Lauren Dawes1*, Animesh Singla2, Keryn Davidson3, Santosh Poonoose1 and Nick Vrodos1
1Department of Neurosurgery, Flinders Medical Centre, Bedford Park, Australia
2Department of Vascular Surgery, Port Macquarie Base Hospital, Port Macquarie, Australia
3Department of Neurosurgery, Royal North Shore Hospital, Australia
*Corresponding Author:
Lauren Dawes
Department of Neurosurgery, Flinders Medical Centre, Bedford Park, Australia
Tel: 0424736621
E-mail: lrndws@gmail.com
Received date: October 07, 2017; Accepted date: October 24, 2017; Published date: October 26, 2017
Citation: Dawes L, Singla A, Davidson K, Poonoose S, Vrodos N. Haemmorhage into a Septum Pellucidum Subependymoma: An Unusual Complication of a Benign Glial Neoplasm. Neurooncol Open Access 2017, Vol.2 No.1:4.
Copyright: © 2017 Dawes L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Subependymal glioma; Subependymoma; Intraventricular haemorrhage; Low grade glioma; Benign tumour; Neurosurgery; Brain tumour; Septum pellucidum
Introduction
Originally described in 1945 by Sheinker, SE’s are rare benign (WHO grade I) glial neoplasms representing 0.2-0.7% of all intracranial tumours [1,2]. Approximately 40% are symptomatic and classically present with symptoms of obstructive hydrocephalus, ataxia, visual changes and impaired cognition [3-5]. Rarely do they present with symptoms or signs of acute haemorrhage. To date there have been only thirteen reported cases of haemorrhage arising from subependymomas, with just two located at the septum pellucidum (SP). This report presents only the third case of SP haemorrhage and the first reported case of a co-existent meningiothelial meningioma.
Case Report
A 76-year-old male presented to the emergency department following a sudden-onset severe headache associated with nausea and unsteadiness of gait. His past medical history was significant for a complete resection of a right frontal lobe WHO Grade I meningiothelial meningioma two years prior, and a diagnosed synchronous intraventricular anterior septum pellucidum lesion. He also had significant history ischaemic heart disease, metallic aortic valve replacement (on warfarin) and an implanted defibrillator.
