Joseph M Bodi1, Célestin N Nsibu1, Roland L Longenge1, Michel N Aloni2, Pierre Z Akilimali3, Pierre M Tshibassu4, Patrick K Kayembe3, Ahmeddin H Omar5, Kenji Hirayama6, Jan Verhaegen7, Aimé Lumaka8,9* and Prosper T Lukusa8
1Discipline of Pharmacology, School of Pharmacy, University of the Western Cape, Bellville 7535, South Africa
2Department of Chemistry, University of the Western Cape, Bellville 7535, South Africa
3South African Herbal Science and Medicine Institute, University of the Western Cape, Bellville 7535, South Africa
4Discipline of Pharmaceutics, School of Pharmacy, University of the Western Cape, Bellville 7535, South Africa
5Discipline of Pharmacology, School of Pharmacy, University of the Western Cape, Bellville 7535, South Africa
6Department of Chemistry, University of the Western Cape, Bellville 7535, South Africa
7South African Herbal Science and Medicine Institute, University of the Western Cape, Bellville 7535, South Africa
8Discipline of Pharmaceutics, School of Pharmacy, University of the Western Cape, Bellville 7535, South Africa
9Discipline of Pharmaceutics, School of Pharmacy, University of the Western Cape, Bellville 7535, South Africa
- *Corresponding Author:
- Aimé Lumaka
Department of Biomedical and Preclinical Sciences
GIGA-R, Laboratory of Human Genetics
University of Liège, Belgium
E-mail: aime.lumaka@uliege.be
Received date: August 18, 2018; Accepted date: November 22, 2018; Published date: November 30, 2018
Citation: Bodi JM, Nsibu CN, Longenge RL, Aloni MN, Akilimali PZ, et al. (2018) High IgG1 Malaria Antibodies Level in Children is a Possible Risk Factor of Blackwater Fever: A Case-Control Study. Ped Health Res Vol.3 No.3:9.
Copyright: © 2018 Bodi JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Black-water fever; IgG; Antibodies; Malaria; Congo
Introduction
Pathogenesis of acute massive intravascular hemolysis in Blackwater fever (BWF) is recognized to be very complex. Deficiency in malaria immunity often observed in the expatriate population, Quinine treatment and Plasmodium falciparum parasite are the most commonly incriminated factors [1-3]. It is likely that all these factors interact with some underlying genetic factors for the development of the BWF [4]. It was previously observed that BWF occurred during P. falciparum malaria episodes in individuals receiving quinine [3], prompting further investigations of the role of the parasite and that of the quinine compound in the occurrence of BWF [2,5-9]. It has also been reported that the complex, that is made up by Quinine the P. falciparum Parasite and the Red blood cell, alters the red blood cell membrane and acts as a neo-antigen, triggering the synthesis of antibodies. Future contacts between these antibodies and neo-antigen will result in intravascular acute massive hemolysis. This reaction is attributed to complement activation through either the classical pathway or the alternative pathway [10-14].
Malaria antibodies increase gradually with age in autochthone population, due to sustained contacts with the vector and malaria parasite [15-30]. This elevation is a more complex process that can be divided into few steps. Children aged below 6 months are under a protection provided to them by maternally transmitted antibodies, fetal hemoglobin, the low concentration of Para Amino Benzoic Acid contained in maternal breast milk, and the use of the insecticide-treated net (INT). Later, children between 6 months and 5 years lose most of these protective factors and become exposed to malaria attacks. This vulnerability is confirmed by the occurrence of about 90% of malaria gross mortality during this time window [31]. Finally, after 5 years of age children develop acquired protective malaria immunity and clinical malaria episodes decrease both in frequency and severity [31-33].
Regarding the specific aspects of this malaria immunity, IgG1 directed against Apical Membrane Antigen 1 (AMA1) and the carboxy-terminal region of the Merozoite Surface Protein 1 (MSP1-19), are predominant in malaria immunity protection during the first 2 years of life [28,29,34]. From the 3rd year of the life, malaria IgG3, directed against MSP2, increase [28,34]. Basically, the role of these antibodies is to protect against malaria episodes. Surprisingly, the majority of children with BWF are above 5 years, an age where children are expected to have already acquired malaria protective immunity against malaria in the stable endemic area [5,6,35,36]. To date, the amounts of these malaria antibodies have not been evaluated in a systematic way in BWF patients. Also, the possibly perverse effect of malaria antibodies in the occurrence of BWF is not fully elucidated. This study aimed at determining the profile of malaria IgG1 antibodies in children with blackwater fever compared to patients with uncomplicated malaria.
