Keywords
Paraquat dichloride; Toxicity; Vitamin C; Garlic; Liver function; Oxidative stress
Introduction
Paraquat dichloride (PQ) is a non-selective contact herbicide for broadleaf weed control. It is used widely in modern agricultural practice worldwide and is emerging rapidly in Nigerian’s agricultural industry. Paraquat is not only toxic to plants but adversely affect human and farm animals [1,2] by accumulating in the lungs, liver, kidneys and heart. Animal exposure occurs by accidental or intentional swallowing, or through damaged skin or inhalation. Studies on paraquat toxicity have shown that chronic exposure can lead to lung and liver damage, kidney failure, and Parkinsonian lesions in addition to fibrosis [3,4].
Paraquat toxicity occurs through excess production of free radicals which results in oxidative stress and damage [5,6]. This toxicity emanates from the redox cycle that generates superoxide radical (O2•–) that cascades to the production of hydrogen peroxide (H2O2) and hydroxyl radical (HO–). Oxidative stress can damage molecular structures, cell function, and is implicated in numerous pathological situations. However, adverse impact of free radicals can be repaired by the body's natural defense system and/or antioxidants consumed in the diet. Garlic, glutathione and vitamin C are food and food components that have antioxidant potentials
Garlic (Allium sativum) is an important food flavour and is used in herbal remedies [7]. Garlic is a good source of selenium, iodine, arginine, Vitamin C and B6 [8], allicin, Sallylcysteine, and allylcysteine. Allicin is an organosulfur compound, unstable and quickly changes into a series of other sulfur-containing compounds such as Diallyl sulfide (DAS), diallyl trisulfide (DAT), and DAS, disulfide derivatives (DADS) etc. [9]. Allyl disulfide protects cells against microsomal lipid peroxidation, allylcysteine are important hydroxyl radical (•OH), and peroxyl radical (ROO•) scavengers [10], and allicin can scavenge hydroxyl radicals and prevent lipid peroxidation. Garlic organo sulfides components (DAS, DADS and DAT) were shown to play a differential modulatory role on the GSH related antioxidant system [11]. Futher more, garlic organo sulfides DAS, DADS, DPS (dipropyl sulfide) and DPDS (dipropyl disulfide) induces the expression of NAD(P)H [12].
Glutathione (GSH) is an antioxidant with capacity to prevent oxidative damage to vital cellular components by free radicals, peroxides, lipid peroxides, and heavy metals [13,14]. In reduced state, the thiol group of cysteine in glutathione can donate a reducing equivalent (H++e−) to other molecules, such as reactive oxygen species to neutralize them. Oxidized glutathione (GSSG) is reduced in the presence of an electron donor (NADPH) by glutathione reductase [15]. Biologically, Vitamin C is an antioxidant and a good reducing agent, that donates electrons to several enzymatic and some non-enzymatic reactions [16,17]. Cellular and extracellular content of glutathione [18] and NADPH-dependent Enzyme mechanisms [19] maintain semi dehydroascorbic acid and dehydroascorbic acid in a reduced state.
The increased use of pesticides for crop production, prevention of unwanted plants and improvement of crop yield has resulted to intolerable deposits of these chemicals in soil, plants and water sources due to indiscriminate use. Pesticide residues find their way into mammals through water consumption and via food chain. Mammalian toxicity of paraquat has been a focal point of research in recent years, because systematic exposure initiates progressive degeneration and potential lethal lesions on mammalian tissues and organs. Therefore, this study determined the hepatotoxicity of paraquat dichloride and ameliorative effect of some nutritional supplements.
Materials and Methods
Experimental design
Thirty-six male Wistar albino rats were housed in metal cages lined with sawdust, in a properly ventilated animal house at 24 ± 3°C in a 12 hour light/dark cycle. During the one week period of acclimatization the rat were allowed free access to water and rat chow. The study was considered and approved by the Ethical committee of Biochemistry Department, Federal University of Technology Owerri, Nigeria and was carried out according to the national and institutional guidelines for protection of human subjects and animal welfare [20]. After acclimatization, the rats (140-160 g) were divided into six groups of six rats each in metal cages;
Normal control (NC) received 0.9% NaCl saline solution only. Paraquat control (PQ), Vitamin C (VC), Garlic (GC), Glutathione (GS) and Synergy (SYN) groups received 1.5 mg/kg of body weight of paraquat dichloride intraperitoneally each alternate day. All groups (except NC) was treated orally with 40 mg/kg body weight of Vitamin C, Garlic and Glutathione supplements daily respectively while SYN group received 40 mg/kg body weight of Vitamin C, Glutathione and Garlic (VGG) treatments in the ratio of 1:1:1 every day for two weeks. All rats were allowed free access to rat chow and clean water and no death was recorded throughout.
Sample collection
Blood samples were collected by ocular puncture into test tubes and allowed to stand for 30 min to clot and then centrifuged at 3000 × g for 15 min to obtain serum. Serum samples were stored in a refrigerator at 4°C until needed for biochemical analyses. After sample collection the rats were sacrificed and liver was excised rinsed thoroughly in ice cold saline. Liver sample was homogenized in KCl buffer (1.15 %) in EDTA at pH 7.4 and centrifuged for 20 min at 250 × g. Aliquots of supernatant from the homogenate was used to assay oxidative stress parameters. Some portions of liver sample were stored in 0.3 % formaldehyde for histopathology.
