- (2004) Volume 5, Issue 4
Miguel Echenique-Elizondo1, Ana Tuneu Valls2, José Luis Elorza Orúe2, Ignacio Martinez de Lizarduy3, Javier Ibáñez Aguirre4
1Department of Surgery, Basque Country University; 2Department of Dermatology, Donostia Hospital; 3Department of Dermatology Hospital de Basurto; 4Department of Surgery, Zumárraga Hospital. San Sebastián, Spain
Received: 06 February 2004 Accepted: 30 March 2004
Context Glucagonoma syndrome may present either associated with a pancreatic neoplasm which secretes glucagon or as a pseudoglucagonoma associated with other diseases. It is extremely infrequent but well-known with a current prevalence estimated at 1/20,000,000. Design A retrospective review of glucagonoma and pseudoglucagonoma cases observed between January 1998 and December 2003 in three hospitals. Patients: Five cases: 3 with a demonstrable glucagon-secreting tumor and 2 cases without an associated neoplasm. Main outcome measures Age, sex, initial diagnosis, associated symptoms, and pathology were analyzed as were procedures employed in diagnosis, imaging studies, laboratory data, surgery and follow-up. Results Hyperglycemia and elevated plasma glucagon levels were found in all cases. In 3 cases, hypo-aminoacidemia and a descrease in fatty acids were found . No changes of zinc levels were observed. Abdominal ultrasound studies were of no value except in evaluating pancreatitis. A CT-scan was conclusive when a pancreatic neoplasm existed and 3 patients were operated on a curative basis. Discussion Necrolytic migratory erythema was the key diagnosis in all cases. Surgery was intended to be curative. The follow-up was of 8, 37 and 57 months in the cases of true glucagonoma syndrome. Conclusions A real prevalence of glucagonoma syndrome could be greater than currently estimated. In our series, it was 13.5/20,000,000. Pseudoglucagonoma syndrome remains a rarity.
https://sporbahisleri.livejournal.com https://wakelet.com/@SporBahisleri67459 https://theomnibuzz.com/author/sporbahisleri/ https://lessons.drawspace.com/profile/322207/sporbahisleri/workflow https://writeupcafe.com/profile/sporbahisleri/ http://www.pearltrees.com/sporbahisleri https://pharmahub.org/members/26874/blog https://www.zupyak.com/u/Spor-Bahisleri/ https://www.metroflog.co/sporbahisleri https://www.fuzia.com/fz/spor-bahisleri https://tr.pinterest.com/sporbahislerim/ https://my.getjealous.com/sporbahisleri https://sporbahisleri.contently.com https://hubpages.com/@sporbahisleri https://www.tumblr.com/sporbahisleri https://hub.docker.com/u/sporbahislerim https://betsiteleri.blogfree.net https://betsiteleri.amebaownd.com https://sporbahisleri.pixnet.net/blog https://betsiteleri.seesaa.net https://betsiteleri.threadless.com https://betsiteleri.neocities.org https://bahissiteleri.localinfo.jp https://betsiteleri.shopinfo.jp https://teletype.in/@betsiteleri https://ubl.xml.org/users/sporbahisleri https://betsiteleri.educatorpages.com https://betsiteleri.onlc.fr https://sporbahisleri.gumroad.com
Endocrine Gland Neoplasms; Erythema; Glucagonoma; Pancreatic Neoplasms
DTPA: diethylenetriaminepentaacetic acid; MOFS: multiorgan failure syndrome; NME: necrolythic migratory erythema; PET: positron emission tomography
First described by Becker et al. in 1942 [1], glucagonoma syndrome is a very infrequent, although well-known, disease. It is characterized by the existence of a glucagonssecreting neoplasm associated with hyperglucagonemia, necrolytic migratory erythema (NME), diabetes mellitus, hypoaminoacidemia, cheilitis, normocytic anemia, vein thrombosis, loss of weight and neuropsychiatric manifestations [2]. The existence of NME used to be considered pathognomonic. Pseudoglucagonoma syndrome refers to the existence of NME in the absence of a neoplasm which secretes glucagon. Slightly more than 300 cases of glucagonoma have been published so far. Its annual incidence has been estimated at 1/20,000,000. It is being described more frequently, and the real prevalence may be greater than estimated [3]. Pseudoglucagonoma syndrome has been described in an even smaller group of patients although data on its real incidence is not conclusive.