Methods
Study design, subjects, and case definitions
This is a case-control study carried out in four medical institutions across Kinshasa, between January 2010 and December 2011. The 2-years study period was necessary to gather sufficient. Kinshasa, the capital of DRC, is characterized by two distinct seasons, a rainy season (mid-September to mid- May) and a dry season (mid-June to mid-August). Cases are patients with Blackwater Fever (BWF), whereas controls had uncomplicated Plasmodium falciparum malaria (UM). BWF was defined as the presence of hemoglobin in the dark urine after acute intravascular hemolysis (macroscopic hemoglobinuria). In addition, cases were febrile patients, with jaundice, anemia and Plasmodium falciparum malaria confirmed by the presence of P. falciparum parasite on blood thick and film. Conversely, Uncomplicated Malaria (UM) were patients with fever associated with the presence of P. falciparum on blood thick and film. Consecutively to the recruitment of a case, two controls were recruited, matching for gender, age and residential area to the case. The mean age was 8.62 ± 3.84 years for cases and 8.55 ± 3.77 years for controls. The range was 2-15 years in the two groups.
Clinical evaluation
A standard clinical examination was conducted to obtain a medical history and clinical data. Malaria was confirmed by the presence of the parasite in malaria blood thick and film.
Laboratory measurements
Twenty mL of fresh urine were collected from each participant. The presence of hemoglobin in urine was first accessed by urinary dip stick (Medi test Combi9, Machery Eur, Paris, France) and then confirmed by a spectrometer (Thermo Genesis 10 BIO, New York USA) using 3,3′ dimethyl benzidine reagent and protocol [37].
Collection of blood
Sera were collected in small cryotubes of 2 ml, and then stored at -80 Celsius degrees (°C) in the laboratory of Department of Tropical Medicine, school of medicine at the University of Kinshasa. Later, these samples were transferred to the Institute of Tropical Medicine at Nagasaki University in Japan for immunological analysis. Before the shipment to Nagasaki, samples were taken out of the -80°C storage; each individual tube was stored in an absorbing pouch accordingly labelled with the patient’s ID. Next, these pouches were stored in (UN code UN3373 (biology substance category B) boxes following the P650 packing instructions. The box was picked-up from our University in Kinshasa, transported and delivered at the Nagasaki University, Japan by DHL company. Samples were shipped through standard DHL cold transport chain.
Quantification of malaria antibodies IgG1
Malaria Immunoglobulins (IgG1) were assessed from the individual sera by ELISA. Briefly, 96-well plates were pre-coated with 100 μl of 0.1 μg/ml of Plasmodium falciparum crude antigen in coating buffer and kept overnight at 4°C. Plates were washed three times with 400 μl/well of 0.05% Tween-PBS, then blocked for nonspecific binding using 340 μl/well of 0.1% blocking reagent (Roche Diagnostics, Mannheim, Germany) for 1h at 37°C. Plates were washed three times with 400 μl/well of 0.05% Tween-PBS, then 100 μl of serially diluted sera (1:10) was added and incubated at 37°C for 3h. Plates were then washed five times with 400 μl/well of 0.05% Tween-PBS and 100 μl of Horseradish Peroxidase (HRP)-conjugated goat anti-human IgG1 (Southern Biotechnology, Birmingham, AL), diluted with blocking buffer (1:4000), was added and incubated for 1 h at room temperature. Plates were washed 5 times with 400 μl/well of 0.05% Tween-PBS and the antigen-antibody reaction was visualized by the addition of 50 μl/well of 3,3',5,5'- tetramethylbenzidine (TMB) (Vector Laboratories, CA, USA). The color development reaction was stopped after 30 min by adding 50 μl of 1N of H2SO4, and the absorbance was measured in an automated plate reader (Bio-Rad, Hercules, CA) at 450 nm [38].
Ethics statement
Written informed consent was obtained from parents for each patient and the study protocol conforms to the ethical guidelines of the World Medical Association Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects. The study received approval of Ethics Committee of Public Health School of University of Kinshasa under the number ESP/CE/027B/2011. Patient’s information was obtained using anonymized research forms designed in local languages.
