu opinions was also an area of concern. These questions should be addressed in future qualitative research in this area.
With regards to sample size, there are no specific rules when determining an appropriate sample size in qualitative research. Qualitative analyses typically require a smaller sample size the quantitative analyses. For phenomenological studies, Creswell recommends five to 25 14 and Morse suggests at least six 15.
There is much discussion in Japanese healthcare of a “global standard” for health practice. However, our findings show that the family approach in general practice in Japan was subject to varying definitions, and it was conceptualized differently in contrasting clinical and educational settings. Further research is needed to examine how general physicians in other cultural contexts understand and practice the family approach.
Conclusions
Application of the family approach in the context of general practice in Japan is mediated through different phases and stages. The implementation of the approach depends on various clinical settings and educational levels. We suggest that general physicians’ understanding of the family approach is heavily dependent on the social and cultural context.
Acknowledgement
We appreciate the work of everyone who supported us, especially our colleagues at the department of General Medicine, Nagoya University Hospital, Japan who gave advice on this study.
Competing Ans Coflicting Interests
There are any non-financial competing interests to declare in relation to this manuscript. Therefore our submission needs much more time.
Authors' Contributions
Dr Takenaka is the corresponding author. He wrote this manuscript and researched data, contributed to written informed consent, and discussion.
Dr Ban have been involved in drafting the manuscript and revising it critically for important intellectual content and have given final approval of the version to be published.
Drs. Suzuki and Dr Tokuyama have made substantial contributions to acquisition of data and analysis and interpretation of data.
Dr Sato have made substantial contributions to conception and design, especially ethical consideration.