Case Report - (2017) Volume 18, Issue 2
Departments of 1Medical Gastroenterology, 2Hepato-Pancreatico-Biliary Surgery, 3Surgical Gastroenterology, and 4Radiodiagnosis and Interventional Radiology, GEM Hospital and research centre Pvt. Ltd, Coimbatore, India
Received December 05th, 2016 - Accepted January 06th, 2017
A fifteen-year-old male patient, known case of chronic pancreatitis diagnosed as obscure gastrointestinal bleed in previous admission, readmitted for melena and upper abdominal pain since 2 days. Blood investigations revealed severe anemia with acute on chronic pancreatitis. Upper Gastro-Intestinal endoscopy revealed altered bood in stomach, adherent blood clot in ampulla. Thorough saline wash removed the clot, and blood stained bile flow was seen. This suspected the presence of hemosuccus pancreaticus, and proceeded with computed tomography abdomen. Computed tomography abdomen revealed presence of pseudoaneurysm in ventral division of inferior pancreaticoduodenal artery. Selective angiography confirmed the finding and coil angioembolization was done. No rebleeding during hospital stay.
Ampulla of Vater; Pancreas; Pancreatitis; Chronic
CT computed tomography; GI gastro-intestinal; HP hemosuccus pancreaticus
Hemosuccus pancreaticus (HP) is a rare and potentially life threatening upper gastrointestinal (GI) bleed, defined as bleeding from ampulla of Vater through pancreatic duct. It was first described in 1931 by Lower and Farrel who reported a primary spleenic aneurysm rupture into the main pancreatic duct while the name hemosuccus pancreaticus was given by Sandblom in 1970. It is usually occurs due to the rupture of a visceral aneurysm into the main pancreatic duct; splenic artery pseudoaneurysm associated with chronic pancreatitis represents the leading cause of this condition [1, 2]. HP has been estimated to occur in about one in 1,500 cases of GI bleeding [3].
A Fifteen-year-old-male patient who is a known case of chronic pancreatitis without endocrine and exocrine insufficiency, admitted for melena with upper abdominal pain since 2 days. Patient had melena 2 weeks back also for which he was hospitalised in our institution and evaluated with upper GI endoscopy, colonoscopy and CT angiogram which were normal and considered it as obscured overt GI bleed. There was no history of NSAID intake. Clinical examination revealed pallor, tachycardia and severe epigastric tenderness. Other systemic examination nothing contributory. Blood investigations showed haemoglobin of 7 gms/dL, normal leucocyte and platelet count, significantly elevated serum amylase (657 U/L) and lipase (786 U/L), normal liver and renal function test. Peripheral smear showed microcytic and hypochromic anemia. Transabdominal ultrasonography revealed acute on chronic pancreatitis with pancreatic calcifications. Etiological workup done for chronic pancreatitis showed normal triglycerides levels, normal calcium and parathyroid harmone levels. There was no pancreatic divisum on MRCP and IgG4 levels were normal. Upper GI endoscopy (Figure 1) revealed altered blood in stomach with adherent clot in the ampulla. After thorough saline wash, ampulla showed blood stained bile and hemosuccus pancreaticus was suspected. CT abdomen showed evidence of chronic pancreatitis with pseudo-aneurysm (7x6 mm) in the ventral division of inferior pancreaticoduodenal artery (Figure 2). Later patient underwent angiography through right femoral approach, superior mesenteric artery was cannulated with 5F Sim 1 catheter and selective angiography confirmed a pseudoaneurysm in the ventral branch of inferior pancreaticoduodenal artery supplying mid body of pancrease (Figure 3). Selective angioembolization done at neck of pseudoaneurysm (Figure 4). Check angiogram revealed no filling of pseudoaneurysm.
