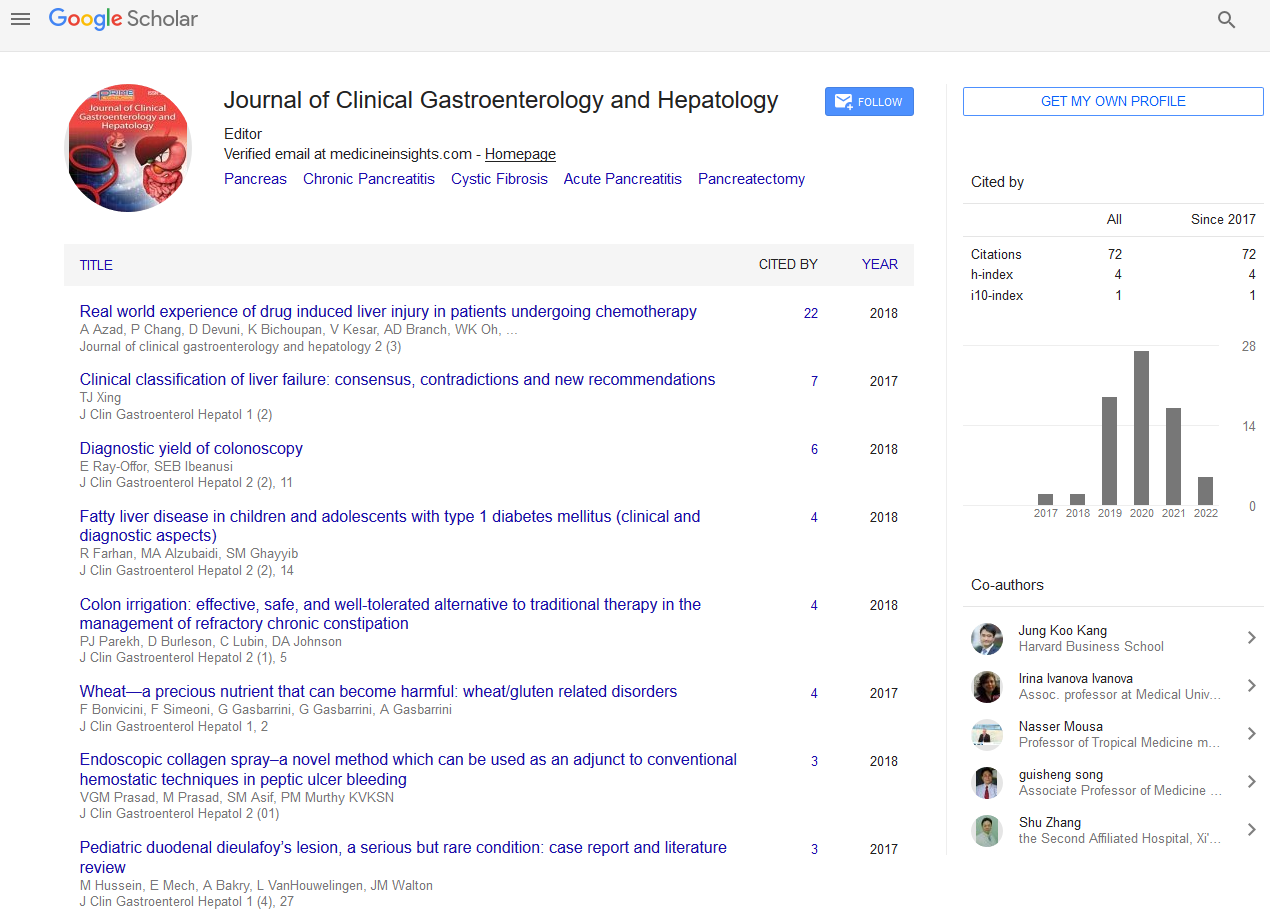
Review Article - (2024) Volume 8, Issue 4
Gut Microbiome and Immune Responses in Gastrointestinal Diseases
Byung Soo Yoo1*,
Benjamin L. Robinson1,
Ana Vilela2,
Alsiddig Elmahdi3,
Kevin Houston3 and
David A. Johnson4
1Department of Gastroenterology and Medicine, Advocate Health Wake Forest, Charlotte, North Carolina, United States of America
2Department of Medicine, Eastern Virginia Medical School, Norfolk, Virginia, United States of America
3Department of Medicine, Virginia Commonwealth University, Richmond, Virginia, United States of America
4Department of Gastroenterology and Medicine, Eastern Virginia Medical School, Norfolk, Virginia, United States of America
*Correspondence:
Byung Soo Yoo, Department of Gastroenterology and Medicine, Advocate Health Wake Forest, Charlotte, North Carolina,
United States of America,
Email:
Received: 31-Jul-2024, Manuscript No. IPJCGH-24-21046;
Editor assigned: 05-Aug-2024, Pre QC No. IPJCGH-24-21046 (PQ);
Reviewed: 19-Aug-2024, QC No. IPJCGH-24-21046;
Revised: 26-Aug-2024, Manuscript No. IPJCGH-24-21046 (R);
Published:
04-Sep-2024, DOI: 10.36648/2575-7733.8.4.32
Abstract
Highlighting the expanding research on the Gastrointestinal (GI) microbiome, this review explores its
pivotal role in disease pathogenesis, specifically, gastroesophageal reflux disease, barrett’s esophagus,
eosinophilic esophagitis, inflammatory bowel disease, colon cancer and hepatobiliary disease. The
immune system acts as a crucial bridge, connecting the gut microbiome to these GI disorders. Studies
demonstrate that microbial dysbiosis triggers immune responses, initiating a pro-inflammatory
cytokine cascade. This reciprocal inflammatory interplay between the host’s immune system and GI
microbiome contributes to disease progression, emphasizing significant potential for diagnostic and
therapeutic implications.
Keywords
Gut microbiome; Immune system; Gastrointestinal disorders; Gastroesophageal reflux
disease; Barrett’s esophagus; Eosinophilic esophagitis; Esophageal cancer; Inflammatory bowel
disease; Colon cancer; Hepatobiliary disease
Introduction
The dynamic interplay between the Gastrointestinal (GI)
microbiome and the host immune system constitutes a
vibrant field of research. Delving into the intricacies of this
relationship has significantly advanced our comprehension of
GI diseases, shedding light on the delicate equilibrium within
the immune system and its intricate interactions with the GI
microbiota. The gut microbiota, composed of bacteria, viruses,
fungi and archaea, inhabits various environments, including
the respiratory tract, GI tract and skin [1,2]. This intricate
collection of microorganisms, termed microbiota, along with its genomic components from the GI tract, referred to as the
microbiome, plays a pivotal role in health and disease [3].