Determination of liver function parameters
Aspartate aminotransferase (AST) and Alanine aminotransferase (ALT) activities were assayed by the method as described by Reitman and Frankel [21] using commercial kits provided by Bio Merieux France. The method described by Rec [22] was used to determine alkaline phosphatase (ALP) activity using commercial kits provided by Bio Merieux France. The method of Jendrassik and Grof [23] was used to determine total bilirubin. Total protein and albumin were determined as described by Tietz et al. [24] and Doumas et al. [25] respectively.
Determination of liver lipid peroxidation
To measure lipid peroxidation, malondialdehyde (MDA) concentration, the end product of lipid peroxidation was determined. Malondialdehyde was determined by the method described by Wallin et al. [26]. Briefly; four test tubes were setup and into these tubes; 0.1 ml of sample, 0.9 ml of distilled water, 0.5 ml of 25 % trichloroacetic acid (TCA) and 0.5 ml of 17 % TBA in 0.3 % NaOH were pipetted. The setup was incubated at 95°C for 40 minutes and subsequently cooled. Finally, 0.1 ml of 20 % sodium dodecyl sulphate was added and absorbance of the mixture measured at 532 nm and 600 nm against a blank.
Determination of glutathione
The concentration of glutathione was determined by the method described by Raja et al. [27]. Briefly: Protein was separated from the sample by mixing 1 ml sample homogenate with 4 ml of 10 % trichloroacetic acid and centrifuged at 3000 rpm for 10 min. Then 0.01 ml of the supernatant was pipette into a tube containing 2 ml of phosphate buffer (pH 8.4), 0.5 ml of 5, 5-dithiobis (2- nitrobenzoic acid) and 0.4 ml doubled distilled water. The setup was mixed vigorously and absorbance taken at 412 nm in spectrophotometer within 15 min.
Determination of total antioxidant capacity
Total antioxidant activity was estimated by Ferric reducing ability of Plasma (FRAP) method by Benzie and Strain [28]. Briefly: Initially, a working reagent comprising acetate buffer (pH 3.6), ferric chloride and tripyridyltriazine in the ratio of 10:1:1 respectively was prepared. To 60 μl of sample or standard or blank in a clean test tube, 1.8 ml of working reagent was added. The reaction mixture was mixed thoroughly and incubated at 37°C for 10 minutes. The resulting blue coloured solution developed was then read at 593 nm. The blank was treated the same way except that 60 μl of distilled water was added instead of plasma. The standard solution contains 1000 μmol/l of ferrous sulphate.
Histological studies
Samples of liver were fixed with formal saline and subjected to dehydration, clearing (de-alcoholisation), infiltration and embedded in paraffin as described by Okoro [29] with minor modifications. Samples were serially sectioned at an appropriate thickness and stained with hematoxylin and eosin (H&E) [30]. Further, tissue sections were examined with light microscope at a magnification of 100x and 400x.
Statistical analysis
Results were expressed as mean and standard deviation (mean ± standard deviation) and determined for all the parameters. The data were analyzed by one-way analysis of variance (ANOVA) using SPSS program, version 18, followed by Duncan (Multiple Range-test). Values were considered significant at p<0.05.
Results
Liver function enzyme activities
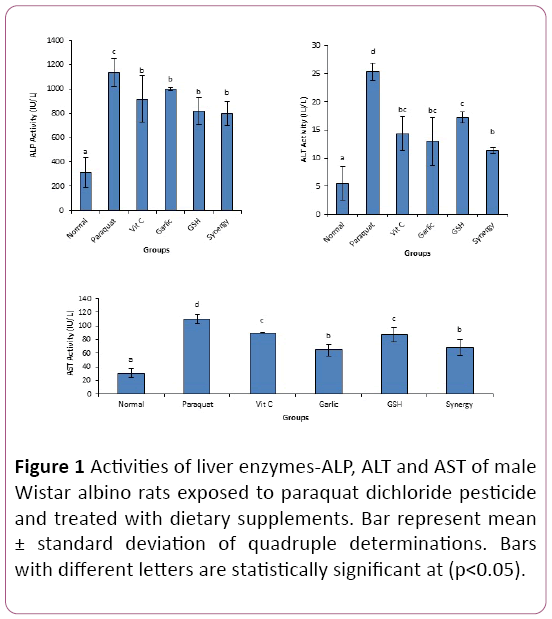
Hepatic toxicity was evaluated by determining serum ALT, AST, and ALP activities as biomarkers of liver damage. This is presented in Figure 1, with paraquat control showing significant increase in the activities of ALP, ALT and AST as compared to Normal control. Furthermore, activities of these liver enzymes reduced significantly in groups exposed to paraquat and treated concomitantly with vitamin C, glutathione, and garlic alone, and combination of vitamin C +glutathione+garlic (VGG) supplements when compared to paraquat control.
