- (2009) Volume 10, Issue 1
Marco Massani, Alessio Bridda, Ezio Caratozzolo, Luca Bonariol, Michele Antoniutti, Nicolò Bassi
Fourth Surgical Division, Regional Hospital "Ca' Foncello". Treviso, Italy
Received September 22nd, 2008 - Accepted November 26th, 2008
Context Hemosuccus pancreaticus is a rare cause of upper chronic and intermittent gastrointestinal hemorrhage which cannot be easily detected by endoscopy. It is usually due to the rupture of a visceral aneurysm into the main pancreatic duct; splenic artery pseudoaneurysm associated with chronic pancreatitis represents the leading cause of this condition. The diagnosis is based on direct visualization of the hemorrhage through the main pancreatic duct at angiography. Given its rarity, difficulties in determining the source of bleeding can result in delayed treatment. Case report We present a rare case of true splenic artery aneurysm fistulized in the main pancreatic duct and misdiagnosed as a bleeding pancreatic pseudocyst on preoperative examination which included CT and MRCP. Conclusions Our experience confirms that the diagnosis of bleeding from the main pancreatic duct is very difficult. It requires careful and repeated evaluation by a team of specialists.
Aneurysm; Gastrointestinal Hemorrhage; Pancreatic Pseudocyst; Pancreatic Ducts; Pancreatic Fistula; Splenic Diseases
Hemosuccus pancreaticus is a rare cause of upper chronic and intermittent gastrointestinal hemorrhage which cannot be easily detected by endoscopy. It is usually due to the rupture of a visceral aneurysm into the main pancreatic duct; splenic artery pseudoaneurysm associated with chronic pancreatitis represents the leading cause of this condition. The diagnosis is based on direct visualization of the hemorrhage through the main pancreatic duct at angiography. Given its rarity, difficulties in determining the source of bleeding can result in delayed treatment.
A 53-year-old man was referred to our clinic for evaluation of melena following recurrent episodes of acute abdominal pain. During the 6 months prior to admission, the patient had complained of recurrent episodes of epigastric pain irradiating to the back and resolving spontaneously. His medical and surgical history included an appendectomy for acute gangrenous appendicitis and an untreated hiatal hernia. He denied any history of drug and alcohol abuse.
He had had two previous admissions with three emergent upper gastrointestinal endoscopies, performed in the Gastroenterology Unit of our hospital, revealing a hiatal hernia and fresh blood in the second part of the duodenum and in the anterior wall of the stomach. During one of these procedures, small nonbleeding angiodysplasias were treated with argon plasma coagulation. Colonoscopy was unremarkable. On physical examination, the patient was pale and diaphoretic, but asymptomatic and hemodynamically stable. No signs of chronic hepatopathy or splenomegaly were noted. A blood count and chemistry tests showed mild anemia (hemoglobin 8.3 g/dL; reference range: 12-16 g/dL) and high serum lipase level (387 U/L; reference range: 13-60 U/L). Because of persistent abdominal pain and melanotic stools, the patient underwent a scintigraphic bleeding study with 99mTc-tagged red blood cells. The scan showed only a slight accumulation of radiotracer in the right lower quadrant of the abdomen in late images (at 24 and 27 hours). A magnetic resonance cholangiopancreatography (MRCP) revealed an 8.2 cm pseudocystic lesion of the pancreatic body with a thickened wall and bloody content. A contrast-enhanced MRI showed an ectasic splenic artery eroded into the pseudocyst and a dilated main pancreatic duct communicating with the pseudocyst; the celiac trunk was also dilated. These findings were confirmed at a contrast-enhanced CT scan (Figures 1 and 2).
At laparotomy, a large aneurysm of the proximal and middle splenic artery, firmly adherent to the body of the pancreas was identified. After mobilization of the spleen and pancreas, ligation of the splenic artery at the origin where the vessel was normal, and ligation of the splenic vein, a distal splenopancreatectomy was performed. Examination of the open specimen showed an ulcerated and calcific 7 cm splenic aneurysm. Histological examination revealed a true aneurysm associated with chronic pancreatitis and hyperplasia of the isles of Langerhans. The post-operative course was unremarkable, except for a hyperglycemic episode treated with insulin.