Studies have revealed that the human gut microbiome
encompasses a diverse array of species, numbering up to
1500, with Firmicutes spp. and Bacteroidetes spp. constituting
a substantial 92% of this community [4,5]. The normal
composition of the microbiome is influenced by a myriad of
factors, chiefly genetics and environmental cues. Maintaining
a healthy equilibrium between the microbiome and the
immune system is crucial for an individual’s well-being.
However, disruptions in this balance, leading to microbial dysbiosis, have been associated with prevalent diseases such
as obesity, type 2 diabetes mellitus, hypertension and various
GI disorders.
This intricate relationship extends its implications to diseases
like Gastroesophageal Reflux Disease (GERD), Barrett’s
Esophagus (BE), Eosinophilic Esophagitis (EoE), Inflammatory
Bowel Disease (IBD) and certain GI cancers. The gut
microbiome’s production of metabolites, its interaction with
the host’s immune system and the elicitation of immune
responses through inflammatory signaling are central
mechanisms underpinning the pathophysiology of these
diseases [6]. Additionally, the diet and exogenous factors also
play vital role in the composition of intestinal microbiome.
The dysbiosis of intestinal microbiome was noted in high fat
and high sugar diet fed murine models.
Understanding the nuanced ways in which the microbiota
interacts with the host’s GI tract not only enhances our
comprehension of these diseases, but also opens potential
avenues for diagnostic and therapeutic interventions. This
review aims to provide an in-depth exploration of the intricate
relationship between the gut microbiome and the host
immune system, specifically in the context of GI diseases.
Literature Review
Gastroesophageal Reflux Disease
Gastroesophageal Reflux Disease (GERD) is one of the most
widespread GI diseases with its prevalence over 25% in
western countries [7]. The previously accepted etiology of
GERD was an inflammatory response to gastric acid reflux
from direct luminal mucosal injury. However, recent studies
are investigating the propagation of the intraluminal
inflammatory pathway through an immunogenic response to
the Esophageal Microbiome (EM) as a possible contributor to
the pathogenesis of GERD [8,9].
The normal esophageal microbiota is mainly composed of
gram-positive bacteria Firmicutes spp., Bacteroidetes spp., Proteobacteria spp., Fusobacteria spp., Actinobacteria spp., Saccharibacteria spp. Firmicutes is the most dominant phylum
and Streptococcus is the most prevalent genus [10]. The EM
exhibits a microgeographic gradient, with gram-positive flora
being more prevalent proximally and an increasingly diverse
gram-negative composition distally [11]. Shifts in the
esophageal continuum from gram-positive to gram-negative
bacteria have been found to precede histological changes,
suggesting that dysbiosis in the EM plays a role in developing
pathological states of the esophagus [12]. The composition of
the EM is affected by gastric refluxate and distal migration of
bacteria from the oral cavity. Environmental factors like
diet, age, smoking status and proton pump inhibitor use
also contribute to interpersonal variability in
esophageal microbiota [13].
Gram-negative bacteria contribute to the
immunopathogenesis of GERD through the
Lipopolysaccharide (LPS) Toll-Like-Receptor-4 (TLR4) pathway.
Increased prevalence of LPS containing gram-negative spp. in the distal esophagus leads to an inflammatory cascade
through the interaction of LPS with TLR-4. This sequence
promotes Nuclear Factor kappa B (NF-κB) and Interferongamma
(IFN-γ), leading to a cytokine cascade of interleukin
(IL)-1B, IL-8, IL-18 and Tumor Necrosis Factor-alpha (TNF-α),
ultimately resulting in transmucosal lymphocytic proliferation
and resultant inflammation [14]. Moreover, this cytokine
pathway leads to increased Nitric Oxide (NO) synthase activity,
causing reduced gastric motility and increased relaxation of
the Lower Esophageal Sphincter (LES), increasing gastric acid
refluxate exposure to the distal esophagus further
propagating this inflammatory pathway in a cyclical pattern
[15].
Gastrointestinal microbiota produces peptides called
bacteriocins whose role is to compete with pathogenic flora,
improve the Gut-Blood Barrier (GBB) and modulate the
immune system. The gut-blood barrier is crucial to
maintaining homeostasis between the bloodstream and the
gastrointestinal tract of the esophagus [16]. Studies examining
the pivotal role of the GBB show that bacteriocins produced
from probiotics Streptococcus spp., Bi idobacterium spp. and Lactobacillus spp. can reduce IL-6 and IL-17, pro-inflammatory
cytokines, stimulating expression of Tight Junction (TJ)
proteins, promoting gastrointestinal-blood barrier stability
[17,18]. Furthermore, administration of Lactobacillus
rhamnosus GG decreased pro-inflammatory cytokines, TNF-α
and Macrophage Inflammatory Protein 2 (MIP-2) in the GI
tract of murine models through increasing IL-10 receptor
expression [19]. Unfavorable compositional changes to the EM
and subsequent altered bacteriocin expression could lead to
GBB instability and inflammatory pathways propagation,
which could contribute to disease progression in GERD.
Defensins, like bacteriocins but of eukaryotic origin, are small
polypeptides that contribute to innate immunity through
bactericidal properties. Bacterial products, such as cytokines
or LPS, induce the expression of defensins, which can disrupt
bacterial cell membranes, promote pore formation in bacterial
capsules and propagate the adaptive immune system [20].
The loss of defensins could result in esophageal dysbiosis from
unmitigated gram-negative bacterial activity with resulting
esophageal inflammation through the LPS-TLR4-NF-ΚB
pathway, ultimately leading to the propagation of GERD [21].
Understanding the intricate interchanges between the
esophageal microbiome and the immune system is crucial to
treating GERD effectively. The esophageal dysbiosis with
transition to gram negative bacteria and its metabolites along
with resultant proinflammatory cytokines further instigates
the disease in its proinflammatory state. By acknowledging
the significance of therapeutic interventions that restore
microbial balance and modulate immune responses, we can
explore the role of the microbiome in GERD and develop
targeted treatments that focus on optimizing microbial and
immune system interactions. This developing narrative invites
further investigation and presents an opportunity to mitigate
the sequela of this disease.
Discussion
Barrett’s Esophagus
Barrett’s Esophagus (BE) is a disease of the distal esophagus
characterized by the replacement of squamous mucosa with
metaplastic columnar epithelium and is associated with
longstanding and uncontrolled GERD. As with GERD, the
incidence of BE has increased with higher uses of
antimicrobials, suggesting that esophageal dysbiosis
contributes to BE’s inflammatory and malignant pathogenesis
[22].
Columnar metaplasia arises from the expression of specific
cytokines in the distal esophagus, resulting in chronic
inflammation and subsequent stimulation of gastric stem
cells. As seen in GERD, a higher concentration of gramnegative
bacteria in the distal esophagus results in further LPS
and TLR interaction, ultimately leading to the inflammatory
and metaplastic changes that characterize BE [23].