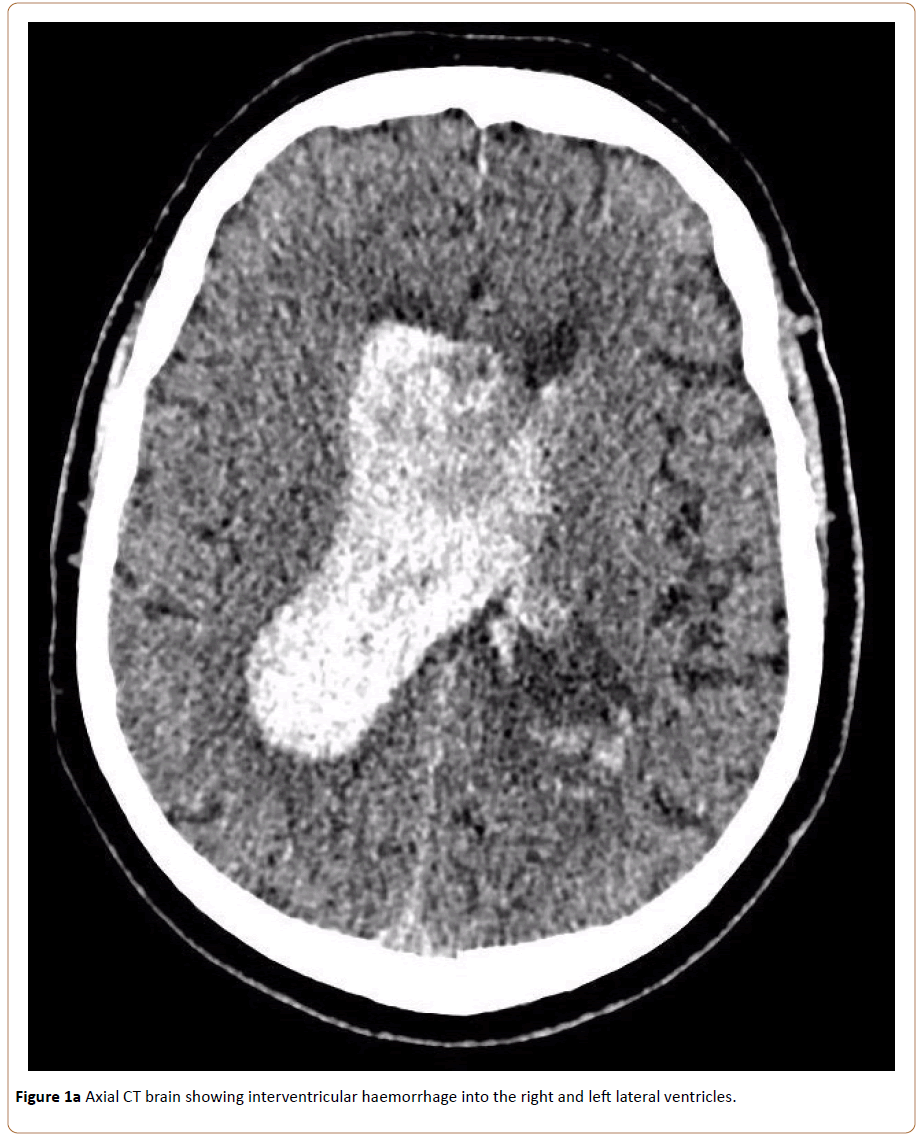
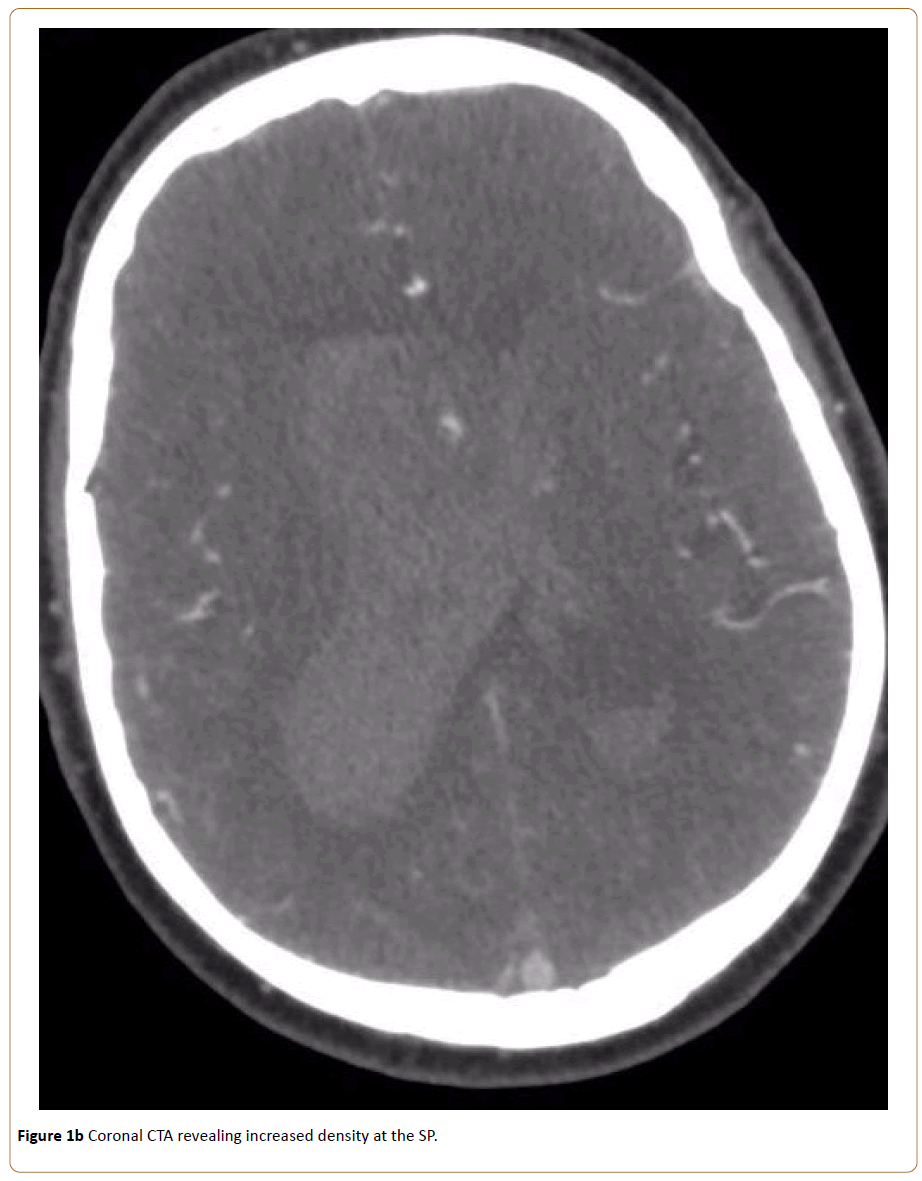
On initial presentation he had a left hemi-sensory neglect with reduced power in left arm flexion. Significant laboratory findings included an international normalized ratio (INR) of 2.5. Shortly thereafter, he experienced a rapid decline in his Glasgow Coma Score (GCS) necessitating intubation. Computed tomography (CT) brain showed a right lateral intraventricular haemorrhage extending to the third and fourth ventricles with associated acute hydrocephalus and transependymal CSF leak (Figure 1a). Concurrent CT angiography revealed increased density at the SP raising suspicion for the known lesion as the causative agent (Figure 1b). A magnetic resonance imaging scan was not possible as the patient’s prior metallic valve replacement was incompatible.
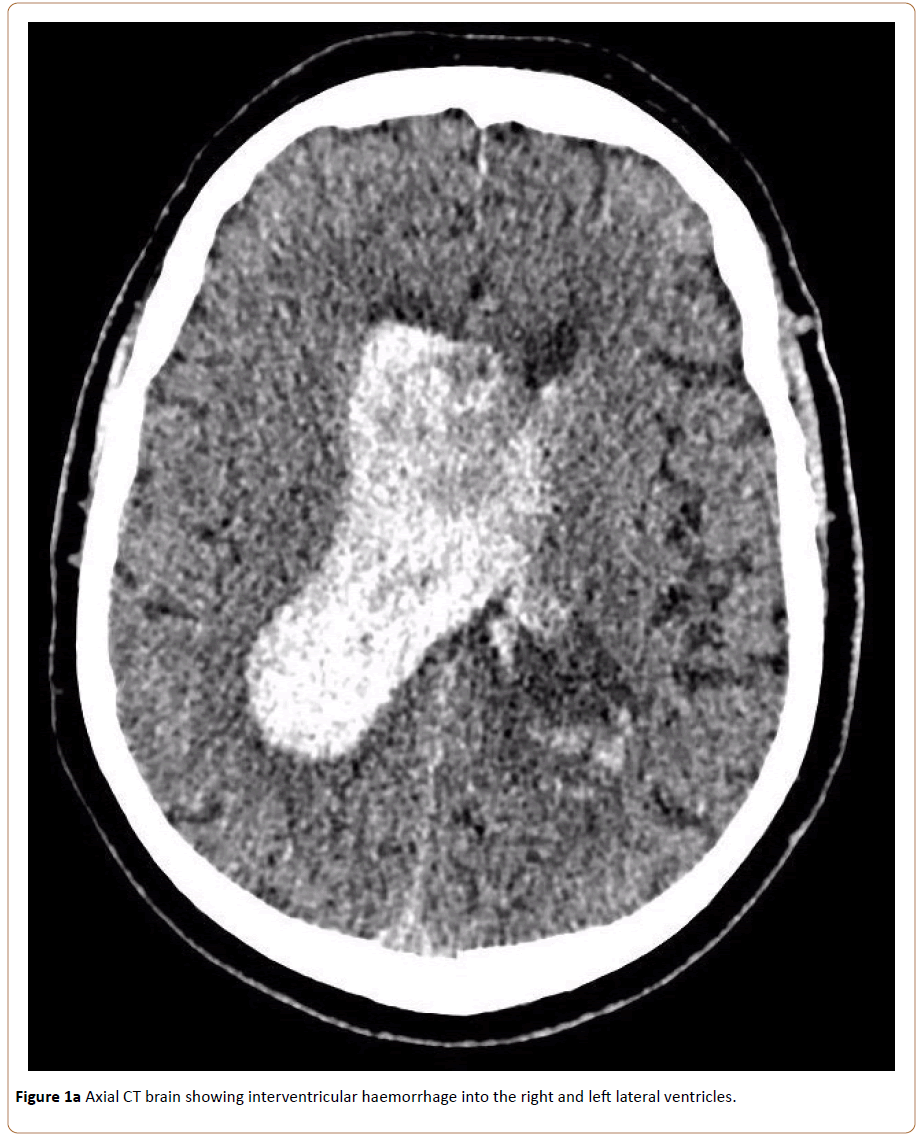
Figure 1a: Axial CT brain showing interventricular haemorrhage into the right and left lateral ventricles.