Hemosuccus pancreaticus, defined as bleeding from the papilla of Vater via the pancreatic duct, is a rare and challenging cause of acute and intermittent upper gastrointestinal bleeding predominantly affecting men (sex ratio 7:1). Also known as pseudohemobilia and Wirsungorrhaghia, it was first described in 1931 by Lower and Farrel who reported a primary splenic aneurysm ruptured into the main pancreatic duct [1] while the name hemosuccus pancreaticus was given by Sandblom in 1970 [2]. Hemosuccus pancreaticus may be differentiated from hemorrhage due to pancreatic abscesses or stones eroding vessels in the wall of the gastrointestinal tract [2].
Gastrointestinal bleeding through the pancreatic duct can be divided into 2 groups: 1) hemorrhage of strictly pancreatic origin; this accounts for about 60-80% of cases [3] and is usually due to a pancreatic pseudocyst or a peripancreatic pseudoaneurysm associated with acute relapsing or chronic pancreatitis [4]; pancreatic arterovenous malformations and pressure ulcers in the ductal wall due to pancreaticolithiasis are anecdotal reported causes of hemosuccus pancreaticus [5, 6]; 2) hemorrhage of extra pancreatic origin; this is rare and usually due to a splenic aneurysm of malformative (fibromuscular dysplasia), atherosclerotic, traumatic or mycotic origin. Mean age at onset is about 60 years versus 50 years for the pseudoaneurysm-related forms [7]. Intrapancreatic duplication cysts of gastric or duodenal origin, ulcerating into the main pancreatic duct, are another reported cause of hemosuccus pancreaticus [4].
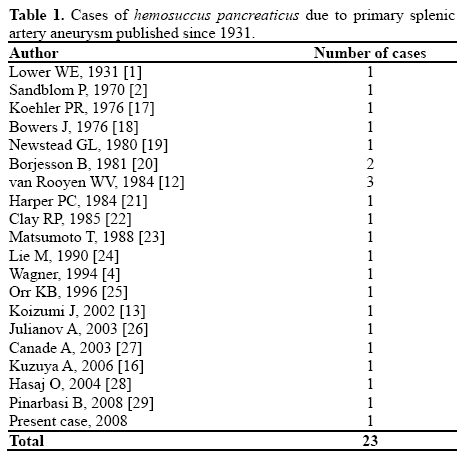
The splenic artery is the third most common site for aneurysms, after the abdominal aorta and iliac arteries, and the most common visceral site of arterial aneurysms [3]. True splenic artery aneurysms account for about 60% of visceral artery aneurysms and occur mainly in women (male-to-female ratio 1:4), pregnancy being a known risk factor for rupture [5]. They are generally located in the middle and distal third of the artery, and can be singular or multiple; a diffuse enlargement of the vessel is the typical feature, but a saccular form can be seen in mycotic aneurysms [8]. Usually asymptomatic, a primary splenic artery aneurysm rarely ruptures into a normal pancreatic duct. This is the 23rd case of hemosuccus pancreaticus caused by a primary splenic aneurysm reported in the English-language literature since 1970 (Table 1).
Intermittent gastrointestinal bleeding of unknown origin is often a diagnostic problem. It can be very difficult to make the diagnosis of hemosuccus pancreaticus, even with a known diagnosis of pancreatitis, because of its rarity and anatomical location, not being readily accessible by endoscopy. Intermittent colic epigastric pain followed by hematochezia, melena or hematemesis within 30-40 minutes is the characteristic finding, reported to be very specific and nearly pathognomonic [9]. The pain and its crescendo-decrescendo course result from increased intraductal pressure due to blood in the pancreatic duct and from ductal obstruction due to clot formation [9, 10]. Mild pancreatitis due to chronic intermittent distension of the main pancreatic duct by clots can sometimes be seen; it was referred to as “hemoductal pancreatitis” by Longmire and Rose in 1973 [11]. Other clinical signs and symptoms reported less frequently are palpable pulsating mass, weight loss and vomiting.
Endoscopy represents the first diagnostic step in patients with upper gastrointestinal bleeding. Although it is essential to rule out other causes of bleeding, it rarely identifies blood exiting the ampulla of Vater [12]. In all patients with active upper gastrointestinal bleeding and a non-diagnostic endoscopy, an early angiography should be carried out.
Angiography is the gold standard for the demonstration of the fistulized aneurysmatic vessel; however, to demonstrate extravasations through the main pancreatic duct, the exam should be performed while the patient is experiencing pain. The discovery of splenic artery dilation without extravasations of blood leads to clinical suspicion but not to a definitive diagnosis.