Specifically, IL-1b, a pro-inflammatory cytokine, is found to be
expressed to a high degree in BE. The protease caspase-1
accomplishes proteolytic cleavage of the precursor to IL-1b
[24]. Inflammasomes containing Pattern-Recognition
Receptors (PRRs) interact with Pathogen-Associated
Molecular Patterns (PAMPs) from microbes in the distal
esophagus, leading to activation of caspase-1 and initiating
inflammation [25]. Notably, the lipopolysaccharides seen in
the outer membrane of gram-negative bacteria interact with
NOD-like receptor protein 3 inflammasomes in Barrett’s
epithelial cells, resulting in apoptosis and metaplastic
inflammatory changes [26]. Higher proportions of LPS
containing gram-negative bacteria could lead to upregulation
of cyclooxygenase (COX), isoenzymes COX-1 and -2, producing
Prostaglandins (PG) and leading to delayed gastric emptying,
reduction in lower esophageal sphincter tone and increased
intra gastric pressure, which could promote reflux and
subsequent inflammation seen in BE [27]. Similar to GERD,
tight junction proteins are essential in the relationship
between the innate immune response and the pathogenesis
of BE. Inflammatory changes from the higher presence of
gram-negative and anaerobes in the distal esophagus result in
the activation of Wnt signaling that creates defects in the tight
junction proteins and reduces mucin production, both of
which have protective roles from carcinogenesis. [28].
The LPS-TLR4-NF-ΚB inflammatory pathway observed in GERD
is also present in BE, but distinct dysbiosis related changes
drive the metaplasia in BE. According to a study, Neisseria spp. Campylobacter spp. and Fusobacteria spp. are more prevalent
in samples from BE than in non-BE controls [29]. Furthermore,
decreased bacterial diversity and lower prevalence of Bacteroidetes spp. and Prevotella spp. are observed when
analyzing the metaplastic tissue of Barrett’s compared to
normal esophageal tissue [30]. In GERD, an abundance of Proteobacteria spp. is seen with Bacteroidetes spp. however, a
shift towards higher proportions of Fusobacteria spp. with less Bacteroidetes spp. is found in BE. As dysplastic changes
progress to Esophageal Adenocarcinoma (EAC), a
compositional change in the EM occurs with increased prevalence in Firmicutes [31].
Additionally, Helicobacter pylori (H. pylori) has been
postulated to contribute to the pathogenesis of BE by
expressing inflammatory NF-κB and COX-2 in distal esophageal
epithelial cells [32]. It is worth noting that several factors can
lead to changes in the esophageal microbiome, just like in
GERD. Specifically, in the case of Barrett’s esophagus, studies
have shown a correlation between High-Fat Diets (HFD) and
dysbiosis-related changes in the balance between Bacteroides
spp. and Firmicutes spp. bacteria [33].
Similar to GERD, the observed esophageal dysbiosis and
proinflammatory state in BE are crucial in understanding the
disease. The complex interaction between microbial
dynamics, inflammatory responses and environmental factors
highlights the necessity for a comprehensive and
multidimensional approach to managing and investigating
Barrett's esophagus, opening the way for potential
therapeutic interventions.
Eosinophilic Esophagitis
Eosinophilic Esophagitis (EoE) is a Th2 antigen-mediated,
chronic inflammatory condition marked by eosinophilic
inflammation in the esophagus. The complexity of the disease
is closely influenced by interactions of the gut microbiome and
immune responses [34]. Although the exact cause and
pathophysiology remain unclear, it is currently thought to be
the outcome of a confluence of genetic, environmental and
immunological factors. Evidence suggests that a compromised
epithelial barrier facilitates allergen contact with the
esophageal mucosa, triggering alarmin release. These
alarmins, acting through type 2 Innate Lymphoid Cells (ILC2s)
and basophils, initiate a cytokine driven immune response,
leading to eosinophilic inflammation and increased barrier
disruption. Simultaneously, tissue-resident antigen-presenting
cells activate CD4+ T helper type 2 cells, which recruit and
activate eosinophils, mast cells and plasma cells, resulting in
localized IgE and IgG4 production [35,36]. IgE release
subsequently triggers TGF-β release from mast cells,
contributing further to inflammation and fibrosis [37]. Recent
research has shed light on the potential role of the innate
immune system and the microbial pattern recognition
receptors can play in the pathogenesis of EoE.
Studies examining the profile of esophageal microbiota of
those with EoE revealed enrichment of Neisseria spp. and Corynebacterium spp. in patients with EoE compared to those
without EoE. Furthermore, patients with active EoE have been
found to have increased microbial load, as well as increased
abundance of Haemophilus spp. and a decrease of specific
members of the Firmicutes phylum [38]. Subsequently,
compared to healthy individuals, an increased bacterial load
was evident in patients with EoE, irrespective of their
treatment status or the degree of mucosal eosinophilia,
explicitly demonstrating a significant abundance of Haemophilus [39].
The ability of Haemophilus spp. to penetrate epithelial cells
suggests opportunistic bacteria could take advantage of the
compromised barrier in EoE, contributing to persistent inflammation [40,41]. Haemophilus is linked to various Th2-
mediated conditions, such as recurrent pediatric asthma,
chronic obstructive pulmonary disease and rhinosinusitis, all
of which suggest that these bacteria may play a role in fueling
inflammation in EoE [42-44].
Investigating the role of microbiota in esophageal mucosa
inflammation is essential, given its potential connection to
initiating and perpetuating inflammation on mucosal surfaces.
Current evidence indicates that microbiota penetration
activates epithelial cells and innate and adaptive immune
cells, triggering the release of cytokines and subsequent
immune responses and inflammation. Toll-like receptors'
involvement in EoE further underscores the potential impact
of microbiota on disease progression. Evidence that compared
to healthy individuals, bacterial load and specific TLRs are
overexpressed in EoE patients, rectified following dietary
therapy-induced remission and mucosal healing, further
supports this association of microbiota and immunologic
response [45]. The TLRs, as microbial pattern recognition
receptors found on epithelial and lamina propria cells, play a
crucial role in distinguishing between pathogens and
commensal microorganisms. This implies that heightened
exposure of the microbiota and microbial products to the
compromised esophageal mucosal barrier could elevate the
release of alarmins by esophageal epithelial cells, contributing
to the progression of esophageal inflammation. This
upregulation of TLRs suggests a pivotal role for microbiota in
the disease's pathophysiology. The functional TLR-mediated
signaling pathways in the esophageal mucosa of active EoE
patients activate the innate immune system in the esophagus,
contributing to cellular damage.
The relationship between eosinophilic esophagitis, the
microbiome and immune responses in gastrointestinal
diseases is complex and dynamic. Understanding how these
interactions contribute to immune dysregulation and
inflammation can help focus therapies on developing balance
in the microbiome and enhancing barrier integrity. This
approach would address the disease's symptomatic aspects
and its underlying etiology. Further research is needed to
clarify specific interactions between the esophageal
microbiome and the immune system as they relate to EoE to
develop more effective treatment strategies.