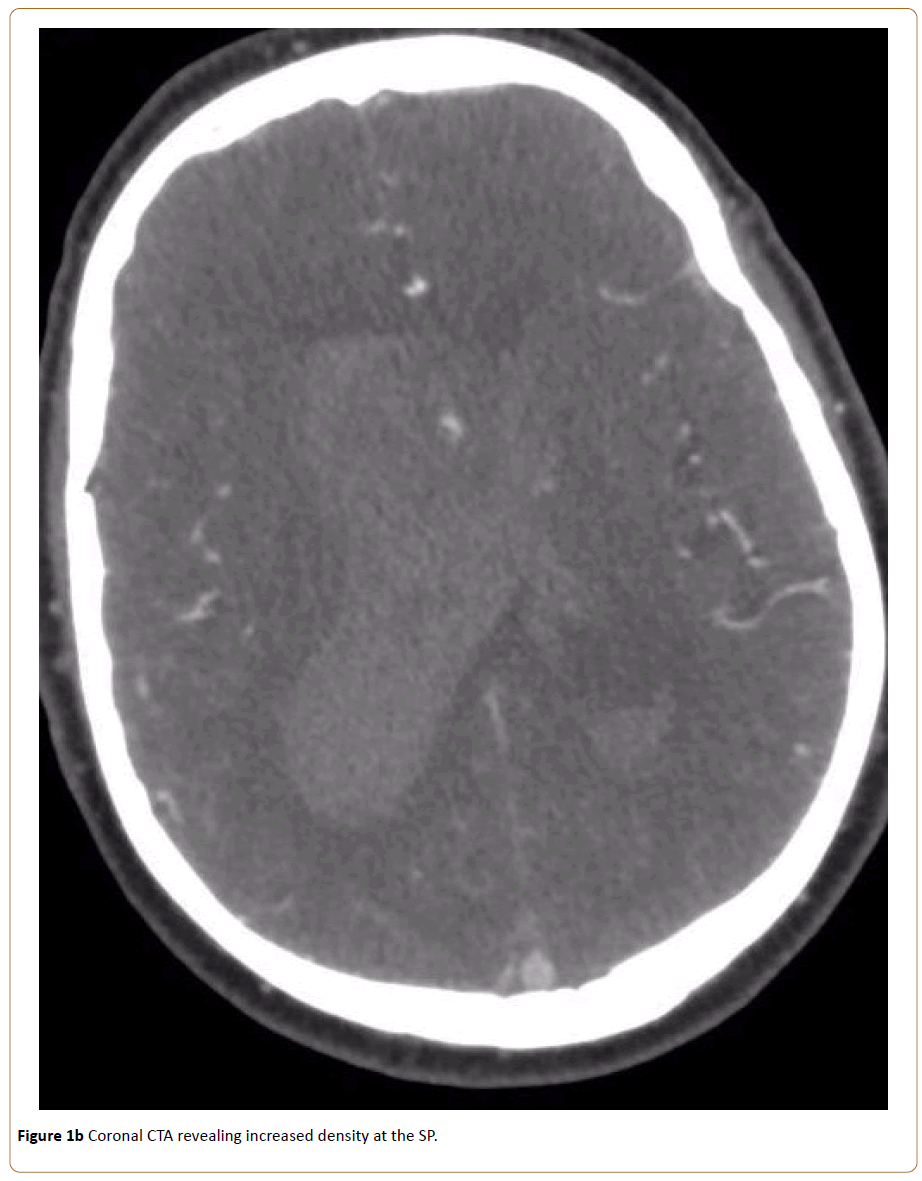
Figure 1b: Coronal CTA revealing increased density at the SP.