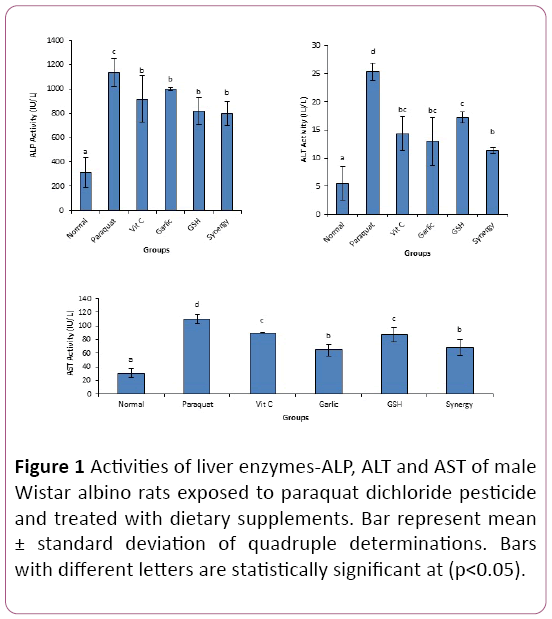
Figure 1: Activities of liver enzymes-ALP, ALT and AST of male Wistar albino rats exposed to paraquat dichloride pesticide and treated with dietary supplements. Bar represent mean ± standard deviation of quadruple determinations. Bars with different letters are statistically significant at (p < 0.05).
Liver protein and bilirubin
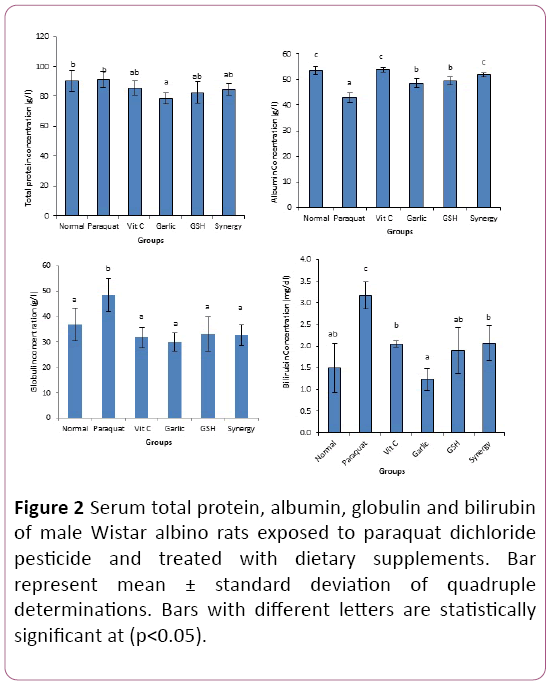
The result of liver protein concentrations Figure 2 showed that, serum total protein in paraquat exposed groups had no significant difference as compared to control.
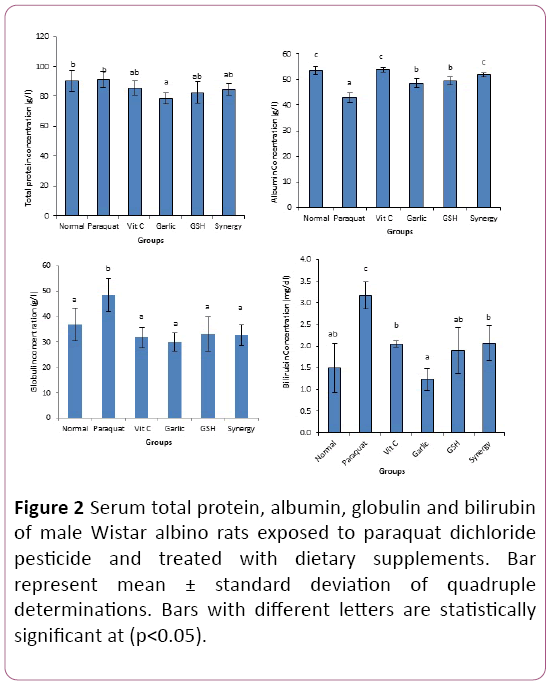
Figure 2: Serum total protein, albumin, globulin and bilirubin of male Wistar albino rats exposed to paraquat dichloride pesticide and treated with dietary supplements. Bar represent mean ± standard deviation of quadruple determinations. Bars with different letters are statistically significant at (p < 0.05).
This implies that, exposure to paraquat did not affect total protein concentrations. However, serum albumin concentration of paraquat control decreased significantly when compared to normal control and supplement treated groups. Furthermore, serum globulin and bilirubin concentration increased significantly in paraquat control as compared to normal control and groups treated concurrently with supplements.
Oxidative stress parameters
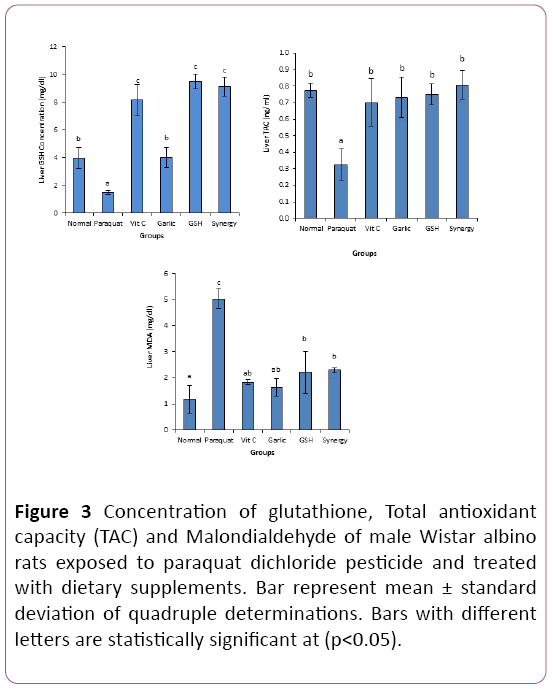
Results of oxidative stress parameters Figure 3 showed significant decrease in total antioxidant capacity and glutathione concentration in paraquat control group compared to normal control and supplement treated groups. However, paraquat control group presented a significantly increased malondialdehyde concentration compared to other groups (Figure 4).