Esophageal Cancer
Esophageal Cancer (EC) is an aggressive malignancy, ranking
as the eighth most diagnosed cancer and the sixth most
common cause of cancer death in the world [46]. Although
Esophageal Squamous Cell (ESCC) carcinoma is the most
prevalent type worldwide, Esophageal Adenocarcinoma (EC)
is increasing in prevalence in developed countries [47].
Increasing evidence suggests that achieving a thorough
comprehension of the molecular composition of esophageal
cancer necessitates focusing not only on tumor cells but also
on the tumor microenvironment. This microenvironment
comprises diverse cell populations, signaling factors and
structural molecules that engage with tumor cells and play
supportive roles across all stages of tumorigenesis [48]. The dynamic interplay between the host's microbiota and the
immune system is emerging as a critical factor influencing the
development, progression and treatment outcomes of
esophageal malignancies.
As in other states of esophageal disease, the microbiota in
esophageal cancer is characterized by reduced microbial
diversity characterized by a shift from gram-positive to gramnegative
bacteria. The genera most enriched in esophageal
cancer are Fusobacterium, Streptococcus, Peptostreptococcus, Veilonella, Actinobacillus, Gemella, Rothia and Prevotella [49,50]. A study done by Jing et al., studied the microbiota
spectrum of ESCC patients and demonstrated a significant
difference in the microbial diversity and richness between the
ESCC patients; the results provided a potential association of Streptococcus spp., Actinobacillus spp., Peptostreptococcus spp., Fusobacterium spp. and Prevotella spp. with ESCC [51].
Reduced microbial diversity in ESCC patients could indicate a
shift towards an environment conducive to chronic
inflammation and tumorigenesis.
Specific bacteria, such as Porphyromonas gingivalis and Fusobacterium nucleatum, have been implicated in promoting
carcinogenesis in ESCC. These bacteria play a role in ESCC cell
proliferation and migration through the TLR4/NF-κB and IL-6/
STAT3 pathways, contributing to either disease progression or
drug resistance [52]. Gao et al., identified P. gingivalis infects
the epithelium of the esophagus of ESCC patients and
established an association between infection with P. gingivalis and the progression of ESCC, which suggests P. gingivalis infection could be a biomarker for disease progression [53].
Studies indicate that P. gingivalis activates the NF-κB pathway
in ESCC cells, promoting proliferation and motility. Animal
models link P. gingivalis infection to advanced esophageal
cancer stages and poor prognosis via the IL-6/STAT3 pathway,
contributing to chemotherapy resistance. Clinical findings
reveal elevated P. gingivalis in ESCC patients' saliva and tumor
sites compared to controls. The presence of P. gingivalis infection correlates with ESCC severity and poor prognosis,
indicating its role in disease progression, chemotherapy
resistance and unfavorable outcomes through NF-κB and IL-6/
STAT3 pathways [54].
Fusobacterium nucleatum is closely related to increased
tumor staging and gene mutations such as TP53, COL22A1,
TRBV10-1, CSMD3, SCN7A and PSG11 [55]. This suggests that
the abundance of Fusobacterial nucleatum and tumor
mutation burden may be combined as a potential method to
predict high risk for metastasis in ESCC [56]. Additionally,
more recent studies have found that Fusobacterium
nucleatum promoted the early development of ESCC by
upregulating the expression of IL-32/PRTN3 and activating the
PI3K/AKT signaling pathway [57]. These findings highlight the
significant roles of Porphyromonas gingivalis and Fusobacterium nucleatum in influencing the course and
outcomes of esophageal squamous cell carcinoma.
Therapeutic manipulation of the microbiota, such as
probiotics and prebiotics, could serve as adjuncts to modulate
the tumor microenvironment and enhance the efficacy of
conventionally used treatments. This multifaceted approach emphasizes the need for a comprehensive understanding of
the microbial influences in esophageal cancer biology,
encouraging a broader perspective incorporating the
microbiome into the traditional paradigms of oncology.
Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) refers to a category of
chronic autoimmune conditions of the gastrointestinal tract.
The two most recognized types are Crohn’s Disease (CD) and
ulcerative colitis. These conditions can be differentiated by
clinical characteristics such as distribution, with UC limited to
the mucosal layer of the colorectal GI tract [58]. Either
condition can be characterized by relapsing symptoms of
diarrhea, abdominal pain and bloody stools. While the clinical
characteristics are well described, the underlying
pathogenesis is complex [59].
Recent developments have demonstrated that the intestinal
microbiota also plays a role in disease pathogenesis along
with genetic and environmental factors [60]. IBD is
characterized by intestinal epithelium damage secondary to
the infiltration of lymphocytes, neutrophils and macrophages
and dysregulation of the inflammatory response. The
detection of intestinal flora in the GI epithelium initiates this
response. As such, dysregulation of the delicate interactions
between GI epithelial cells, intestinal flora and immune cells
can lead to the exaggerated immune response seen in IBD
[61].
The human GI tract consists of 100 trillion micro-organisms
and comprises over 1,000 different bacterial species. Pattern
Recognition Receptors (PRRs) are expressed throughout the
cells of the intestinal tract. These PRRs influence the
composition of the tract via the regulation of product (mucus,
antimicrobial peptides and immune mediators) secretion [62].
The four major PRR classes include TLRs, NLR, C-type lectin
receptors and RIG-1-like receptors. Much like in other
inflammatory-mediated diseases, TLRs in the intestines
recognize pathogen associated molecular patterns and
activate intracellular cascades, which lead to the transcription
of inflammatory cytokines. TLR-4, in particular, has
significantly been implicated in this process as it binds to LPS
found on gram-negative bacteria and leads to the
downstream activity of prominent inflammatory cytokines
such as TNF-a, IL-6, IL-1 and type-1 interferons, which all play
a role in inflammatory bowel disease [63].
The TLR-4 expression is elevated in individuals with
inflammatory bowel disease compared to normal individuals
[64]. Nod-Like Receptors (NLR) are also thought to play a role.
The Nucleotide-binding Oligomerization Domain 2 (NOD2)
receptor recognizes Muramyl Dipeptide (MDP) in
peptidoglycan, found in the cell walls of gram-positive and
gram-negative bacteria. The downstream effect is the
activation of NF-kB, which leads to the secretion of IL-12 and
other pro-inflammatory cytokines. The NOD2 gene is
frequently mutated in CD patients [65].