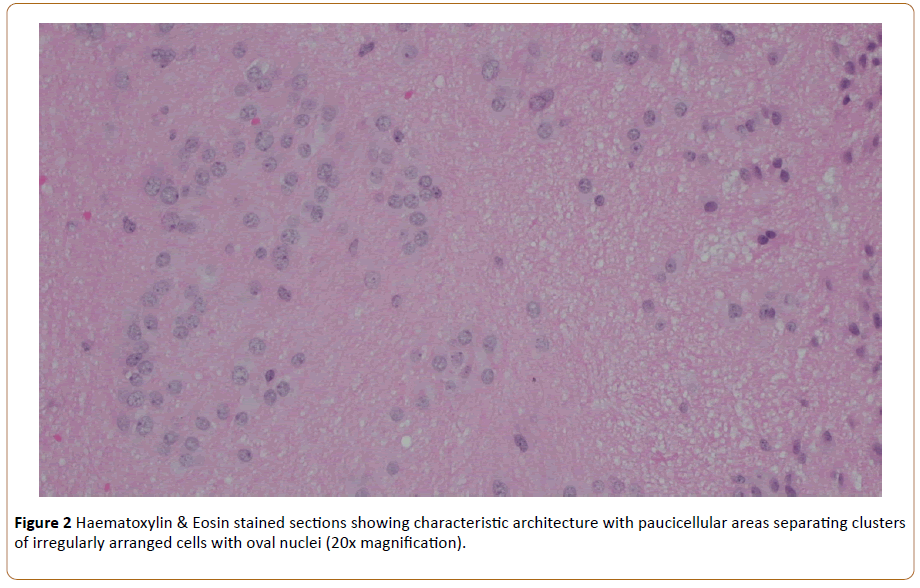
A left frontal external ventricular drain was placed. The following week the patient underwent a stereotactic fronto-parietal craniotomy and sub-total resection via an interhemispheric approach. Intraoperative frozen specimens identified an ependymal tumour. Formal histological analysis was compatible with a WHO Grade I SE, confirmed on specialist neuropathological review (Figure 2).
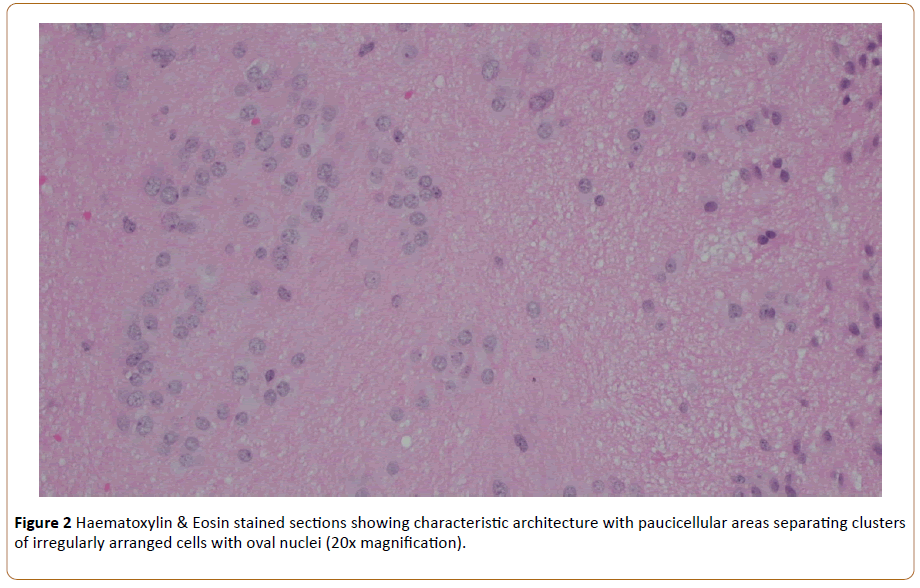
Figure 2: Haematoxylin & Eosin stained sections showing characteristic architecture with paucicellular areas separating clusters of irregularly arranged cells with oval nuclei (20x magnification).
