Tadahiko Tamura, Nobuyuki Ishikawa*, Sai-ichi Tanaka, Yuko Hayashi, Takeshi Miyamoto and Shizuya Saika
Department of Ophthalmology, School of Medicine, Wakayama Medical University, Kimiidera, Wakayama, Japan
- *Corresponding Author:
- Nobuyuki Ishikawa
Department of Ophthalmology, School of Medicine
Wakayama Medical University, Kimiidera
Wakayama, Japan
Tel: 81-73-447-2300
Fax: 81-73-448-1991
E-mail: niskw@wakayama-med.ac.jp
Received date: November 07, 2016; Accepted date: January 03, 2017; Published date: January 09, 2017
Citation: Tamura T, Ishikawa N, Tanaka SI, Hayashi Y, Miyamoto T, et al. (2017) Histopathological Analyses of the Differences in Foreign Body Cell Reactions against Intraocular Lenses According to the Period of Implantation. J Eye Cataract Surg 2:17. doi:10.4172/2471-8300.100017
Copyright: © 2017 Tamura T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
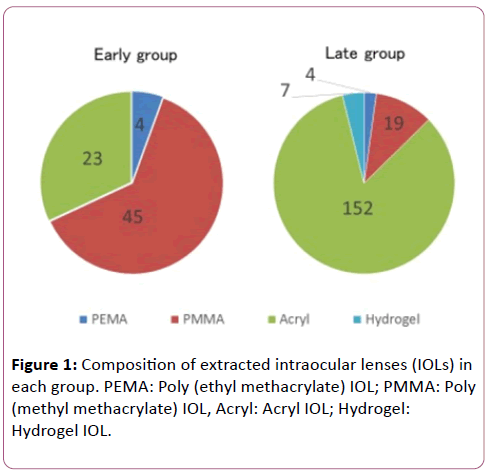
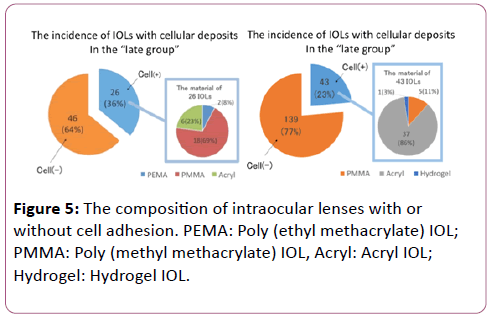
We examine if cell adhesion to the surface of an intraocular lens varies with the period of implantation. Samples of extracted intraocular lenses (IOLs) that had been implanted during 1987-2000 (n=72, early group) and those during 2001–2014 (n=182, late group) were included. IOLs were stained with hematoxylin and eosin and grouped according to the presence or absence of cellular deposits on the central area of the IOL anterior surface. Silicone IOLs were excluded because the silicone material does not adhere to cells. The early group included four poly( ethyl methacrylate) (PEMA) IOLs, 45 poly (methyl methacrylate) (PMMA) IOLs, and 23 acryl IOLs, and the late group included four PEMA IOLs, 19 PMMA IOLs, 152 acrylic IOLs, and seven hydrogel IOLs. Twenty-six of 72 samples (36%) in the early group and 43 of 182 IOLs (23%) in the late group were associated with cellular deposits in the central area of the IOL surface. The difference was statistically significant using the chi-square test. The number of IOLs with cell adhesions was less in the late group when compared with the early group.
Keywords
Intraocular lens; Implantation; Inflammation; Vision; Ophthalmology; Microscopy
Introduction
Advances in surgical instruments and the development of new materials for implanted intraocular lenses (IOLs) have resulted in a reduction of postoperative intraocular inflammation and an improvement of postoperative vision of patients.
Macrophages and giant foreign body cells adhere to the surface of implanted IOLs as a result of a foreign body reaction [1-4]. Cell adhesion to an implanted biomaterial can be regulated by the characteristic of the materials, but cellular adhesion to the surface of an IOL usually does not affect a patient’s vision. However, we experienced an impaired vision in a patient with massive cell adhesion related to uveitic inflammation [5,6] this case suggested that inflammation in the anterior chamber may affect the level of cell adhesion to an IOL. Macrophages on the IOL surface can also affect the behaviour of lens epithelial cells via secretion of growth factors that modulate fibrogenic reactions of the cells leading to capsular opacification [1-3].
It has been reported that cells can adhere to the surface of an IOL that has been in the eye for a long period [7]. However, there is no report of the possible differences in foreign body cell reactions against IOLs implanted in the eye for different lengths of time. The present study therefore analyzed the possible differences in foreign body cell reactions against IOLs according to the periods of implantation from 1987–2014 in the Japanese population. We examined changes of cell adhesions on IOLs without silicone optics, because the hydrophobic silicone material did not adhere to macrophages.