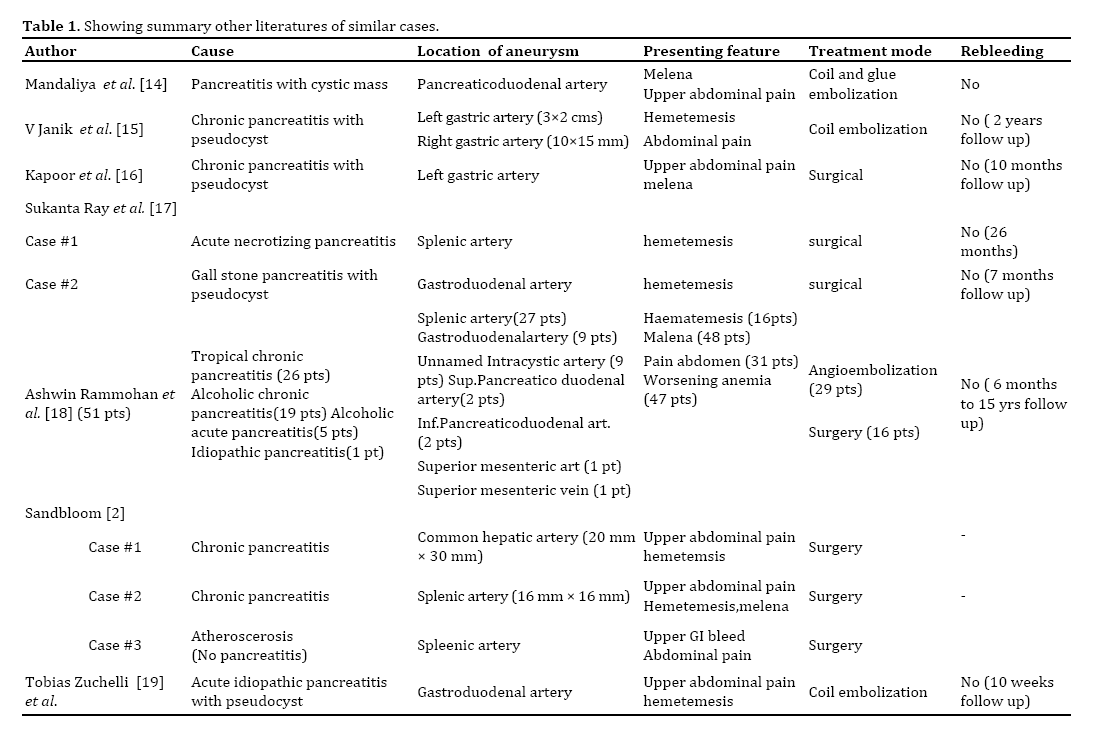
This Fifteen-year-old boy, known case of chronic pancreatitis who was previously admitted for evaluation of melena and considered it as obscure overt GI bleed. Subsequently at present admission he was diagnosed as HP due to psuedoanuerysm in inferior pancreaticoduodenal artery. Upper GI endoscopy revealing adherent clot over the ampulla of Vater and blood stained bile flow gave us clue towards the diagnosis. This clinical scenario emphasises the intermittent nature of bleed and importance of examining the ampulla for upper GI bleed evaluation in pancreatitis patients. During a bout of pancreatitis, pancreatic proteolytic enzymes digest the arterial wall causing pseudoaneurysm which may bleed into pancreatic duct of Wirsung, raising the intraductal pressure causing to severe abdominal pain. As the duct is decompressed through ampulla, patient will have upper GI bleed and relief in pain which explains the crescendodecrescendo type of abdominal pain. Ductal blockage also causes increase in serum amylase and lipase levels. This logical analysis of pathogenesis explains the triad of abdominal pain (crescendo-decrescendo nature), elevated serum pancreatic enzymes and GI bleed which is seen in HP patients [4, 5]. The most common cause for pseudoaneurysm is acute or chronic pancreatitis [6]. Other frequent causes are trauma [7], rupture of true aneurysm [8], pancreatic tumors [9], arteriovenous malformations [10]. The splenic artery is the most common artery involved (60-65%) followed in decreasing order of frequency by gastroduodenal (20-25%), pancreaticoduodenal (10- 15%), hepatic (5-10%) and left gastric arteries (2-5%) [11, 12, 13, 14, 15, 16]. Table 1 gives details about other similar cases . These data highlights the fact that inferior pancreaticoduodenal artery is less commonly involved which is involved in the present case. Ultimately, angiography is the diagnostic reference standard, identifies the causative artery, delineates the anatomy and allows for therapeutic intervention. The sensitivity of angiography is usually greater than 90% [8, 13, 15, 17].There are two potential therapeutic approaches: interventional radiological procedures and surgery. If the source of hemorrhage is found by angiography then interventional radiographic procedures are the first choice for initial management with immediate good results in 79-100% of the cases and an overall success rate of 67%. The techniques for intervention include embolization via prosthetic material, balloon tamponade and stent placement. Coil embolization is the most frequently described technique which is done our patient also. It stimulates thrombus formation in the pseudoaneurysm [17, 18]. Surgical treatment is indicated when there is uncontrolled bleeding, persistent shock, failure of embolization, rebleeding after embolization, or when initial angiography shows no abnormal findings. The various surgical procedures include distal pancreatectomy and splenectomy, central pancreatectomy, intracystic ligation of the blood vessel, aneurysm ligation and bypass graft. Most surgical procedures have shown success rates of 70-85%, at the same time operative mortality rates of 10-50% have been reported in the literature. The rate of rebleeding after surgery is 0-5% [17, 19, 20, 21].
HP is an arterial bleed, often life threatening if diagnosis is delayed. This case highlights the importance of examining major papilla for evidence of bleed in patients of pancreatitis presenting with upper GI bleed, which gives us clue for early diagnosis and intervention.
Authors declare no conflict of interests for this article.