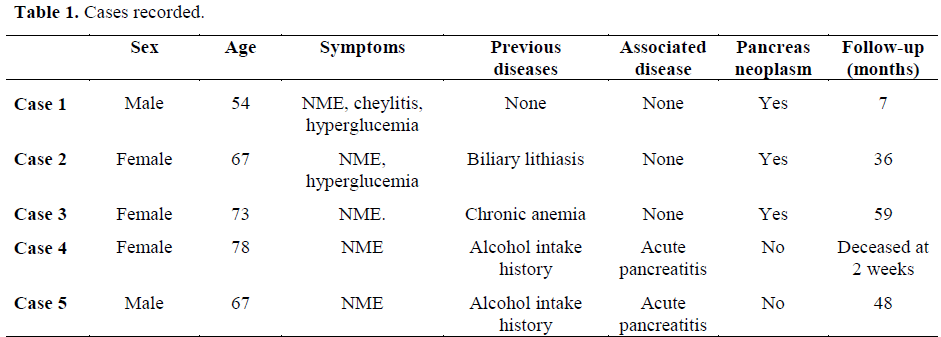
A retrospective review of the cases of glucagonoma and pseudoglucagonoma registered in a sanitary area covering a population of 950,000 persons has been done. From January 1998 to December 2003, 5 cases were treated for glucagonoma syndrome: 3 with a demonstrable pancreatic neoplasm (true glucagonoma syndrome) and 2 cases without a pancreatic neoplasm (pseudoglucagonoma syndrome). We collected the available data on a retrospective basis in each case, including age, sex, first diagnosis and associated symptoms, associated diseases observed, diagnostic procedure, imaging studies, laboratory data, therapeutic procedures employed, surgery and follow-up (Table 1).
No approval by an ethical committee was obtained due to the retrospective nature of the study.
Frequencies were used as descriptive statistics.
Of the 5 cases studied, 3 were males (60%) and 2 were females (40%). The main clinical manifestation at the moment of diagnosis was the existence of an NME in all of them (Figure 1). Glossitis and cheilitis were observed in 3 cases (Figure 2). In 2 cases, confirmation of NME was done by skin biopsy.
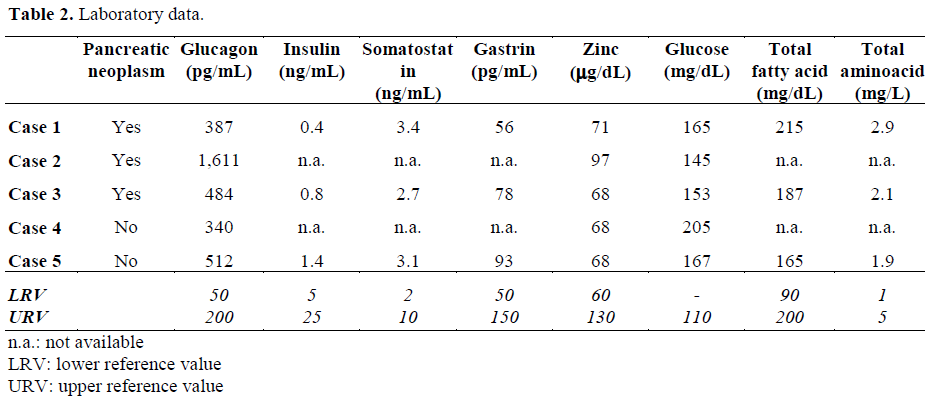
Laboratory data showed an elevation of the plasma glucose in all cases (Table 2). It was more evident in true glucagonoma than in pseudoglucagonoma and was associated with the elevation of plasma glucagon levels. In 3 cases, hypoaminoacidemia was present together with a descrease in free fatty acid levels. No alteration of plasma zinc levels was observed.
Abdominal ultrasound did not offer conclusive results, except in the two cases of pancreatitis, and the CT scan demonstrated a pancreatic neoplasm in 3 cases, situated in the tail, the body/tail, and the body (Figure 3a, 3b, 3c, respectively). An 111I- TPA- (diethylenetriaminepentaacetic acid)-Nterminal D-fenil-alanine octreotide enhanced radio nuclide scan was not done preoperatively.
The 3 patients presenting with pancreatic neoplasms were operated on and the tumor was resectable in all three cases (Figure 4), through a distal pancreatectomy associated with a splenectomy. No regional disease could be demonstrated on gross and pathology studies (Figure 5). A cutaneous rash cleared up between 7 and 15 days after surgery. The follow-up was 8, 37 and 57 months and the patients are disease-free so far. An 111I-DTPA-N-terminal D-fenil-alanine octreotide enhanced radio nuclide scan was performed postoperatively in two patients without evidence of disease spread.
The two cases of pseudo-glucagonoma had a history of alcohol dependence and previous episodes of mild acute pancreatitis. One of these patients died from multiorgan failure syndrome (MOFS) as a result of severe acute pancreatitis after two weeks from admission and the other remained free of symptoms 49 months later. This latter patient had a skin rash cleared up by the 10th day, he had not further episodes of pancreatitis, but we have not been able to show tumor growth in successive controls.
Glucagonoma syndrome is a paraneoplastic phenomenon characterized by the existence of a glucagons-secreting neoplasm associated with hyperglucagonemia, NME, diabetes mellitus, hypo-aminoacidemia, cheilitis, normocytic anemia, vein thrombosis, loss of weight and neuropsychiatric manifestations [2]. The existence of these symptoms, hyperglycemia and a demonstrable pancreatic neoplasm are useful in establishing a diagnosis [4, 5]. Glucagon is responsible for the clinical picture, and the existence of hypoaminoacidemia, hyperglycemia and lipolisis seem to be responsible for the skin changes, generally described as associated with zinc deficiency and favored by the existence of a previous alteration of the liver function. Patients do not generally present with specific manifestations, such as weight loss, diabetes, diarrhea, and stomatitis [6].