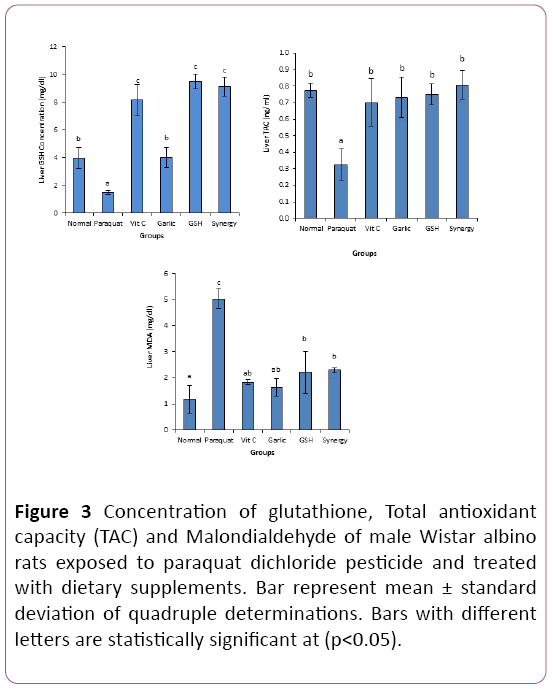
Figure 3: Concentration of glutathione, Total antioxidant capacity (TAC) and Malondialdehyde of male Wistar albino rats exposed to paraquat dichloride pesticide and treated with dietary supplements. Bar represent mean ± standard deviation of quadruple determinations. Bars with different letters are statistically significant at (p < 0.05).
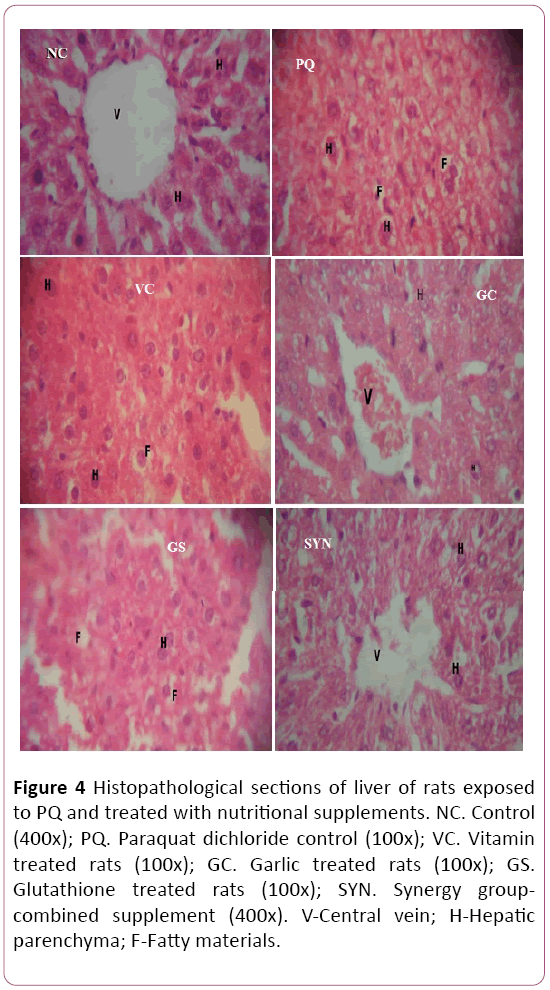
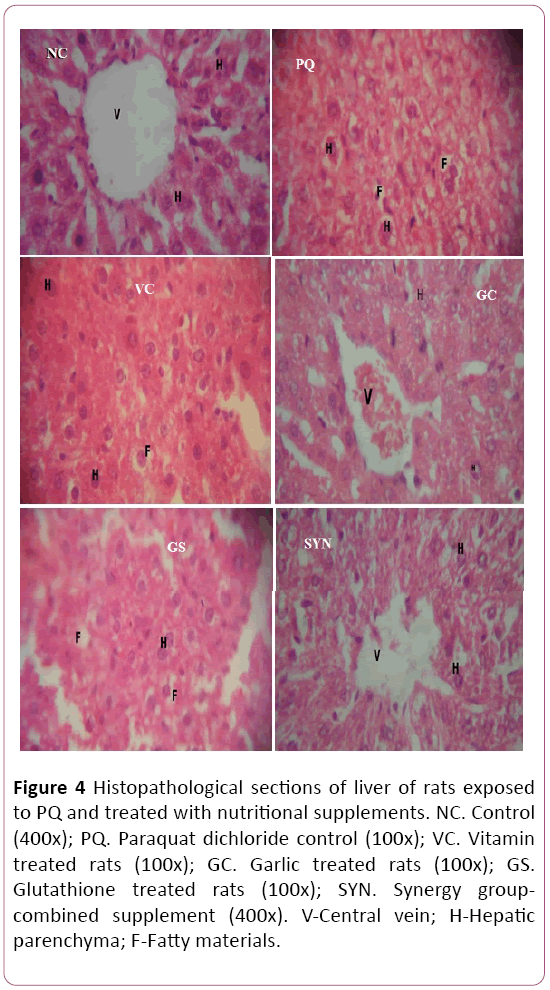
Figure 4: Histopathological sections of liver of rats exposed to PQ and treated with nutritional supplements. NC. Control (400x); PQ. Paraquat dichloride control (100x); VC. Vitamin treated rats (100x); GC. Garlic treated rats (100x); GS. Glutathione treated rats (100x); SYN. Synergy groupcombined supplement (400x). V-Central vein; H-Hepatic parenchyma; F-Fatty materials.