While the inflammatory cascade is a hallmark of IBD, another
key characteristic is intestinal microbiota dysbiosis. Further, there is a marked reduction in the diversity of the
microbiome. Specifically, reducing specific phyla such as
Actinobacteria, Firmicutes and Bacteroides is associated with
dysbiosis. Importantly, these organisms produce Short-Chain
Fatty Acids (SCFAs), which act as anti-inflammatory products
in the intestines [66]. These findings seem reversible, as longterm
remission is associated with normalizing bacterial
microbiota and SCFA levels in fecal specimens. It should also
be noted that intestinal bacteria synthesize these fatty acids
from degrading indigestible carbohydrates. The implication is
that there is a complex interplay between diet, microbiome
composition and degree of inflammation and these
relationships should continue to be studied.
Beyond the distress from the symptoms of IBD, the disorder
can also have severe complications. Patients with IBD are at
increased risk of colon cancer. Having UC increases one’s risk
of developing colitis-associated cancer by 18%-20% and those
with CD are at an 8% increase [67].
The prevailing knowledge on IBD focuses on a multi-faceted
approach incorporating genetic, microbial and immune
factors. The recognition of the gut microbiota’s involvement in
disease pathogenesis in addition to the genetics and
environmental cues advances our understanding of IBD.
Notably, dysbiosis of the gut microbiome marked by a
reduction in diversity and specific bacterial phyla further
contributes the proinflammatory state in IBD. However,
emerging evidence suggests that intervention targeting
microbiome restoration and dietary modifications may hold
future for therapeutic intervention. The complex connections
between diet, microbiome composition and degree of
immune response present many opportunities for continuing
research and development.
Colon Cancer
Colorectal Cancer (CRC) is the second deadliest cancer in the
United States, with 52,550 deaths in 2023, including 3,750
individuals less than 50 years of age [68]. As with many other
GI illnesses discussed, CRC is associated with a change in the
composition of the intestinal microbiome. Compared to
healthy patients, the microbiome of CRC patients has
increased levels of Fusobacterium spp. and other gram
negatives. There are also increased levels of some gram
positives, such as Enterococcus faecalis, which has been
associated with the development of adenocarcinoma in IBD
patients.
Like in IBD, CRC is associated with a reduction of butyrateproducing
organisms. Like other SCFAs, butyrate acts as an
anti-inflammatory and an antioxidant, promoting the growth
of anaerobic bacteria [69]. Activation of the previously
described inflammatory also plays a role in the development
of CAC. Colitis-Associated Cancer (CAC) has a poorly
understood mechanism, but it appears that upregulation of
TLR-4 may trigger the proliferation of intestinal epithelial cells
and lead to carcinoma. Given that TLR-4 responds to LPS, an
association can be made between the make-up of the
intestinal microflora and the development of CAC.
Beyond their propensity to trigger inflammatory cascades
through the binding of PRRs, the gut microbiota also
influences the development of neoplasia by producing protein
toxins, which promote proliferation and reduce apoptosis.
These include Cytolethal Distending Toxins (CDT) and DNAdamaging
toxins from gram-negative bacteria. Persistent
exposure to these toxins can reduce their DNA-damaging
effects via mutations and tolerance. As such, a microbiome
abundant with organisms that produce these toxins can be
associated with the development of CAC.
Another instance of gram-negative bacteria impacting
neoplasia is the case of Bacteroides fragilis, which produces Bacteroides fragilis Toxins (BFTs). These BFRs bind to Ecadherin
in the intestinal epithelial cell, releasing the protein
from the tumor suppressor protein, beta catenin. Once
released, E-cadherin becomes an active transcription factor
that promotes cell proliferation. Furthermore, BFTs also
reduce apoptosis of intestinal epithelial cells, augmenting
neoplasia.
Collectively, these findings highlight the potential of targeting
microbial components in CRC as an avenue for prevention or
therapy. Strategies may include microbiome regulation
through diet, probiotics or antimicrobials and direct targeting
of notable bacterial toxins or inflammatory pathway identified
in CRC.
Hepatobiliary Diseases
Hepatobiliary diseases, encompassing Hepatocellular
Carcinoma (HCC), are intricately shaped by the interplay
between the gut microbiome and immunotherapy. Recent
research illuminates this complex relationship, with the gut
microbiota composition emerging as a robust predictor of
immune checkpoint therapy response in hepatobiliary
diseases [70]. The comprehension of the gut-liver axis proves
crucial in unraveling the mechanisms of chronic liver diseases,
such as Non-Alcoholic Fatty Liver Disease (NAFLD), intricately
connected to the gut microbiota [71]. Exploring interactions
between gut microbes and the tumor immune
microenvironment reveals promising avenues for
immunotherapeutic interventions in liver cancer [72].
Numerous studies highlight the profound connection between
the GI microbiome and its communication with the liver. Key
players in this interaction include the portal vein and biliary
system. The portal vein facilitates the direct transportation of
immune cells, cytokines and gut-derived products to the liver.
In contrast, the liver reciprocates by secreting bile and
bioactive mediators into the intestine via the biliary system.
The intricate structure of the gut vascular and single layer
epithelial cells, bound by tight junction proteins, along with
the mucus layer and microorganisms, forms a robust physical
barrier. Components like antimicrobial molecules and
Secreted Immunoglobulin A (SIgA) contribute to maintaining
biochemical barriers. The intestinal barrier, functioning as the
first line of defense in human immunity, complements the
liver's role as the second line of defense against pathogenic
factors escaping from the intestinal mucosal immune defense
[73].
Gastrointestinal microbiome dysbiosis can compromise these
barriers, heightening mucosal permeability. Dietary factors
impact the composition of the intestinal microbiome and play
a crucial role in preserving the integrity of the intestinal
barrier. The pathological state induced by a high-fat diet
results in bacterial translocation and endotoxin entry into the
portal venous system, activating immune cells in the liver and
triggering inflammatory responses, ultimately causing tissue
damage to the intestinal mucosa, liver and systemic organs
[74].
The close relationship between the gut and the liver in
immune pathogenesis underscores its significance for
translational therapy [75]. The hepatic immunological
response triggered by gut permeability, especially the role of
Kupffer cells in the initial immune response, is explored.
Continuous exposure of the liver to gut microbiome
components through the portal vein emerges as a critical
factor influencing liver adaptation.
The intricate interplay between the gut microbiome and
immunotherapy in hepatobiliary diseases such as HCC
highlights the importance of understanding the gut-liver axis.
Central to the relationship of gut liver axis are the portal vein
and biliary system which facilitate bidirectional
communication between the gut and liver. Dysbiosis of the GI
microbiome can compromise the integrity of the intestinal
barrier. Additionally, dietary factors play a crucial role in
modulating the gut microbiome and the intestinal barrier
function. As our understanding of these intricate interactions
advances, translational therapies target the gut liver axis hold
promise for improved management of hepatobiliary diseases.