Although the identification of an aneurysm or pseudoaneurysm is classically based on angiography, in hemodynamically stable patients the aneurysm can invariably be demonstrated on US, contrast-enhanced CT scan and MRI. Moreover US, CT and, in particular, MRI are more accurate in sizing the aneurysm and can show other pancreatic or endoabdominal causes of bleeding [4].
MRI and MR angiography have their own added advantages over a CT scan of multiplanner capacity, such as radiation and angiography-like image reconstruction. Koizumi et al. [13] reported a case of hemosuccus pancreaticus due to primary splenic aneurysm in which MRI successfully identified communication between the aneurysm and the main pancreatic duct. However, in our case, MRI was not useful for the diagnosis, as in the case previously reported by Toyoki et al. [14].
Hemosuccus pancreaticus due to true or false splenic aneurysms can be treated surgically or by interventional radiological means, depending on the underlyng disorders.
Surgical options for splenic pseudoaneurysm include proximal arterial ligation, distal pancreatectomy and splenectomy, [4] although simple exclusion through ligation can not eliminate the risk of late re-bleeding because of the presence of a diseased pancreas which may be the source of the recurrent pancreatitis.
Surgical treatment for a primary splenic artery aneurysm has changed over the past decade and spleen conservation should be attempted in order to prevent post-splenectomy sepsis. In particular, treatment depends on aneurysmal location in the splenic artery. Aneurysmectomy and splenectomy are the standard treatments for distal aneurysms involving the splenic hilum. Conversely, proximal and middle aneurysms can be managed by excision of the aneurysm with or without reconstruction or by simple ligation; proximal and distal ligation of the artery through an open or laparoscopic approach has become the preferred technique for primary uncomplicated aneurysms [15]. In this case, even if the splenic artery is not reconstructed, backflow through the short gastric vessels and the right gastroepiploic artery prevents infarction of the spleen.
When hemoductal pancreatitis complicates a primary splenic aneurysm fistulized into the main pancreatic duct, distinguishing a true from a secondary aneurysm can be difficult. Moreover, the proximal and distal ligation of the aneurysm does not seem to be an effective treatment due to the persistent communication between the aneurysm and the pancreatic duct. In this case, distal pancreatic resection should represent the only surgical option.
Interventional radiology is the primary choice of treatment for high risk patients or for hemodynamically unstable patients who undergo angiography. Endovascular treatment options include coil or gel foam embolization, detachable balloon occlusion and stent graft. As for surgical options, the choice of the endovascular technique depends on the location of the aneurysm in the artery. Coil embolization has been used extensively for distal splenic aneurysms while stent grafts, excluding the aneurysmatic tract, are more suitable for proximal primary or secondary aneurysms because of the rigidity of the vascular system. However, the angle between the celiac trunk and the aorta, and the tortuosity of the splenic artery could make these procedures extremely difficult or not feasible [8]. Moreover, they cannot be used for giant aneurysms and have the possibility of recurrence of the aneurysm and complications such as spleen infarction or abscess.
Endovascular procedures are reported to be effective in the treatment of splenic aneurysms fistulized in the main pancreatic duct, and some authors claim interventional radiology as the procedure of choice for these cases, considering surgery an alternative treatment when radiology is not successful [14, 16]. However, in our opinion, coil embolization or stent grafting can be considered effective techniques for controlling hemodynamically unstable conditions, but surgical resection is the only treatment preventing recurrent bleeding in both true and false aneurysms. The integration of interventional radiology and surgery should be obtained in hemodynamically unstable patients; preoperative transcatheter embolization during angiography might provide an opportunity to gain temporary control over the bleeding vessel and thus provide time for planning and performing the definitive surgical treatment of a high-risk patient under optimum clinical conditions.
Our experience confirmed the difficulty of correctly diagnosing bleeding from the main pancreatic duct. Careful and repeated observations should be carried out in order to reveal the source of obscure and persistent upper gastrointestinal tract bleeding. The role of angiography both for diagnosis and treatment is fundamental, and surgery should be considered only when radiological treatment fails. Pancreatoscopy, although difficult, and intraoperative ultrasonography are of great benefit in locating the precise site of bleeding in the main pancreatic duct
The authors have no potential conflicts of interest