Data management and analysis
Data were recorded using Epi-Info 7 Version 2002 (CDC) and analyzed using SPSS 18.0. The geometric mean of malaria antibodies with his confidence interval was calculated. After geometric mean calculation, data were transformed into logarithm of antibodies. The error of mean with confidence interval were calculated and allowed comparison with the logarithm of antibodies in the 2 groups. The simple linear regression was used to analyze the correlation between the logarithm of antibodies and age of children in the two groups.
Ancova model allowed modeling the logarithm of antibodies and age in months between cases and controls. All the tests were calculated at 5% significance. Descriptive analysis was performed to obtain either means for quantitative variables or proportions for all the qualitative variables. The confidence interval at 95% was calculated.
Multivariate analysis was used to determine associations between variables and BWF. The odds ratio was used to measure the force of associations.
Results
A total of 129 children, 43 with BWF and 86 with UM were recruited in the study. Sixty-eight (52.7%) females and 61 (47.3%) males were included with a male to female sex-ratio of 1:1.1 and the age ranging from 2 to 15 years with a mean age of 8.57 ± 3.73 years. The mean age was 8.62 ± 3.84 years for patients with BWF or 8.55 ± 3.77 years for UM. In total, 81.4% of children with BWF were over 5 years of age, while only 18.6% under 5 years old [OR: 1.33 (0.53-3.32) (Table 1).
| Variables |
Case (n=43) |
Controls (n=86) |
Total (n=129) |
OR (IC95%) |
p |
| Distribution for age |
| - = 5 years |
8 (18.6) |
20 (23.3) |
28 (21.7) |
1 |
0.676 |
| - > 5 ears |
35 (81.4) |
66 (76.7) |
101 (78.3) |
1.33 (0.53-3.32) |
| Sex: n(%) |
| - Male |
21 (48.8) |
40 (46.7) |
61 (47.3) |
1.10 (0.53-2.28) |
0.803 |
| - Female |
22 (51.2) |
46 (53.5) |
68 (52.7) |
1 |
| Season |
| - Rainy |
38 (88.4) |
51(59.3) |
89 (69.0) |
5.22 (1.87-14.56) |
<0.001 |
| - Dry |
5 (11.6) |
35 (40.7) |
40 (31.0) |
1 |
| Plasmodium |
| - Falciparum |
37 (86.0) |
73 (84.9) |
110 (85.3) |
1.10 (0.39-3.12) |
0.86 |
| - Falciparum-malariae |
6 (14.0) |
13 (15.1) |
19 (14.7) |
1 |
| Parasitemia (per microliter) |
| - Low<500/μL |
32 (78.0) |
43 (51.8) |
76 (61.3) |
3.31 (1.41-7.78) |
0.005 |
| - High> 500/μL |
9 (22.0) |
40 (48.2) |
48 (38.7) |
1 |
|
Table 1: sociodemographic features of children with BWF versus UM.
Interestingly, 6 (14%) had co-infection of P. falciparum and Plasmodium malariae while 37 (86%) have mono-infection. Likewise, 73 children (84.9%) in the control group had monoinfection with P. falciparum, while 13 children (15.1%) in this group had co-infection with P. falciparum and P. malariae. Low parasitemia was mostly observed in BWF children. The association shows a statistically significant difference 331(141-778) with p=0.005 (Table 1).
In univariate analysis, using crude Odds ratio, quinine was significantly associated with the occurrence of BWF [OR:47.31 (10.64-210.3), p<0.001] (Table 2). Interestingly, in multivariate analysis, using adjusted Odds Ratio, quinine was associated with the occurrence of BWF with p<0.001 [OR: 50.19 (10.7-234.4)].
| Variables |
Crude OR |
adjusted OR |
| (95% IC) |
p |
(95% IC) |
p |
| Antimalaria drugs |
| - ACT |
1 |
<0.001 |
1 |
<0.001 |
| - Quinine |
47.3 (10.6-210.3) |
50.19 (10.7-234.4) |
| G6PDstatus |
| - Normal (= 276UI/L) |
1 |
0.017 |
1 |
0.115 |
| - Deficiency (<276UI) |
0.35 (0.14-0.54)) |
0.39 (0.12-1.27) |
| Parasitemia |
| - High> 500/μL |
1 |
0.005 |
1 |
0.012 |
| - Low<500/μL |
0.30 (0.13-0.71) |
0.25 (0.08-0.74) |
Table 2: Determinants factors in the occurrence of BWF.