Liver histology
Histopathology evaluation of liver section of Paraquat dichloride control (PQ) showed liver parenchyma in which hepatocytes were surrounded by fatty materials and extensive vacuolations and some hepatocytes appeared hypertrophic. However, liver sections of Normal control showed liver tissue with normal central vein and hepatocytes. Furthermore, liver sections of groups treated with nutritional supplements showed varying changes: VC-Liver section shows liver tissue consisting of hepatocytes in which some are surrounded with fatty materials with vacuolations and hypertrophy of some hepatocytes; GC-Liver section shows liver tissue with congested central vein and hepatocytes appearing normal; GSLiver section shows liver parenchyma consisting of hepatocytes that show hyperplasia with a few hepatocytes that are surrounded by fatty materials and few vacuolations; SYN-Liver section shows liver tissue with normal central vein and hepatocytes.
Discussion
Paraquat dichloride is used strictly by licensed applicators in developed countries due to its toxicity [31], but in developing countries like Nigeria, Guatemala etc, it is not listed as a hazardous chemical and may be used by anyone that can afford it [32]. When compared to most pesticides, paraquat is extremely toxic to animal, especially humans and this has resulted to increased fatality rates due to little or no strategies to manage paraquat poisoning. It is on this premise that this study was conceptualized to determine ameliorative strategy to paraquat poisoning using nutritional supplements. Biochemical and histological parameters of experimental animals were adopted for the evaluation.
Data obtained in this study showing significant increase in activities of liver enzymes indicate impaired integrity of hepatocellular membrane and this could culminate to liver dysfunction. Studies have shown that oxidative damage to cellular molecules on exposure to PQ presents functional and biochemical changes which manifests as liver damage [33,34], and observed as increased activities of liver enzymes [35]. These observations concur with previous studies on paraquat induced liver toxicity, which showed increase in serum activity of liver enzymes [36,37].
Since the reduction of PQ generates free radical [38], it may be adduced that increase in serum activities of liver enzyme resulted from free radical induced oxidative hepatocellular damage as reported in many pathological conditions such as liver and kidney damage, cancer and diabetes mellitus [39,40]. However, reduced activities of liver enzymes observed on nutritional supplements treated groups indicate protective effect against paraquat induced toxicity and possibly amelioration of liver damage.
The non-significant change of total protein and significant increase in globulin observed in this study is contrary to the report by Lalruatfela et al. [41], which showed significant decrease in these parameters in paraquat exposed groups. The increase in serum globulin may be attributed to liver inflammation and damage from oxidative stress [42,43]. However, Banaee et al. [44] reported decreased serum globulin in sub-lethal Paraquat exposure. Also, the significant decrease of albumin may indicate dysfunctional protein synthesizing potential prevalent in hepatotoxic conditions [45,44]. Furthermore, decreased albumin in paraquat control may be due to the capacity of paraquat to bind to plasma albumin as reported by Jaiswal et al. [46]. This may engender spontaneous conformational changes and fragmentation of albumin. Decreased albumin may also be attributed to increased breakdown of some amino acids by paraquatinduced oxidative stress. The supplement treated groups (especially, Vitamin C and Synergy group) showed significant improvement in albumin concentration indicating accelerated liver regeneration which may have enhanced synthesis of proteins, especially albumin.
The significant increase in concentration of bilirubin in paraquat exposed rats may be the aftermath effect of decreased uptake and conjugation of bilirubin by dysfunctional hepatic cells. These values of serum bilirubin agree with the report of Ahmad et al. [37] and McCormack et al. [36]. Reduction of paraquat-induced elevation of bilirubin concentration in nutritional supplement treated groups indicate potential protective role with potential ameliorative effect which could restore bilirubin uptake and conjugation by hepatic cells and possible secretion into the bile ducts.
Glutathione (GSH) is an important antioxidant produced by liver cells and the major soluble antioxidant in cell compartment [45]. The significant decrease in GSH concentration may be attributed to its use in various protective roles against oxidants [13,45]. Glutathione donates its electrons to cellular oxidants and are oxidized in the process. Oxidized glutathione can be reduced in the presence of NADPH and glutathione reductase [15]. As oxidative stress has a crucial role in paraquat induced liver injury, in this study, total antioxidant capacity (TAC) was measured, as indicator of blood, cells, and tissues defense system against free radicals. TAC measures the antioxidant capacity of all antioxidants in a biological sample and not just the antioxidant capacity of a single compound. Measurement of TAC can provide information on overall antioxidant status, which may include those antioxidants not yet recognized or not easily measured [47,48]. The significant reduction of TAC in paraquat-exposed groups may be attributed to the excess production of free radicals by paraquat, which overwhelms the systems antioxidant capacity. This leads to oxidative damage [5,6,49] especially hepatic injury [50], due to paraquat-induced increase in free radical production and attenuation of antioxidant capacity. The observed significant decrease in glutathione concentration confirms the adverse effect of paraquat in attenuation of antioxidant level. This situation gives impetus to oxidative damage as indicated by the significant increase in malondialdehyde concentration. This is so because the free radicals provoke tissue injury by interacting with polyunsaturated fatty acids of phospholipids membranes [51,52] of hepatocytes and cell organelles producing free radicals and MDA. Malondialdehyde produced during autocatalytic chain reaction (lipid peroxidation) is very harmful to the cells [53]. Data obtained in this study showed that treatment of PQ exposed groups with vitamin C, garlic and glutathione increased and maintained liver concentration of glutathione and total antioxidant. The pathway of glutathioneascorbate cycle detoxifies reactive oxygen species [54,55]. The supplement treated groups also presented MDA concentration close to the normal control indicating effective inhibition of oxidative stress and consequently reduced lipid peroxidation. These findings are in agreement with previous results where antioxidants such as vitamin C and garlic were used to ameliorate the effect of xenobiotic induced toxicity [56,57].