Conclusion
The intricate relationship between the GI microbiome and the
immune system has been revealed as a pivotal factor in the
pathogenesis of various GI diseases, including GERD, BE, EoE,
IBD, colon cancer and hepatobiliary disease. Through a
comprehensive exploration of existing studies, it becomes
evident that microbial dysbiosis eliciting an immune response
has a cyclic mechanism that potentially fuels these diseases'
development and/or progression. Recognizing the gut
microbiome as a critical player in the pathophysiology of GI
disorders provides a foundation for developing strategies to
modulate the microbiome and harness its potential for clinical
applications. Future research promises to unveiling novel
therapeutic approaches that can address the diseases provide
personalized medicine.
Author Contributions
David A. Johnson MD and Byung Soo Yoo MD contributed to
the construction of the project; all authors wrote and edited
the manuscript.
Conflicts of Interest
David A Johnson MD research investigator for ISOTHRIVE.
References
- Marchesi JR, Adams DH, Fava F, Hermes GD, Hirschfield GM, et al. (2016) The gut microbiota and host health: A new clinical frontier. Gut. 65(2):330-339.
[Crossref][Google Scholar][PubMed]
- Sender R, Fuchs S, Milo R (2016) Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 14(8): 533-536.
[Crossref][Google Scholar][PubMed]
- Shi N, Li N, Duan X (2017) Interaction between the gut microbiome and mucosal immune system. Military Med Res. 24:1-7.
[Crossref][Google Scholar][PubMed]
- Harmsen HJ, de Goffau MC (2016) The human gut microbiota. Adv Exp Med Biol. 902:95-108.
[Crossref][Google Scholar][PubMed]
- Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, et al. (2005) Diversity of the human intestinal microbial flora. Science. 308(5728):1635-1638.
[Crossref][Google Scholar][PubMed]
- Liu J, Tan Y, Cheng H, Zhang D, Feng W, et al. (2022) Functions of gut microbiota metabolites, current status and future perspectives. Aging Dis. 13(4):1106.
[Crossref][Google Scholar][PubMed]
- El-Serag HB, Sweet S, Winchester CC, Dent J (2014) Update on the epidemiology of gastro-oesophageal reflux disease: A systematic review. Gut. 63(6):871-880.
[Crossref][Google Scholar][PubMed]
- Wang K, Wang S, Chen Y, Lu X, Wang D, et al. (2024) Causal relationship between gut microbiota and risk of gastroesophageal reflux disease: A genetic correlation and bidirectional Mendelian randomization study. Front Immunol. 15:1327503.
[Crossref][Google Scholar][PubMed]
- Mazgaeen L, Gurung P (2020) Recent advances in lipopolysaccharide recognition systems. Int J Mol Sci. 21(2):379.
[Crossref][Google Scholar][PubMed]
- Pei Z, Bini EJ, Yang L, Zhou M, Francois F, et al. (2004) Bacterial biota in the human distal esophagus. Proc Natl Acad Sci. 101(12):4250-4255.
[Crossref][Google Scholar][PubMed]
- Dong L, Yin J, Zhao J, Ma SR, Wang HR, et al. (2018) Microbial similarity and preference for specific sites in healthy oral cavity and esophagus. Front Microbiol. 9:1603.
[Crossref][Google Scholar][PubMed]
- Blackett KL, Siddhi SS, Cleary S, Steed H, Miller MH, et al. (2013) Oesophageal bacterial biofilm changes in gastroâ?oesophageal reflux disease, Barrett's and oesophageal carcinoma: Association or causality? Aliment Pharmacol Ther. 37(11):1084-1092.
[Crossref][Google Scholar][PubMed]
- D'Souza SM, Houston K, Keenan L, Yoo BS, Parekh PJ, et al. (2021) Role of microbial dysbiosis in the pathogenesis of esophageal mucosal disease: A paradigm shifts from acid to bacteria? World J Gastroenterol. 27(18):2054.
[Crossref][Google Scholar][PubMed]
- Zavala-Solares MR, Fonseca-Camarillo G, Valdovinos M, Granados J, Grajales-Figueroa G, et al. (2021) Gene expression profiling of inflammatory cytokines in esophageal biopsies of different phenotypes of gastroesophageal reflux disease: A cross-sectional study. BMC Gastroenterol. 21:1-9.
[Crossref][Google Scholar][PubMed]
- PishKenari FN, Qujeq D, Bonahi SS, Kashifard M, Hajian-Tilaki K (2022) Nitric oxide and inducible nitric oxide synthase levels in EE and NERD patients. Gastroenterol Hepatol Bed Bench. 15(1):79.
[Google Scholar][PubMed]
- Dicks LM, Dreyer L, Smith C, van Staden AD (2018) A review: The fate of bacteriocins in the human gastro-intestinal tract: Do they cross the gutâ??blood barrier? Front Microbiol. 9:2297.
[Crossref][Google Scholar][PubMed]
- Wang Y, Kasper LH (2014) The role of microbiome in central nervous system disorders. Brain Behav Immun. 38:1-12.
[Crossref][Google Scholar][PubMed]
- Ling X, Linglong P, Weixia D, Hong W (2016) Protective effects of bifidobacterium on intestinal barrier function in LPS-induced enterocyte barrier injury of Caco monolayers and in a rat NEC model. PloS One. 11(8):e0161635.
[Crossref][Google Scholar][PubMed]
- Mirpuri J, Sotnikov I, Myers L, Denning TL, Yarovinsky F, et al. (2012) Lactobacillus rhamnosus (LGG) regulates IL-10 signaling in the developing murine colon through upregulation of the IL-10R2 receptor subunit. PLoS One. 7(12):e51955.
[Crossref][Google Scholar][PubMed]
- Machado LR, Ottolini B (2015) An evolutionary history of defensins: A role for copy number variation in maximizing host innate and adaptive immune responses. Front Immunol. 6:115.
[Crossref][Google Scholar][PubMed]
- Schroeder S, Robinson ZD, Masterson JC, Hosford L, Moore W, et al. (2013) Esophageal human β-defensin expression in eosinophilic esophagitis. Pediatr Res. 73(5):647-654.
[Crossref][Google Scholar][PubMed]
- Yu G, Gail MH, Shi J, Klepac-Ceraj V, Paster BJ, et al. (2014) Association between upper digestive tract microbiota and cancer-predisposing states in the esophagus and stomach. Cancer Epidemiol Biomarkers Prev. 23(5):735-741.
[Crossref][Google Scholar][PubMed]
- Yang L, Lu X, Nossa CW, Francois F, Peek RM, et al. (2009) Inflammation and intestinal metaplasia of the distal esophagus are associated with alterations in the microbiome. Gastroenterology. 137(2):588-597.
[Crossref][Google Scholar][PubMed]
- Quante M, Bhagat G, Abrams JA, Marache F, Good P, et al. (2012). Bile acid and inflammation activate gastric cardia stem cells in a mouse model of Barrett-like metaplasia. Cancer Cell. 21(1):36-51.