Postoperatively the patient showed gradual neurological recovery. On day 32, he underwent insertion of a percutaneous endoscopic gastrostomy tube for maintenance of adequate nutritional intake. On day 50, the patient was discharged to rehabilitation. Whilst at rehabilitation, he succumbed to a hospital-acquired pneumonia with subsequent decline and passed away peacefully three months after initial presentation.
Discussion
SEs are infrequent glial neoplasms typically described as being benign [3]. Demographically, symptomatic lesions most commonly manifest in middle-aged and elderly males however they have been described in all decades of life [1-7]. SE’s are prevalently located within the fourth ventricle, followed in order by the lateral ventricles, SP, third ventricle and spinal cord [3,5]. Synchronous or metachronous lesions are extremely rare; to the author’s knowledge this is the first reported case of a synchronous SE and meningioma.
Spontaneous haemorrhage subependymomas is unusual due to their hypovascularity [5]. Of the thirteen cases of SE haemorrhages identified in the literature (Table 1), only two prior cases involved the SP [4,8]. Moreover, these had not been diagnosed prior to the acute event and interestingly, cases had presented in considerably younger individuals (Table 1). A definitive mechanism of intratumoural bleeding has yet to be elucidated; However, stretching of adjacent ependymal and subependymal veins secondary to tumour growth is implicated [5]. This patient had a significantly increased risk due to arterial hypertension, therapeutic INR and antiplatelet therapy.
| Author |
Gender |
Age |
Predisposing Factor |
Presentation |
Haemorrhage |
Tumour Location |
Treatment |
Outcome |
| Scheithauer |
F |
81 |
Unknown |
Decreased conscious state |
Tumoural |
Left Ventricle |
Nil operative |
Haemorrhage, death |
| Changaris et al. |
M |
16 |
No |
SAH |
Tumoural, subarachnoid |
Right atrium, occipital horn |
Parieto-occipital transcortical, total resection |
Homonymous hemianopia, survived |
| Seiki et al. |
F |
33 |
No |
SAH |
Ventricular, subarachnoid |
Left atrium |
Parieto-occipital transcortical, total resection |
Unknown |
| Yamasaki et al. |
F |
54 |
No |
Chronic headache |
Tumoural |
Left frontal horn |
Transcallosal, total resection |
Transient memory impairment, survived |
| Marra et al. |
F |
42 |
Unknown |
SAH |
Ventricular, subarachnoid |
Right frontal horn |
Transcallosal, total resection |
Nil deficits, survived |
| DiLorenzo et al. |
M |
46 |
HTN |
SAH |
Ventricular, subarachnoid |
Septum Pellucidum |
Frontal Transcallosal, total resection |
Nil deficits, survived |
| Lindboe et al. |
M |
63 |
Highly vascular tumour |
Confusion, memory loss, urinary incontinence |
Tumoural |
Left frontal horn |
Transcallosal, partial resection |
Haemorrhage, death |
| Viale (awaiting PDF) |
M |
52 |
Unknown |
Decreased conscious state |
Tumoural |
Right frontal horn |
approach, total resection |
Nil deficits, survived |
| Furie et al. |
M |
46 |
Unknown |
Chronic headache |
Tumoural |
Right atrium |
|
Unknown |
| Carrasco et al. |
M |
71 |
HTN,
anticoagulation |
Decreased conscious state |
Tumoural, ventricular |
Left frontal horn |
Frontal transcallosal |
Permanent memory impairment, survived |
| Akamatsu et al. |
M |
32 |
No |
Headache, decreased conscious state |
Ventricular |
Septum Pellucidum |
Anterior TC, IH. Total resection |
Nil deficits, survived |
| Landriel et al. |
M |
32 |
No |
Headache |
Cisterna Magna |
Fourth Ventricle, spinal canal |
Midline suboccipital, velotonsillar. Total resection |
Nil deficits, survived |
| Present Case |
M |
76 |
HTN,
anticoagulation |
Headache, decreased conscious state |
Septum pellucidum |
Right lateral ventricle |
Fronto-parietal, IH. Partial resection |
Decreased conscious state, urinary incontinence, death |
Table 1: Summary of previous cases of subependymoma (SEs) presenting with intratumoral haemmorhage. TC=Transcallosal, IH=interhemispheric, SAH=subarachnoid haemorrhage.
