- (2011) Volume 12, Issue 2
Vishal Gupta, Sunil Kumar, Pankaj Kumar, Abhijit Chandra*
Department of Surgical Gastroenterology, Chhatrapati Shahuji Maharaj Medical University. Chowk, Lucknow, Uttar Pradesh. India
Received December 15th, 2010 Accepted February 1st, 2011
Context Visceral artery pseudoaneurysms are uncommon. They most commonly affect the splenic artery and are secondary to chronic pancreatitis. Giant pseudoaneurysms (5 cm or larger in size) are rare and, until now, only 19 cases have been reported. Case report A 47-year-old chronic alcoholic and diabetic male presented with upper abdominal pain of 1-month duration without any other significant complaint. Computed tomography was performed which revealed features of chronic pancreatitis along with a splenic artery pseudoaneurysm measuring 7x4 cm in size. As the disease was confined to the body and tail of the pancreas, the patient underwent a distal pancreatectomy and splenectomy along with resection of the pseudoaneurysm with an uneventful postoperative course. Conclusion Splenic artery pseudoaneurysms, especially the giant variety, are uncommon. As they are most commonly secondary to chronic pancreatitis, they are better managed surgically which resolves the pseudoaneurysm as well as its underlying cause (i.e. chronic pancreatitis).
Pancreatitis, Chronic; Splenectomy; Aneurysm, False
Visceral artery aneurysms are uncommon and pseudoaneurysms are rare entities. The splenic artery is the most commonly affected artery [1]. Goldberg et al. [2] found only 160 cases of splenic artery pseudoaneurysm in the literature which were reported in the last 43 years. The Mayo clinic experience revealed only 10 cases over a period of 18 years [1]. Giant pseudoaneurysms, defined as pseudoaneurysms equal to, or greater than, 5 cm in size, are rare. Only 19 cases have been reported until now. We herein describe the case of a giant pseudoaneurysm of the splenic artery in a patient who presented with abdominal pain without bleeding.
A 47-year-old male patient presented to our out-patient department with a 1-month history of non-radiating epigastric abdominal pain, moderate to severe in intensity occasionally requiring injectable analgesics. There was a history of occasional vomiting. He had been an alcoholic for the past 15 years. Diabetes had been detected 6 months previously and was controlled with an oral hypoglycemic. There was no history of hematemesis, melena, fever, jaundice, altered bowel habits, anorexia or weight loss. He had undergone an open cholecystectomy 3 years previously for symptomatic gallstones. Physical examination was non-contributory. The patient was initially evaluated elsewhere with abdominal ultrasound which revealed a multilayered lesion with a peripheral anechoic area contiguous with the splenic artery and another cystic lesion (5.5x4 cm) close to the anterior abdominal wall. The patient was admitted to our center and underwent further evaluation.
A hematological work-up, including hemoglobin and liver function tests, was normal. A contrast enhanced computed tomography scan (Figures 1 and 2) revealed features of chronic pancreatitis with multiple foci of calcifications in the pancreatic duct and parenchyma involving the body and tail. The pancreatic duct was not significantly dilated. There was a large pseudoaneurysm measuring 7x4 cm in size in the splenic artery. In addition, there was a pseudocyst measuring 6x4 cm in size in the omentum, separate from the pancreas.
The patient underwent an exploratory laparotomy. The pancreas was firm and there was a large pulsating pseudocyst in the body of the pancreas having a thin wall at places where an intraluminal clot could be seen (Figure 3). It was densely adherent to the stomach and the retroperitoneum. Another pseudocyst was also located in the greater omentum separate from the pancreas. The lesser sac was entered by dividing the gastrocolic omentum and the short gastric vessels. The stomach was separated from the pseudoaneurysm and the pancreas by careful dissection. Proximal vascular control of the splenic artery was achieved near its origin. A distal pancreatectomy and splenectomy were then performed in an antegrade manner (Figure 4). The omental pancreatic pseudocyst was also resected. The postoperative period was uneventful and the patient was discharged on the 7th postoperative day.
Visceral artery pseudoaneurysms are uncommon. The splenic artery is the most commonly affected visceral artery [1]. They usually develop secondary to pancreatic diseases. They develop more commonly in chronic pancreatitis (46%) than in acute pancreatitis (6%) [1]. Our patient developed a splenic artery pseudoaneurysm secondary to chronic pancreatitis. The mechanisms of the formation of pseudoaneurysms in pancreatitis include inflammation with enzymatic digestion of the pancreatic or peripancreatic artery, visceral artery erosion by pseudocysts and pseudocyst erosion into the bowel wall and intramural artery [3]. Abdominal trauma is the second most common cause. Damage to the intima and elastic lamina due to rapid deceleration may lead to the formation of such a pseudoaneurysm [4]. Other causes described are peptic ulcer disease and iatrogenic causes (e.g. prior abdominal surgery or endovascular interventions) [1, 2].