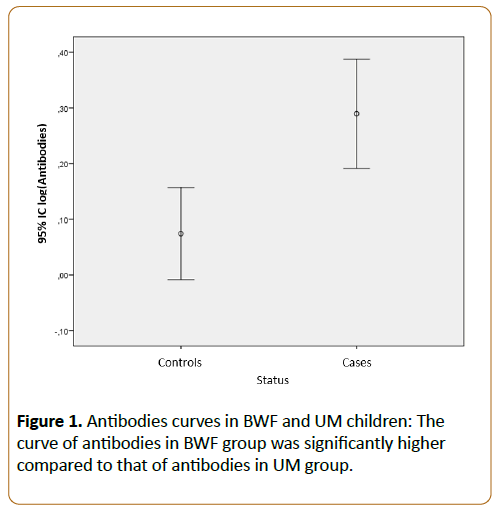
The geometric mean of antibodies in the study population was high in Blackwater fever children.
[1.95 (IC95%: 1.55-2.44)] versus in control group: [1.19 (IC95%: 0.98-1.002.0)]. The curve of antibodies in BWF group was significantly higher compared to that of antibodies in UM group (Figure 1).
Figure 1: Antibodies curves in BWF and UM children: The curve of antibodies in BWF group was significantly higher compared to that of antibodies in UM group.
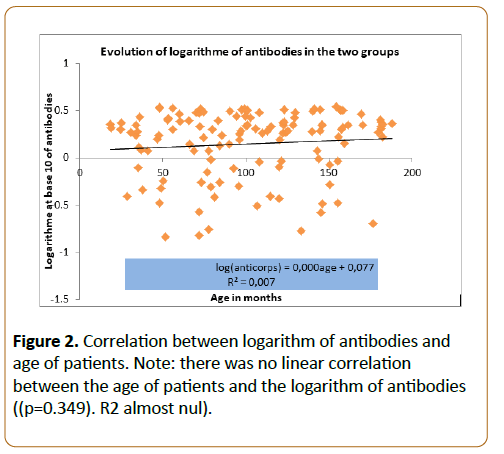
Regarding the evolution of antibodies and age of patients, there was no linear correlation between the age of patients and the logarithm of antibodies. Age alone did not influence directly the rate of antibodies (p=0.349). The coefficient of R2 was totally null and this relation was not linear (Figure 2).
Figure 2: Antibodies curves in BWF and UM children: The curve of antibodies in BWF group was significantly higher compared to that of antibodies in UM group.
Among the hemoglobinuria patients, seven (16.2%) developed Acute Renal Failure (ARF) when the other did not. Due to financial constraints, only two children among those seven with ARF received peritoneal dialysis whereas others received other medication-based conservative treatments. In the evolution, three of the patients with ARF who did not receive dialysis developed anuria and died from this complication.
Discussion
Malaria is still one of the deadlier diseases in children in Sub- Saharan African countries and it takes various deadly presentations including BWF. We conducted a case-control study to investigate the possible association between IgG1 against malaria parasite and the occurrence of BWF in children from DR Congo.
We included both small children and young adolescents but observed no significant association between the age and the risk for BWF. A great proportion of individuals infected by more than one species of malaria parasite was noticed in this study. However, there was no significant change in the risk for BWF between those with only P. falciparum and those with both P. falciparum and P. malariae.
It is widely known that acquired immunity establishes with age and is triggered by exposition to pathogen among other factors. Of note, people living in the high malaria transmission area, where host-pathogen interactions are sustained, develop malaria immunity early in life. In this setting, children from around 5 years already have established acquired immunity against malaria, thus exhibit a significant decrease of malaria episodes [19-33]. During the first two years of life, malaria IgG1 antibodies, directed against AMA1 and MSP1-19, are gradually elevated [28,29,34]. These IgG1 remain predominant till around the age of 10 when IgG3 targeting MSP2, which start increasing from 3 years of age, take over. Local studies confirmed this antibody conversion and showed high parasitemia around 10 years old [39,40]. No linear correlation was observed between the age of patients and the values of IgG1 antibodies in the current study. A larger cohort will be useful to verify this correlation. It should, however, be mentioned that many other factors are involved in the acquisition of immunity like the duration of exposure to the vector, the nature of P. falciparum antigen involved, the vector, the immune and genetic status of the patients [23,25,28,41,42], which were beyond the scope of this study.