The crucial features of this case are thus highlighted; a rare lesion in an extraordinary location with the unexpected complication of haemorrhage. This raises several compelling issues. Whilst it is rare for SE's to bleed, it is an understood possibility and in lesions of the SP there is no tamponade effect from surrounding brain parenchyma, leading to catastrophic sequelae. Antiplatelet and anticoagulant therapies are commonly encountered in neurosurgical patients and questions our level of caution when encountering such patients with SE’s. Traditionally considered clinically benign, should we in fact be far more cautious in our monitoring and management within the context of anticoagulation and antiplatelet therapies?
Secondly, was earlier resection warranted? It is the view of Cunha and colleagues that surgical management is necessary in symptomatic patients, a notion supported by multiple groups [3,6]. The behaviour of SE’s to expand into rather than infiltrate surrounding brain parenchyma and their low growth rate is thought to be optimal for curative resection [3,4]. In retrospect, a conservative approach to this asymptomatic elderly patient with multiple co-morbidities was appropriate. Evidently, a patient-specific and balanced approach is required.
In this case, investigations and subsequent management were influenced strongly by the prior knowledge of the SP lesion. Hypertensive haemorrhages can be similarly located, are far more common, and are managed conservatively. The question is raised whether more aggressive measures should be employed in order to identify an underlying cause of ictus in similarly-aged patients with no known history. This is a complex question that deserves consideration, keeping in mind the relative benefit, yield and cost.
Conclusion
In conclusion, intraventricular haemorrhages secondary to subependymomas are extremely rare. Our patient represents only the third reported case with haemorrhage into a septum pellucidum lesion, and the first reported case of a co-existent meningiothelial meningioma. Investigation and management should be case-specific however further research is required, particularly in older patients with multiple comorbidities.
References
- Lindboe CF, Stolt-Nielsen A, Dale LG (1992) Hemorrhage in a highly vascularized subependymoma of the septum pellucidum: case report. Neurosurgery 31: 741-745.
- Scheithauer BW (1978) Symptomatic subependymoma. J Neurosurg 49: 689-696.
- Yamasaki T, Kikuchi H, Higashi T, Yamabe H, Moritake K (1990) Two surgically cured cases of subependymoma with emphasis on magnetic resonance imaging. Surg Neurol 33: 329-335.
- Akamatsu Y, Utsunomiya A, Suzuki S, Endo T, Suzuki I, et al. (2010) Subependymoma in the lateral ventricle manifesting as intraventricular hemorrhage. Neurol Med Chir (Tokyo) 50: 1020-1023.
- Carrasco R, Pascual JM, Navas M, Fraga J, Manzanares-Soler R, et al. (2010) Spontaneous acute hemorrhage within a subependymoma of the lateral ventricle: successful emergent surgical removal through a frontal transcortical approach. Neurocirugía 21: 478-483.
- Cunha AM, Brito ACG, de Almeida Lima G, de Souza LA, Simões EL, et al. (2012) Cerebellopontine angle subependymoma without fourth ventricle extension: An uncommon tumor in a rare location: Cerebellopontine angle subependymoma. Neuropathology 32: 164-170.
- Furie DM, Provenzale JM (1995) Supratentorial ependymomas and subependymomas: CT and MR appearance. J Comput Assist Tomogr 19: 518-526.
- DiLorenzo N, Rizzo A, Ciappetta P (1991) Subependymoma of the septum pellucidum presenting as subarachnoid hemorrhage. Neurochirurgia (Stuttg) 34: 125-126.