Cutaneous eruption which may go undiagnosed for years before a correct diagnosis is made is not infrequent. NME can be found in any part of the body being most frequently located at the perineum, buttocks, inguinal area, lower abdomen and extremities, namely in areas holding greater pressure and friction. A rash appears and disappears in a 10 day cycle and cure with residual skin hyperpigmentation. Other associated changes may include atrophic glossitis, cheilitis, and inflammation of oral mucosa [7].
Males and females are affected similarly, with the sixth and seventh decades of the life being those of greater frequency of presentation. Although the majority of glucagonomas seem to be sporadic, they can occur in the course of multiple endocrine neoplasm syndromes, and insulin, gastrin, VIP and somatostatin must be evaluated. A glucose tolerance test can help in the delineation of the degree of the alimentary profile in relationship to the secretion of insulin and the functional excess of glucagon. Amino acids, zinc and the essential fatty acids must be evaluated because NME can respond to a correction of its alterations. Nevertheless, high levels of glucagon do not necessarily produce diabetes mellitus, NME [8] or hypoaminoacidemia [9]. Since the liver is responsible for the metabolization of glucagon, cirrhosis can prolong the active period of glucagon expression and contribute to the abnormally high levels in serum. NME with normal levels of glucagon has been described in the sprue and in pancreatitis as well as similar alterations of the skin which can be found in cystic fibrosis [10].
In the presence of NME, the epidermis shows moderate acanthosis, spongiosis, parakeratosis and loss of the granular layer. Dyskeratosis and necrosis in the superficial layers give rise to a characteristic separation of the deepest epidermis [11]. Quick resolutions of NME have been described after surgical resection of a glucagonoma [12] or with a powerful glucagon secretion-inhibiting drug, as happens with somatostatin. Supplements of zinc and the essential fatty acids have been shown to be capable of resolving NME in some patients [13, 14]. The catabolic effects of glucagon at the protein level and fat metabolism are the main factors leading to weight loss, cachexia and anemia [15, 16].
Glucagonomas are slow-growing neoplasms with non-specific symptoms at the beginning. At least 50% of the described cases were metastatic at the moment of the diagnosis and have therefore had a bad outcome. A fiveyear survival rate cannot be estimated because of its rarity, but a study has shown that tumorrelated death occurred in 9 out of 21 patients at an average of 4.9 years after diagnosis, and the remaining 12 patients were alive after an average interval of 3.7 years [17]. The mortality rate associated with the pseudoglucagonoma syndrome is that of the underlying disease. Some cases secondary to celiac sprue are completely cured by diet modification. Others, such as those observed in liver cirrhosis or other neoplasms, generally have a poor prognosis.
Localization of the primary pancreatic neoplasm and spread evaluation is carried out nowadays fundamentally by CT scan, MRI and ultrasound. Positron emission tomography (PET) has recently been employed with positive results [18]. An abdominal angiogram is adequate for locating the primary neoplasm in complex situations because glucagonomas tend to be hypervascularized. The actual identification of the degree of tumor spread is very important because therapeutic interventions may change when metastatic disease exists. Glucagonomas contain somatostatin receptors in more than 80% of cases. Nevertheless, sensitivity and specificity of imaging with somatostatin analogue (111I-DTPA-N-terminal D-fenil-alanine octeotride) has been successfully employed in demonstrating a primary neoplasm and its spread when this exists. It may be utilized as a therapeutic complement due to emission of beta radiation of the marker [19].
These tumors usually present in the tail of the pancreas. They are generally solid, circumscribed and well vascularized [20]. Immunostaining can be positive for glucagon, although the intensity of the dye cannot be correlated with glucagon serum levels. If this method does not detect the production of glucagon, in situ hybridization of mRNA can be conclusive. Electron microscopy may show neurosecretory bodies and a complex endoplasmic reticulum.
Chemotherapy is not effective in the management of glucagonomas probably because the tumor is indolent by nature [21]. Not a single case cured in this way has been recorded [22], but some cases of induced regression and remission of symptomatic NME have been reported. Streptozocin, associated or not with 5-fluorouracil, has offered some response. Dacarbazin has produced remission of NME, reducing levels of titred glucagon. In some patients, octreotide, lanreotide and a long duration analogue of somatostatin have produced rapid clearing of NME, although they have been shown to be ineffective in the pseudoglucagonoma syndrome, where a correct management of the underlying illness often resolves the NME [23, 24, 25].
Surgical resection is the only potentially curative procedure [26]. It is possible when the tumor is still localized. Laparoscopy has recently been employed in a few selected cases [27]. Because tumor growth is slow and tends to be capsulated, resection can be carried out successfully in the early stages [28]. Since NME is the main symptom of the glucagonoma syndrome, palliative therapies can be attempted to diminish skin rash [29]. Tumor mass reduction has been seen to be effective and efficient in healing the cutaneous symptoms [30]; embolization of the liver may also induce selective necrosis of metastasis when present. At present, a liver transplant associated with a pancreatectomy can be considered in the case of rare liver involvement.