Previous studies [25] suggested a slight association between total malaria IgG and the malaria prevalence, which in turn is known to be varied depending on the weather seasons. In this study, patients were recruited over 2 years, during 2 rainy seasons and 2 dry seasons. BWF was significantly observed during rainy seasons (Table 1), known as the high malaria prevalence season. However, we did not investigate the association between IgG and the seasonal prevalence of malaria.
Malaria IgG1 are known to be anti-parasitemia and expected to be observed in combination with low parasitemia, whereas malaria IgG3 antibodies are not anti-parasitemia and can explain the high parasitemia. This has been proven in children above 5 years as well as an expatriate, both found to develop acute massive intravascular hemolysis in the presence of high malaria antibodies IgG1 and low parasitemia [43]. Likewise, our result also shows that malaria IgG1 was significantly elevated in BWF patients. It should be noted that the elevated IgG1 levels did not protect them against BFW. Malaria IgG1 may probably be involved in the pathogenesis of the disease.
To be consistent with the high IgG1 values, one would expect parasitemia to be lower in patients with established acquired immunity against malaria. Many studies have reported low parasitemia in BWF patients [44]. We now report hereby that Congolese patients presenting with BWF have low parasitemia compared to those with uncomplicated malaria. High levels of IgG1 can, of course, explain the observed low parasitemia. However, other external factors specific to our countries such as the use of anti-parasitemia nets and the regular intake of antimalarial medication can also contribute to low parasitemia. Of note, we have shown that the intake of Quinine, a popular antimalaria drug, is significantly associated with the occurrence of BWF in our cohort. Therefore, Quinine compound can explain both the low parasitemia and the BWF by acting either alone or in conjunction with IgG1 antibodies.
Peritoneal dialysis proved to be an effective treatment for those of our patients who developed Acute Renal Failure (ARF). Unfortunately, accessibility is limited to the combination of multiple factors including limited income, expensive reagent often imported from overseas countries. Luckily, a new pediatric dialysis service has been implemented and offers peritoneal dialysis at a significantly lower cost than in the past at the University hospitals in Kinshasa. Hopefully, children will receive better and quicker care to prevent the avoidable deaths as observed during our study.
Conclusion
The malaria IgG1 antibodies were very high in BWF children compared to uncomplicated malaria patients: 1.95 (IC95%: 1.55-2.44) versus 1.19 (IC95%: 0.98-1.43), p=0.002. The high IgG1 malaria did not protect children to develop BWF but may play important role in the activation of complement resulting in acute massive hemolysis leading to BWF. Low parasitemia was associated with the BWF children. The age alone did not influence the level of IgG1.
Limitations of the Study
Increasing sample size, measuring of malaria antibodies IgG3 and Quinine antibodies, exploring complement activation could have improved the design.
Acknowledgements
The authors are thankful to all children and parents who
participated to this study, and to Nasir Nshuaib for the
quantification of malaria IgG1 antibodies (department of
immunogenetics, Nagasaki University, Japan). We thank all our
colleagues, nurses and lab technicians involved in sample and
data collection. This research project was supported by the
University of Nagasaki through the Grant-in-Aid for Scientific
Research (B) 17H04072(2017-2021) of KAKENHI; and the
Katholieke Universiteit Leuven (Belgium) through the scholarship
program for young Congolese researchers (Bourses chaires
scientifiques pour jeunes Congolais). We are grateful to Prof
Fons Verdonck of the KU Leuven Alumni for his support
References
- Palfai TP, Monti PM, Ostafin B, Hutchison K (2000) Effects of nicotine deprivation on alcohol-related information processing and drinking behavior. J Abnorm Psychol 109: 96-105.
- Harrison EL, Hinson RE, McKee SA (2009) Experimenting and daily smokers: episodic patterns of alcohol and cigarette use. Addict Behav 34: 484-486.
- Howell A, Leyro T, Hogan J, Buckner J, Zvolensky M (2010) Anxiety sensitivity, distress tolerance, and discomfort intolerance in relation to coping and conformity motives for alcohol use and alcohol use problems among young adult drinkers. Addictive Behaviors 35:1144-1147.
- Krukowski RA, Solomon LJ, Naud S (2005) Triggers of heavier and lighter cigarette smoking in college students. J Behav Med 28: 335-345.
- Reed MB, Wang R, Shillington AM, Clapp JD, Lange JE (2007) The relationship between alcohol use and cigarette smoking in a sample of undergraduate college students. Addictive Behaviors 32: 449-464.