The reduction of PQ by the interplay NADPH-cytochrome P450 reductase and NADH: ubiquinone oxidoreductase give rise to PQ mono cation free radical, leading to the generation of the superoxide radical (O2 •–) [38,58,59]. These events results in histopathological changes as observed in the present study [60,61]. The observed liver parenchyma showing hepatocytes surrounded by fatty materials indicates failure in fatty acid oxidation. Studies have shown that Paraquat exposure causes derangement in fatty acid metabolism leading to accumulation of fatty acids in hepatocytes [62,63]. The congested central vein observed in garlic (GC) treated rats on Paraquat exposure may be attributed to endothelial cell damage which leads to microcirculation failure and liver congestion. These are consequences peroxynitrite anion generated during paraquat reduction [64]. This indicates overwhelming of the antioxidant potentials of garlic. However, the combination of the three supplements Vitamin C, garlic and glutathione showed significant attenuation of oxidative effect of Paraquat and restoration of hepatic integrity. Vitamin C is an important cofactor in not less than eight enzymatic reactions which activities are important in wound-healing and also acts as an antioxidant, protecting against Oxidative stress [17,65]. The intracellular and extracellular availability of glutathione are important in keeping ascorbate in a reduced state [18]. The synergy of the combined supplement may have inhibited nitric oxide synthase. Day et al. [66] reported that endothelial cell toxicity induced by exposure to Paraquat was attenuated by inhibitors of nitric oxide synthase, which prevent NADPH oxidation. Also, the combined supplement may relief inflammation [67] by interfering with lipid peroxidation and metabolism.
Conclusion
The findings of this study suggests that exposure to the herbicide paraquat dichloride can initiate oxidative stress, lipid peroxidation and liver damage. Furthermore the concomitant administration of garlic, vitamin C and glutathione could be a useful in attenuating the oxidative induced damage in sensitive organs.
Conflict of Interest
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Abd El Kader MA, Fyiad AA, Soliman MS (2006) Protective role of aqueous garlic extract on para quatinduced lung injury in rats. J Biomed Sci 20: 125-136.
- Ahmed MM (2010) Radio and chemo protective properties of hesperidin against genotoxicity induced by gamma radiation and/or paraquat in rat bone marrow cells. J Rad Sci Applic 23: 233-244.
- Tanner CM, Kamel F, Ross GW, Hoppin JA, Goldman SM, et al. (2011) Rotenone, paraquat, and Parkinson's disease. Environ Hlth Perspect 119: 866-872.
- He X, Wang L, Szklarz G, Bi Y, Ma Q (2012) Resveratrol inhibits paraquat- induced oxidative stress and fibrogenic response by activating the nuclear factor erythroid 2-related factor 2 pathway. J Pharmacol Exp Ther 342: 81-90.
- Hafez AM (2009) Antigenotoxic activity of melatonin and selenium against genetic damage induced by paraquat. Aust J Basic & Appl Sci 3: 2130-2143.
- Meng XX, Wang RL, Gao S (2013) Effect of ulinastatin on paraquat-induce doxidative stress in human type II alveolar epithelial cells. World J Emerg Med 4: 133-137.
- National Center for Complementary and Integrative Health (2012) Garlic (''Allium sativum'' L.) National Center for Complementary and Integrative Health, US National Institutes of Health.
- Ujowundu CO, Kalu FN, Nwosunjoku EC (2011) Iodine and inorganic mineral contents of some vegetables, spices and grains consumed in Southeastern Nigeria. Afri J Biochem Res 5: 57-64.
- Borlinghaus J, Albrecht F, Gruhlke MC, Nwachukwu ID, Slusarenko AJ (2014) Allicin: Chemistry and biological properties. Molecules. 19: 12591-12618.
- Maldonado PD, Alvarez-Idaboy JR, Aguilar-González A, Lira-Rocha A, Jung-Cook H, et al. (2011) Role of allyl group in the hydroxyl and peroxyl radical scavenging activity of S-allylcysteine. J Phys Chem B 115: 13408-13417.
- Sukta D (2002) Garlic – A natural source of cancer preventive compounds. Asian Pacific J Cancer Prev 3: 305-311.
- Singh SV, Pan SS, Srivastava SK (1998) Differential induction of NAD(P)H: Quinone oxidoreductase by anticarcinogenenic organosulfides from garlic. Biochem Biophys Res Comm 244: 917-20.
- Pompella A, Visvikis A, Paolicchi A, De Tata V, Casini AF (2003) The changing faces of glutathione, a cellular protagonist. Biochem Pharmacol 66: 1499-1503.