Materials
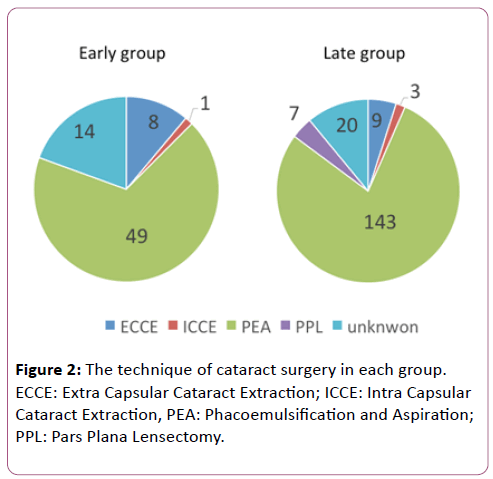
The study was approved by the institutional review board of Wakayama Medical University, Wakayama, Japan and consent of supplying the extracted IOL for investigations was obtained from each patient. Samples were obtained in Wakayama Medical University or in other hospitals and supplied in fixation solution of formalin to Department of Ophthalmology, Wakayama Medical University. A total of 254 samples of extracted nonsilicone IOLs were included in the study. The samples were divided into two groups according to the periods of implantation. Groups 1 and 2 included IOLs implanted between January 1, 1987–December 31, 2000 and January 1, 2001– December 31, 2014, respectively. There were 72 IOLs in group 1, and 182 IOLs in group 2. The types of IOLs in each group are listed in Figure 1 and the technique of cataract surgery in each group is listed in Figure 2.
Figure 1: Composition of extracted intraocular lenses (IOLs) in each group. PEMA: Poly (ethyl methacrylate) IOL; PMMA: Poly (methyl methacrylate) IOL, Acryl: Acryl IOL; Hydrogel: Hydrogel IOL.
Figure 2: The technique of cataract surgery in each group. ECCE: Extra Capsular Cataract Extraction; ICCE: Intra Capsular Cataract Extraction, PEA: Phacoemulsification and Aspiration; PPL: Pars Plana Lensectomy.
Methods
The extracted IOLs were stained with hematoxylin and eosin (HE) as previously reported [8]. The number of cells adhering to a central area 2 mm in diameter on the anterior surface of the IOL was determined using light microscopy. A giant foreign body cell was counted as one cell. The Fisher’s exact test and chisquare test were used to determine significant differences in the percentages of cell adhesion between the two groups.
Results
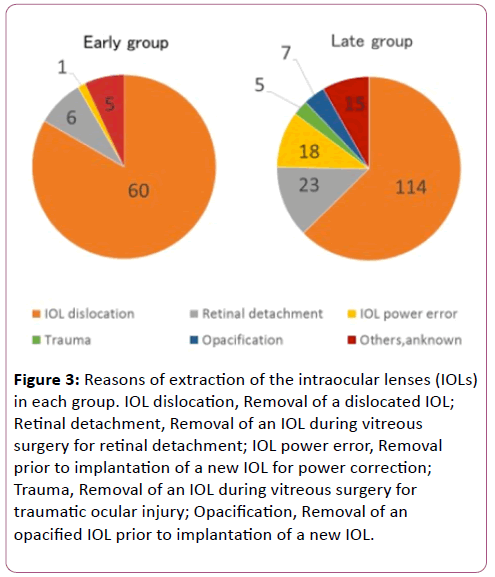
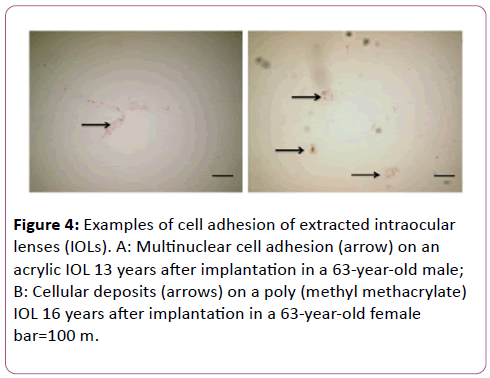
The percentage of acrylic IOLs with cell adhesions increased with increasing time. Figure 3 shows the reasons for the extraction of the implanted IOLs. The percentage of IOLs extracted because of dislocations, including luxation and subluxation, decreased, and the percentage extracted because of replacement of a new IOL to correct for refraction increased with increasing time. Figure 4 shows examples of cell adhesions observed on the IOL surface. In group 1, 26 IOL samples (36%) were associated with adhesion of macrophages. Detailed information of the IOLs with cell adhesions is shown in Figure 5. They involved two polyethylmethacrylate (PEMA) IOLs, 18 polymethylmethacrylate (PMMA) IOLs, and 6 acrylic IOLs. In group 2, 43 IOL (23%) were associated with adhesion of macrophages. They were five PMMA IOLs, 37 acrylic IOLs, and one hydrogel IOL. Using the chi-square test, there was a significant difference in the percentage of IOLs with cell adhesions between the two groups (p<0.05). As for the surgical technique, there was a significant difference in the percentage of IOLs with cell adhesions between the two groups in PEA group (p<0.05) but no significant difference in ECCE group (Tables 1 and 2). As for the type of IOL material, there was a significant difference in the percentage of IOLs with cell adhesions between the two groups in PMMA group (p<0.05) but no significant difference in Acryl group (Tables 3 and 4).