- Hughes JR, Kalman D (2006) Do smokers with alcohol problems has more difficulty quitting? Drug Alcohol Depend 82: 91-102.
- Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, et al. (1996) Mortality following inpatient addictions treatment: Role of tobacco use in a community-based cohort. JAMA: Journal of the American Medical Association 275: 1097-1103.
- Lisha NE, Carmody TP2, Humfleet GL2, Delucchi KL2 (2014) Reciprocal effects of alcohol and nicotine in smoking cessation treatment studies. Addict Behav 39: 637-643.
- Taylor B, Rehm J (2006) When risk factors combine: The interaction between alcohol and smoking for aerodigestive cancer, coronary heart disease, and traffic and fire injury. Addictive Behaviors 31: 1522-1535.
- Jarvis CM, Hayman LL, Braun LT, Schwertz DW, Ferrans CE, et al. (2007) Cardiovascular risk factors and metabolic syndrome in alcohol- and nicotine-dependent men and women. J CardiovascNurs 22: 429-435.
- Joseph AM, Willenbring ML, Nugent SM, Nelson DB (2004) A randomized trial of concurrent versus delayed smoking intervention for patients in alcohol dependence treatment. Journal of Studies on Alcohol, 65: 681-691.
- Kodl M, Fu SS, Joseph AM (2006) Tobacco cessation treatment for alcohol-dependent smokers: when is the best time? Alcohol Res Health 29: 203-207.
- Fu S, Kodl M, Willenbring M, Nelson D, Nugent S, et al. (2008) Ethnic differences in alcohol treatment outcomes and the effect of concurrent smoking cessation treatment. Drug and Alcohol Dependence 92: 61-68.
- Holt LJ, Litt MD, Cooney NL (2012) Prospective analysis of early lapse to drinking and smoking among individuals in concurrent alcohol and tobacco treatment. Psychology of Addictive Behaviors 26:561-572.
- Centers for Disease Control and Prevention (CDC) (2009) Cigarette smoking among adults and trends in smoking cessation - United States, 2008. MMWR Morb Mortal Wkly Rep 58: 1227-1232.
- Irving LM, Seidner AL, Burling TA, Thomas RG, Brenner GF (1994) Drug and alcohol abuse inpatients' attitudes about smoking cessation. J Subst Abuse 6: 267-278.
- Macnee CL, Talsma A (1995) Development and testing of the barriers to cessation scale. Nurs Res 44: 214-219.
- Orleans CT, Rimer BK, Cristinzio S, Keintz MK, Fleisher L (1991) A national survey of older smokers: treatment needs of a growing population. Health Psychol 10: 343-351.
- Kristeller JL (1994) Treatment of hard-core, high-risk smokers using FDA approved pharmaceutical agents: An oral health team perspective. Health Values 18: 25-32.
- Asher MK, Martin RA, Rohsenow DJ, MacKinnon S, Traficante R, et al. (2003) Perceived barriers to quitting smoking among alcohol dependent patients in treatment. Journal of Substance Abuse Treatment 24: 169-174.
- Martin RA, Rohsenow DJ, MacKinnon SV, Abrams DB, Monti PM (2006) Correlates of motivation to quit smoking among alcohol dependent patients in residential treatment. Drug Alcohol Depend 83: 73-78.
- Marlatt GA, Gordon JR (1985) Relapse prevention. New York: Guilford Press.
- Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N (1985) Decisional balance measure for assessing and predicting smoking status. J PersSoc Psychol 48: 1279-1289.
- DiClemente CC, Prochaska JO (1982) Self-change and therapy change of smoking behavior: a comparison of processes of change in cessation and maintenance. Addict Behav 7: 133-142.
- Curry SJ, Grothaus L, McBride C (1997) Reasons for quitting: intrinsic and extrinsic motivation for smoking cessation in a population-based sample of smokers. Addict Behav 22: 727-739.
- Baha M, Le Faou AL (2010) Smokers' reasons for quitting in an anti-smoking social context. Public Health 124: 225-231.
- Curry SJ, McBride C, Grothaus LC, Louie D, Wagner EH (1995) A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. J Consult Clin Psychol 63: 1005-1014.
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 88: 791-804.
- First MB, Williams JB, Spitzer RL, Gibbon M (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Clinical Trials Version (SCID-CT). New York: Biometrics Research, New York State Psychiatric Institute.
- Brown RA, Lejuez CW, Kahler CW, Strong DR (2002) Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol 111: 180-185.