[Crossref][Google Scholar][PubMed]
- Oâ??Neill LA (2002) Signal transduction pathways activated by the IL-1 receptor/toll-like receptor superfamily. Curr Top Microbiol Immunol. 270:47-61.
[Google Scholar][PubMed]
- Nadatani Y, Huo X, Zhang X, Yu C, Cheng E, et al. (2016) NOD-like receptor protein 3 inflammasome priming and activation in Barrettâ??s epithelial cells. Cell Mol Gastroenterol Hepatol. 2(4):439-453.
[Crossref][Google Scholar][PubMed]
- Verbeek RE, Siersema PD, Ten Kate FJ, Fluiter K, Souza RF, et al. (2014) Toll-like receptor 4 activation in Barrettâ??s esophagus results in a strong increase in COX-2 expression. J Gastroenterol. 49:1121-1134.
[Crossref][Google Scholar][PubMed]
- Jovov B, Shaheen NJ, Orlando GS, Djukic Z, Orlando RC (2013) Defective barrier function in neosquamous epithelium. Am J Gastroenterol T. 108(3):386-391.
[Crossref][Google Scholar][PubMed]
- Macfarlane S, Furrie E, Macfarlane GT, Dillon JF (2007) Microbial colonization of the upper gastrointestinal tract in patients with Barrett's esophagus. Clin Infect Dis. 45(1):29-38.
[Crossref][Google Scholar][PubMed]
- Lopetuso LR, Severgnini M, Pecere S, Ponziani FR, Boskoski I, et al. (2020). Esophageal microbiome signature in patients with Barrettâ??s esophagus and esophageal adenocarcinoma. PLoS One. 15(5):e0231789.
[Crossref][Google Scholar][PubMed]
- Zhou J, Shrestha P, Qiu Z, Harman DG, Teoh WC, et al. (2020) Distinct microbiota dysbiosis in patients with non-erosive reflux disease and esophageal adenocarcinoma. J Clin Med. 9(7):2162.
[Crossref][Google Scholar][PubMed]
- Kountouras J, Zavos C, Polyzos SA, Katsinelos P (2015) Helicobacter pylori infection and gastroesophageal reflux disease-Barrett's esophagus sequence "dilemma". Ann Gastroenterol. 2015:153.
[Google Scholar][PubMed]
- Sonnenburg ED, Zheng H, Joglekar P, Higginbottom SK, Firbank SJ, et al. (2010) Specificity of polysaccharide use in intestinal bacteroides species determines diet-induced microbiota alterations. Cell. 141(7):1241-1252.
[Crossref][Google Scholar][PubMed]
- Mennini M, Tambucci R, Riccardi C, Rea F, de Angelis P, et al. (2021) Eosinophilic esophagitis and microbiota: State of the art. Front Immunol. 12:595762.
[Crossref][Google Scholar][PubMed]
- Clayton F, Fang JC, Gleich GJ, Lucendo AJ, Olalla JM, et al. (2014) Eosinophilic esophagitis in adults is associated with IgG4 and not mediated by IgE. Gastroenterology. 147(3):602-609.
[Crossref][Google Scholar][PubMed]
- Mitson-Salazar A, Yin Y, Wansley DL, Young M, Bolan H, et al. (2016) Hematopoietic prostaglandin D synthase defines a proeosinophilic pathogenic effector human TH2 cell subpopulation with enhanced function. J Clin Immunol. 137(3):907-918.
[Crossref][Google Scholar][PubMed]
- Mishra A, Rothenberg ME (2003) Intratracheal IL-13 induces eosinophilic esophagitis by an IL-5, eotaxin-1 and STAT6-dependent mechanism. Gastroenterology. 125(5):1419-1427.
[Crossref][Google Scholar][PubMed]
- Benitez AJ, Hoffmann C, Muir AB, Dods KK, Spergel JM, et al. (2015) Inflammation associated microbiota in pediatric eosinophilic esophagitis. Microbiome. 3:1-1.
[Crossref][Google Scholar][PubMed]
- Harris JK, Fang R, Wagner BD, Choe HN, Kelly CJ, et al. (2015) Esophageal microbiome in eosinophilic esophagitis. PloS One. 10(5):e0128346.
[Crossref][Google Scholar][PubMed]
- Clementi CF, Hakansson AP, Murphy TF (2014) Internalization and trafficking of nontypeable Haemophilus influenzae in human respiratory epithelial cells and roles of IgA1 proteases for optimal invasion and persistence. Infect Immun. 82(1):433-444.
[Crossref][Google Scholar][PubMed]
- Clementi CF, Murphy TF (2011) Non-typeable Haemophilus influenzae invasion and persistence in the human respiratory tract. Front Cell Infect Microbiol. 1:1.
[Crossref][Google Scholar][PubMed]
- Hoggard M, Biswas K, Zoing M, Wagner Mackenzie B, Taylor MW, et al. (2017) Evidence of microbiota dysbiosis in chronic rhinosinusitis. Int Forum Allergy Rhinol. 7(3):230-239.
[Crossref][Google Scholar][PubMed]
- Chunxi L, Haiyue L, Yanxia L, Jianbing P, Jin S (2020) The gut microbiota and respiratory diseases: New evidence. J Immunol Res. 2020(1):2340670.
[Crossref][Google Scholar][PubMed]
- Hufnagl K, Pali-Scholl I, Roth-Walter F, Jensen-Jarolim E (2020) Dysbiosis of the gut and lung microbiome has a role in asthma. Semin Immunopathol. 42(1): 75-93.
[Crossref][Google Scholar][PubMed]
- Arias A, Vicario M, Bernardo D, Olalla JM, Fortea M, et al. (2018). Toll-like receptors-mediated pathways activate inflammatory responses in the esophageal mucosa of adult eosinophilic esophagitis. Clin Transl Gastroenterol. 9(4):e147.
[Crossref][Google Scholar][PubMed]
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, et al. (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 71(3):209-249.
[Crossref][Google Scholar][PubMed]
- Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V (2020) Epidemiology of esophageal cancer: Update in global trends, etiology and risk factors. Clin J Gastroenterol. 13(6):1010-1021.
[Crossref][Google Scholar][PubMed]
- Lin EW, Karakasheva TA, Hicks PD, Bass AJ, Rustgi AK (2016) The tumor microenvironment in esophageal cancer. Oncogene. 1:13.
[Crossref][Google Scholar][PubMed]
- Kovaleva O, Podlesnaya P, Rashidova M, Samoilova D, Petrenko A, et al. (2021) Prognostic significance of the microbiome and stromal cells phenotype in esophagus squamous cell carcinoma. Biomedicines. 9(7):743.
[Crossref][Google Scholar][PubMed]
- Yamamura K, Baba Y, Nakagawa S, Mima K, Miyake K, et al. (2016) Human microbiome Fusobacterium nucleatum in esophageal cancer tissue is associated with prognosis. Clin Cancer Res. 22(22):5574-5581.