- Lu SC (2013) Glutathione synthesis. Biochimica et Biophysica Acta. 1830: 3143-3153.
- Couto N, Malys, Gaskell SJ, Barber J (2013) Partition and turnover of glutathione reductase from Saccharomyces cerevisiae: A proteomic approach. J Proteome Res. 12: 2885-2894.
- Levine M, Rumsey SC, Wang Y (2000) Vitamin C. In Stipanuk MH. Biochemical and physiological aspects of human nutrition. Philadelphia: WB Saunders. P: 541-567.
- Padayatty SJ, Katz A, Wang Y (2003) Vitamin C as an antioxidant: Evaluation of its role in disease prevention. J Am College of Nutr 22: 18-35.
- Gropper SS, Smith JL, Grodd JL (2005) Advanced nutrition and human metabolism. Belmont CA: Thomson Wadsworth pp: 260-275.
- Michels A, Frei B, Vitamin C (2012) In Caudill MA, Rogers M. Biochemical, Physiological, and Molecular Aspects of Human Nutrition 3rd edn, Philadelphia: Saunders p: 627-654.
- National Institute of Health (1985) Guide for the care and use of laboratory animals. DHEW Publication, Office of Science and Health Reports, Bethesda, USA.
- Reitman S, Frankel S (1957) A Colorimetric method of determination of serum glutamic oxaloacetic and glutamic pyruvic transminase. Amer J Pathol 28: 56-62.
- Rec GSCC (1972) Clinical Biochemistry. J Clinical Chem 10: 182.
- Jendrassik L, Grof PV (1938) photometrische methoden zur Bestimmung des blutbilirubins. Biochem 297: 81-89.
- Tietz NW (1995) Clinical guide to Laboratory Test. 3rd Ed. WB Sunders Company Philadelphia. 518-519.
- Doumas BT, Watson WA, Biggs HG (1971) Albumin standards and the measurement of serum albumin with bromocresol green. Clin Chimica acta 31: 87-97.
- Wallin B, Rosengren B, Shertzer HG, Cameyo G (1993) Lipoprotein oxidation and measurement of TBARS formation in a single microlitrepeate; its use for evaluation of antioxidants. Annual Rev Med 208:10-15.
- Raja S, Ahmed K, Kumar V, Mukherjee K, Bandyopadhyay A (2007) Antioxidant effect of Cytisus scopararius against carbon tetrachloride treated liver injury in rats. J Ehnopharm 109: 41-47.
- Benzie IF, Strain JJ (1996) The ferric reducing ability of plasma (FRAP) as a measure of "antioxidant power": the FRAP assay. Anal Biochem 239: 70-76.
- Okoro I (2002) Manual of practical histology, 2nd edn, Peace Publishers Owerri.
- Conn HJ, Darrow MA, Emmels VM (1960) Staining procedures used by the biological stain commission, 2nd edn, The Williams & Wilkins Co. Baltimore. p: 93- 94,
- https://www.ars.usda.gov/ARSUserFiles/20902500/DavidHuggins/NoTill.pdf.
- Hakim D (2016) This Pesticide Is Prohibited in Britain. Why Is It Still Being Exported? New York Times.
- Novaes RD, Gonçalves RV, Marques DC, Cupertino Mdo C, Peluzio Mdo C (2012) Effect of bark extract of Bathysa cuspidata on hepatic oxidative damage and blood glucose kinetics in rats exposed to paraquat. Toxicol Pathol 40: 62-70.
- Amirshahrokhi K, Bohlooli S (2013) Effect of methylsulfonylmethane on paraquat-induced acute lung and liver injury in mice. Inflammation 36: 1111-1121.
- Novaes RD, Goncalves RV, Cupertino MC, Santos EC, Bigonha SM (2016) Acute paraquat exposure determines dose-dependent oxidative injury of multiple organs and metabolic dysfunction in rats: impact on exercise tolerance. Int J Exp Pathol 97: 114-124.
- McCormack AL, Atienza JG, Johnston LC, Andersen JK, Vu S, et al. (2005) Role of oxidative stress in paraquat-induced dopaminergic cell degeneration. J Neurochem 93: 1030-1037.
- Ahmad I, Shukla S, Kumar A, Singh BK, Kumar V (2013) Biochemical and molecular mechanisms of N-acetyl cysteine and silymarin-mediated protection against maneb- and paraquat-induced hepatotoxicity in rats. Chem Biol Interact 201: 9-18
- Clejan L, Cederbaum AI (1989) Synergistic interaction between NADPH-cytochrome P-450 reductase, paraquat and iron in the generation of active oxygen radicals. J Biochem Pharmacol 38:1779-1786.
- Anosike CA, Ugwu UB, Nwakanma O (2008) Effect of ethanol extract of Pyrenacantha staudtii leaves on carbontetrachloride induced hepatotoxicity in rats. Biokemistri 20: 17-22
- Zeb Shah T, Ali AB, Ahmad Jafri S, Qazi MH (2013) Effect of Nicotinic Acid (Vitamin B3 or Niacin) on the lipid profile of diabetic and non-diabetic rats. Pak J Med Sci 29: 1259-1264.
- Lalruatfela PL, Saminathan M, Ingole RS, Dhama K, Joshi MV (2014) Toxicopathology of Paraquat Herbicide in Female Wistar Rats. Asian J Animal Vet Advanc 9: 523-542.