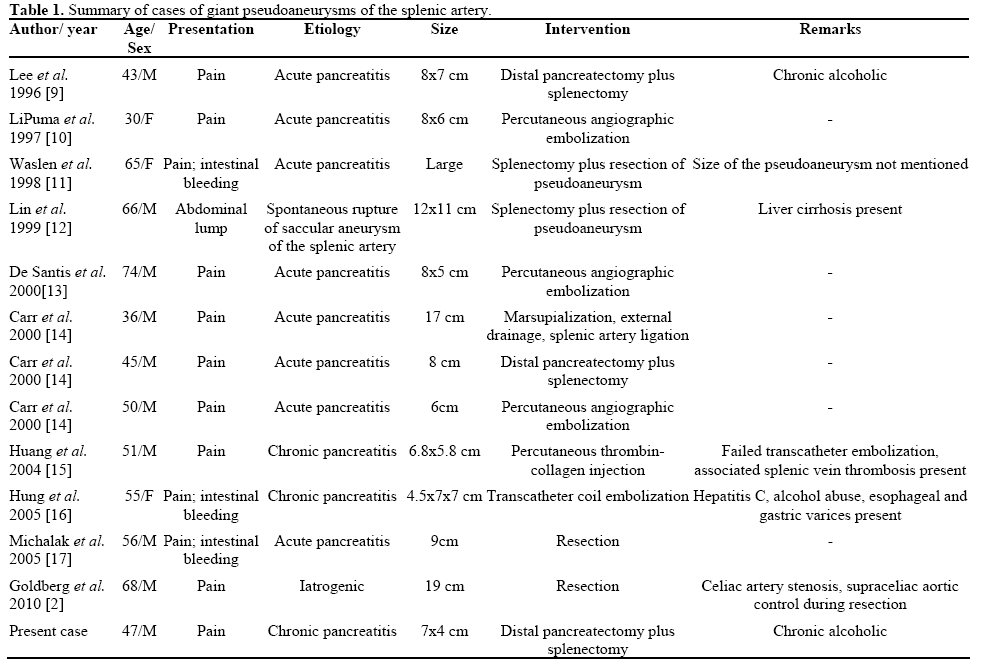
Most of theses pseudoaneurysms are symptomatic at presentation; however, 2.5% of cases have been incidental [1]. They most commonly present with abdominal pain (as in our case) or with bleeding into the gut which may be catastrophic at times. Large or giant pseudoaneurysms may also present with an abdominal lump (Table 1).
Diagnosis is usually made from computed tomography (including CT angiography) or transcatheter angiography. They can also be detected on color Doppler or MR angiography. Transcatheter angiography is considered the gold standard and also has therapeutic potential.
A giant pseudoaneurysm is defined as a pseudoaneurysm equal to, or greater than, 5 cm in size. In the literature, size has ranged from 5-18 cm [1, 2]. Only 19 cases of giant pseudoaneurysms have been reported. Most of these (n=15) have been seen in association with pancreatic diseases [1] (Table 1). Erosion of the splenic artery by an enlarging pseudocyst due to enzymatic digestion and, thus, conversion of the pseudocyst into a pseudoaneurysm can explain the formation of a giant pseudoaneurysm. The remaining 4 cases were secondary to iatrogenic causes: e.g., splenectomy in 2 cases, cystogastrostomy in one and a prior attempt at repairing a splenic artery aneurysm in the last reported case [2].
All splenic artery pseudoaneurysms should be treated when detected as size is not a determinant of future rupture. This is more relevant in patients with chronic pancreatitis as it is an ongoing inflammatory process. A review of the literature suggests that these giant pseudoaneurysms have been managed by both surgical and non-surgical means (Table 1). Different methods of treatment have been trans-angiographic embolization (n=8), distal pancreatectomy/splenectomy (n=7), thrombin injection (n=2), pancreatectomy (n=1) and resection of pseudoaneurysm only (n=1) [2]. However, a pseudoaneurysm associated with a pseudocyst should be treated surgically as the literature indicated that transcatheter embolization has a higher failure rate (20%) as a primary treatment in these patients than in those without pseudocysts (13%) [1]. Hsu et al. [3] have also reported a high (66.7%) rebleeding rate after angiographic embolization. There are recent reports of successful treatment by endovascular stent graft occlusion of these pseudoaneurysms [5]. A pseudoaneurysm related to pseudocyst formation is best treated with surgical excision [1, 6, 7, 8]. Different surgical options exist including splenectomy with or without distal pancreatectomy, ligation of the splenic artery with resection of the pseudoaneurysm and trans-cystic ligation of the bleeding vessel with internal or external drainage of the pseudocyst. Splenectomy, with or without distal pancreatectomy, is a procedure with no reported failure over long periods of time [1]. Distal pancreatectomy and splenectomy should be employed to treat bleeding pseudoaneurysms located in the distal body and tail of the pancreas. Pancreatic resection is the only way to treat these pseudoaneurysms together with the underlying pathologic process in the pancreas which is the primary cause of the pseudoaneurysm. This may be curative in cases where chronic pancreatitis changes are confined to the body and tail of the pancreas, as in our case. However, surgical treatment may not be straightforward especially, in cases of giant pseudoaneurysm.
The authors have no potential conflicts of interest