[Crossref][Google Scholar][PubMed]
- Zou Q, Feng L, Cai X, Qian Y, Xu L (2023) Esophageal microflora in esophageal diseases. Front Cell Infect Microbiol. 13:1145791.
[Crossref][Google Scholar][PubMed]
- Jiang Z, Wang J, Shen Z, Zhang Z, Wang S (2021) Characterization of esophageal microbiota in patients with esophagitis and esophageal squamous cell carcinoma. Front Cell Infect Microbiol. 11:774330.
[Crossref][Google Scholar][PubMed]
- Gao S, Li S, Ma Z, Liang S, Shan T, et al. (2016) Presence of Porphyromonas gingivalis in esophagus and its association with the clinicopathological characteristics and survival in patients with esophageal cancer. Infect Agent Cancer. 11:3.
[Crossref][Google Scholar][PubMed]
- Chiang HC, Hughes M, Chang WL (2023) The role of microbiota in esophageal squamous cell carcinoma: A review of the literature. Thorac Cancer. 14(28):2821-2829.
[Crossref][Google Scholar][PubMed]
- Li Z, Shi C, Zheng J, Guo Y, Fan T, et al. (2021) Fusobacterium nucleatum predicts a high risk of metastasis for esophageal squamous cell carcinoma. BMC Microbiol. 21:1-4.
[Crossref][Google Scholar][PubMed]
- Lei J, Xu F, Deng C, Nie X, Zhong L, et al. (2023) Fusobacterium nucleatum promotes the early occurrence of esophageal cancer through upregulation of ILâ?32/PRTN3 expression. Cancer Sci. 114(6):2414-2428.
[Crossref][Google Scholar][PubMed]
- Yamamura K, Baba Y, Nakagawa S, Mima K, Miyake K, et al. (2016) Human microbiome Fusobacterium nucleatum in esophageal cancer tissue is associated with prognosis. Clin Cancer Res. 22(22):5574-5581.
[Crossref][Google Scholar][PubMed]
- Zhang M, Sun K, Wu Y, Yang Y, Tso P, et al. (2017) Interactions between intestinal microbiota and host immune response in inflammatory bowel disease. Front Immunol. 8:942.
[Crossref][Google Scholar][PubMed]
- Wilson JC, Furlano RI, Jick SS, Meier CR (2016) Inflammatory bowel disease and the risk of autoimmune diseases. J Crohns Colitis. 10(2):186-193.
[Crossref][Google Scholar][PubMed]
- Guan Q (2019) A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. 2019(1):7247238.
[Crossref][Google Scholar][PubMed]
- Abraham C, Abreu MT, Turner JR (2022) Pattern recognition receptor signaling and cytokine networks in microbial defenses and regulation of intestinal barriers: Implications for inflammatory bowel disease. Gastroenterology. 162(6):1602-1616.
[Crossref][Google Scholar][PubMed]
- Kuo WT, Lee TC, Yu LC (2016) Eritoran suppresses colon cancer by altering a functional balance in toll-like receptors that bind lipopolysaccharide. Cancer Res. 76(16):4684-4695.
[Crossref][Google Scholar][PubMed]
- Wu Y, Wu J, Chen T, Li Q, Peng W (2018) Fusobacterium nucleatum potentiates intestinal tumorigenesis in mice via a toll-like receptor 4/p21-activated kinase 1 cascade. Dig Dis Sci. 63:1210-1218.
[Crossref][Google Scholar][PubMed]
- Yamamoto S, Ma X (2009) Role of Nod2 in the development of Crohn's disease. Microbes Infect. 11(12):912-918.
[Crossref][Google Scholar][PubMed]
- Chia LW, Mank M, Blijenberg B, Aalvink S, Bongers RS, et al. (2020) Bacteroides thetaiotaomicron fosters the growth of butyrate-producing Anaerostipes caccae in the presence of lactose and total human milk carbohydrates. Microorganisms. 8(10):1513.
[Crossref][Google Scholar][PubMed]
- Grivennikov SI (2013) Inflammation and colorectal cancer: Colitis-associated neoplasia. Semin Immunopathol. 35:229-244.
[Crossref][Google Scholar][PubMed]
- Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A (2023) Colorectal cancer statistics, 2023. Cancer J Clin. 73(3):233-254.
[Crossref][Google Scholar][PubMed]
- Gubatan J, Boye TL, Temby M, Sojwal RS, Holman DR, et al. (2022) Gut microbiome in inflammatory bowel disease: Role in pathogenesis, dietary modulation and colitis-associated colon cancer. Microorganisms. 10(7):1371.
[Crossref][Google Scholar][PubMed]
- Mao J, Wang D, Long J, Yang X, Lin J, et al. (2021). Gut microbiome is associated with the clinical response to anti-PD-1 based immunotherapy in hepatobiliary cancers. J ImmunoTher Cancer. 9(12):e003334.
[Crossref][Google Scholar][PubMed]
- Tripathi A, Debelius J, Brenner DA, Karin M, Loomba R, et al. (2018) The gutâ??liver axis and the intersection with the microbiome. Nat Rev Gastroenterol Hepatol. 15(7):397-411.
[Crossref][Google Scholar][PubMed]
- Brandl K, Kumar V, Eckmann L (2017) Gut-liver axis at the frontier of host-microbial interactions. Am J Physiol Gastrointest Liver Physiol. 312(5):413-419.
[Crossref][Google Scholar][PubMed]
- Taniki N, Nakamoto N, Chu PS, Mikami Y, Amiya T, et al. (2018) Intestinal barrier regulates immune responses in the liver via IL-10-producing macrophages. JCI Insight. 3(12):e91980.
[Crossref][Google Scholar][PubMed]
- He LH, Yao DH, Wang LY, Zhang L, Bai XL (2021) Gut microbiome-mediated alteration of immunity, inflammation and metabolism involved in the regulation of non-alcoholic fatty liver disease. Front Microbiol. 12:761836.
[Crossref][Google Scholar][PubMed]
- Bozward AG, Ronca V, Osei-Bordom D, Oo YH (2021) Gut-liver immune traffic: Deciphering immune-pathogenesis to underpin translational therapy. Frontiers Immunol. 12:711217.
[Crossref][Google Scholar][PubMed]
- Chopyk DM, Grakoui A (2020) Contribution of the intestinal microbiome and gut barrier to hepatic disorders. Gastroenterology. 159(3):849-863.
[Crossref][Google Scholar][PubMed]
Citation: Yoo BS, Robinson BL, Vilela A, Elmahdi A, Houston K, et al. (2024) Gut Microbiome and Immune Responses in
Gastrointestinal Diseases. J Clin Gastroenterol Hepatol. 8:32.
Copyright: © 2024 Yoo BS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution
License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source
are credited.