- Limdi JK, Hyde GM (2003) Evaluation of abnormal liver function tests. Postgrad Med J 79: 307-312.
- Ujowundu CO, Nnanna CG, Ndubuisi EU, Ngwu PC, Uzoma CW, et al. (2017) Glyphosate-Based Pesticide-Induced Biochemical Changes in Hepatic and Renal Tissues of Clarias Gariepinus. FUTO J Series 1: 225-235.
- Banaee M, Haghi BN, Tahery S, Shahafve S, Vaziriyan M (2016) Effects of Sub-Lethal Toxicity of Paraquat on Blood Biochemical Parameters of Common Carp, Cyprinus carpio. Iranian J Toxicol 10: 1-5.
- Ujowundu CO, Kalu FN, Igwe CU, Agha NC, Igwe KO (2012) Biochemical Studies on the Amelioration of Petroleum Product Intoxication with Indigenous Plants. Inter J Biochem Res Rev 2: 87-97.
- Jaiswal R, Khan MA, Musarrat J (1992) Photosensitized paraquat-induced structural alterations and free radical mediated fragmentation of serum albumin. J Photochem Photobiol B 67: 163-170.
- Ahmad I, Kumar A, Shukla S, Pandey PH, Singh C (2008) The involvement of nitric oxide in maneb- and paraquat-induced oxidative stress in rat polymorphonuclear leukocytes. Free Radic Res 42: 849-862.
- Ferrari CK (2012) Effects of xenobiotics on total antioxidant capacity. Interdiscip Toxicol 5: 117-122.
- Roy W, Maya K, Shawn M, Larry L, Christine D, et al. (2006) Dynamic responses of the glutathione system to acute oxidative stress in dystrophic mouse (mdx) muscles. Am J Physiol Regul Integr Comp Physiol 291: 704-710.
- Atashpour S, Kargar JH, Kargar JZ, Zarei S (2017) Antioxidant effects of aqueous extract of Salep on Paraquat-induced rat liver injury. World J Hepatol 9: 209-216.
- Spitz DR, Azzam EI, Li JJ, Gius D (2004) Metabolic oxidation/reduction reactions and cellular responses to ionizing radiation: A unifying concept in stress response biology. Cancer Metastasis Rev. 23: 311-322.
- Soliman SM (2007) Protective role of oregano oil against histological changes in whole body gamma irradiated albino rats. J Egypt Ger Soc Zool 52: 46-56.
- Halliwell B, Gutteridge JMC (2004) Free radicals in biology and medicine. 3rd Ed. Oxford University PressInc, New York.
- Noctor G, Foyer CH (1998) Ascorbate and glutathione: Keeping active oxygen under control. Annual Rev Plant Physiol Plant Mol Bio 49: 249-279.
- Whitbread AK, Masoumi A, Tetlow N, Schmuck E, Coggan M (2005) Board PG. Characterization of the omega class of glutathione transferases. Meth Enzymol 401: 78-99.
- Karima Z W (2001) The Influence of Vitamin C or Selenium on Paraquat-induced Toxicity in Guinea Pigs. Pak J Bio Sci 4: 81-88.
- Noh B, Lee J, Won Y, Park H, Lee S (2011) The antioxidative effect of black garlic extract on paraquat-induced oxidative stress in ICR mice. Korean J Food Sci Technol 43: 10
- Fukushima T, Yamada K, Isobe A, Shiwaku K, Yamane Y (1993) Mechanism of cytotoxicity of paraquat. I. NADH oxidation and paraquat radical formation via complex I. Exp Toxicol Pathol 45: 345-349.
- Dicker E, Cederbaum AI (1991) NADH-dependent generation of reactive oxygen species by microsomes in the presence of iron and redox cycling agents. Biochem Pharmacol 42: 529-535.
- Ussama ZS, Neamat HA, Amina MM, Mustafa MM (2014) Effects of omega-3 fatty acids against Ehrlich carcinoma-induced hepatic dysfunction. J Cancer Res Exp Oncol 6: 20-28.
- Hamza RG, El-Shennawy HM (2016) Study of the influence of Egyptian apple against oxidative stress in gamma-irradiated rats. Pakistan J Zool 48: 547-556.
- Aoyama T, Peters JM, Iritani N, Nakajima T, Furihata K, et al. (1998) Altered constitutive expression of fatty acid-metabolizing enzymes in mice lacking the peroxisome proliferator-activated receptor alpha (PPAR alpha). J Biol Chem 273: 5678-5684.
- Chohan MS, Tahir M, Lone KP, Sami W, Munir B (2010) Paraquat Induced Hepatotoxicity in Albino Mice. Pakistan J Zool 42: 69-73,
- O'donnell VB, Freeman BA (2001) Interactions between nitric oxide and lipid oxidation pathways: implications for vascular disease. Circul Res 19: 12-21.
- Food Standards Agency (2016) Vitamin C. Food Standards Agency (UK). Archived from the original on 2010-11-16.Retrieved 2016-06-02.
- Day BJ, Patel M, Calavetta L, Chan LY, Stamler JS (1999) A mechanism of paraquat toxicity involving nitric oxide synthase. Med Sci 96: 12760-12665.
- Parhiz H, Roohbakhsh A, Soltani F, Rezaee R, Iranshahi M (2015) Antioxidant and anti-inflammatory properties of the citrus flavonoids hesperidin and hesperetin: an updated review of their molecular mechanisms and experimental models. Phytother Res 29: 323-331.