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO (1991) The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict 86: 1119-1127.
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF (1994) Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addict Behav 19: 33-39.
- Fagerstrom KO, Heatherton TF, Kozlowski LT (1990) Nicotine addiction and its assessment. Ear Nose Throat J 69: 763-765.
- Filbey FM, Claus E, Audette AR, Niculescu M, Banich MT, et al. (2007) Exposure to the taste of alcohol elicits activation of the mesocorticolimbicneurocircuitry. Neuropsychopharmacology 33: 1391-1401.
- Fleming MF, Barry KL, MacDonald R (1991) The alcohol use disorders identification test (AUDIT) in a college sample. Int J Addict 26: 1173-1185.
- Cherpitel CJ (1995) Analysis of cut points for screening instruments for alcohol problems in the emergency room. J Stud Alcohol 56: 695-700.
- Macnee CL, Talsma A (1995) Predictors of progress in smoking cessation. Public Health Nurs 12: 242-248.
- Curry S, Wagner EH, Grothaus LC (1990) Intrinsic and extrinsic motivation for smoking cessation. J Consult Clin Psychol 58: 310-316.
- McBride CM, Pollak KI, Bepler G, Lyna P, Lipkus IM, et al. (2001) Reasons for quitting smoking among low-income African American smokers. Health Psychol 20: 334-340.
- Bonn-Miller MO, Zvolensky MJ (2009) An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addict 18: 409-416.
- Buckner JD, Zvolensky MJ, Schmidt NB (2012) Cannabis-related impairment and social anxiety: the roles of gender and cannabis use motives. Addict Behav 37: 1294-1297.
- Agrawal A, Budney AJ, Lynskey MT (2012) The co-occurring use and misuse of cannabis and tobacco: a review. Addiction 107: 1221-1233.
- Degenhardt L, Hall W, Lynskey M (2001) The relationship between cannabis use and other substance use in the general population. Drug Alcohol Depend 64: 319-327.
- Cohen J, Cohen P (1983) Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum.
- Cohen J, Cohen P, West SG, Aiken LS (2003) Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ US: Lawrence Erlbaum Associates Publishers.
- Lipkus IM, Feaganes JR, Green JD, Sedikides C (2001) The Relationship Between Attitudinal Ambivalence and Desire to Quit Smoking Among College Smokers. Journal of Applied Social Psychology, 31: 113-133.
- Wilson SJ, Creswell KG, Sayette MA, Fiez JA (2013) Ambivalence about smoking and cue-elicited neural activity in quitting-motivated smokers faced with an opportunity to smoke. Addict Behav 38: 1541-1549.
- Festinger LA (1957) A theory of cognitive dissonance. Evanston, IL: Row, Peterson.
- Markowitz LJ (2000) Smoker's perceived self-exemption from health risks. Psi Chi Journal of Undergraduate Research 5: 119-124.
- Jamieson P, Romer D (2001)What do young people think they know about the risks of smoking? In P. Slovic (Ed.), Smoking: Risk, perception, and policy (pp. 51-63). Thousand Oaks, CA US: Sage Publications, Inc.
- Schane RE, Glantz SA, Ling PM (2009) Social smoking implications for public health, clinical practice, and intervention research. American Journal of Preventive Medicine 37: 124-131.
- DaniJA, De Biasi M (2001) Cellular mechanisms of nicotine addiction. PharmacolBiochemBehav 70: 439-446.
- Nestler EJ (2005) Is there a common molecular pathway for addiction? Nat Neurosci 8: 1445-1449.
- Ehrman RN, Robbins SJ, Bromwell MA, Lankford ME, Monterosso JR, et al. (2002) Comparing attentional bias to smoking cues in current smokers, former smokers, and non-smokers using a dot-probe task. Drug Alcohol Depend 67: 185-191.
- Kerst WF, Waters AJ (2014)Attentional retraining administered in the field reduces smokers’ attentional bias and craving.
- Wiers RW, Rinck M, Kordts R, Houben K, Strack F (2010) Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction 105: 279-287.
- Raupach T, West R, Brown J (2013) The most "successful" method for failing to quit smoking is unassisted cessation. Nicotine Tob Res 15: 748-749.
- Korte KJ, Capron DW, Zvolensky M, Schmidt NB (2013) The Fagerström test for nicotine dependence: do revisions in the item scoring enhance the psychometric properties? Addict Behav 38: 1757-1763.