Figure 3: Reasons of extraction of the intraocular lenses (IOLs) in each group. IOL dislocation, Removal of a dislocated IOL; Retinal detachment, Removal of an IOL during vitreous surgery for retinal detachment; IOL power error, Removal prior to implantation of a new IOL for power correction; Trauma, Removal of an IOL during vitreous surgery for traumatic ocular injury; Opacification, Removal of an opacified IOL prior to implantation of a new IOL.
Figure 4: Examples of cell adhesion of extracted intraocular lenses (IOLs). A: Multinuclear cell adhesion (arrow) on an acrylic IOL 13 years after implantation in a 63-year-old male; B: Cellular deposits (arrows) on a poly (methyl methacrylate) IOL 16 years after implantation in a 63-year-old female bar=100 m.
Figure 5: The composition of intraocular lenses with or without cell adhesion. PEMA: Poly (ethyl methacrylate) IOL; PMMA: Poly (methyl methacrylate) IOL, Acryl: Acryl IOL; Hydrogel: Hydrogel IOL.
| |
Early Group |
Late Group |
| Cell(+) |
13 |
18 |
| Cell(-) |
36 |
125 |
Table 1: Comparison of the cell adhesion of IOLs in early group and late group in PEA group (chi-square test P=0.6372)
| |
Early Group |
Late Group |
| Cell(+) |
4 |
3 |
| Cell(-) |
4 |
6 |
Table 2: Comparison of the cell adhesion of IOLs in early group and late group in ECCE group (Fisher’s exact test P=0.6372)
| |
Early Group |
Late Group |
| Cell(+) |
14 |
4 |
| Cell(-) |
3 |
15 |
Table 3: Comparison of the cell adhesion of IOLs in early group and late group in PMMA group (Fisher’s exact test P=0.0006)
Discussion
The present study showed that the number of IOL samples that were associated with adhesion of macrophages extracted before the end of 2000 was greater when compared with those extracted after January 1, 2001. Cell adhesion to the surface of an IOL can be affected by two parameters, involving the physical characteristics of the material or the contact angle of the surface, and the level of inflammation in the anterior chamber [1-3]. The latter can be influenced by the presence of the diseases such as diabetes or uveitis. Postoperative inflammation can be controlled by topical administration of anti-inflammatory drugs, and improvements in surgical procedures could be one of the major reasons for less inflammation in the anterior chamber after surgery [9-11]
Excess adhesion of cells of macrophage origin to the IOL surface could promote capsular fibrosis via growth factor expression by the cells. Evaluation of the degree of cell adhesion to an implanted IOL could therefore be a marker for evaluation of the invasiveness of the procedure to ocular tissues.
References
- O'Brien TP (2003) Advances in intraocular lens materials and designs:maximizing biocompatibility and optical performance. Ophthalmologica 217: 5-18.
- McCulley JP (2003) Biocompatibility of intraocular lenses. Eye Contact Lens 29: 155-163.
- Werner L (2008) Biocompatibility of intraocular lens materials. Curr Opin Ophthalmol 19: 41-49.
- Saika S (2004) Relationship between posterior capsule opacification and intraocular lens biocompatibility. Prog Retin Eye Res 23: 283-305.
- Tamura M, Kanagawa R, Saika S (1990) Comparison of the cellular response on intraocular lenses implanted in rabbit eyes with and without extracapsular lens extraction. J Cataract Refract Surg 16: 746-750.
- Taravati P, Lam DL, Leveque T, Van Gelder RN (2012) Postcataract surgical inflammation.Curr Opin Ophthalmol 23: 12-18.
- Saika S, Miyamoto T, Yamanaka A (1998) Immunohistochemical evaluation of cellular deposits on posterior chamber intraocular lenses. Graefe’s Arch Clin Exp Ophthalmol 236: 758-765.
- Ishikawa N, Miyamoto T, Okada Y, Saika S (2011) Cell adhesion on explanted intraocular lenses: part 1: analysis of explanted IOLs. J Cataract Refract Surg 37: 1333-1338.
- Barbour W, Saika S, Miyamoto T, Ohnishi Y (2005) Biological compatibility of polymethyl methacrylate, hydrophilic acrylic and hydrophobic acrylicintraocular lenses. Ophthalmic Res 37: 255-261.
- Okajima Y, Saika S, Sawa M (2005) Effects of surface modification of intraocular lenses on foreign body reaction. Nippon Ganka Gakkai Zasshi 109: 267-273.
- Yao K, Huang XD, Huang XJ, Xu ZK (2006) Improvement of the surface biocompatibility of silicone intraocular lens by the plasma-induced tethering of phospholipid moieties. J Biomed Mater Res A 78: 684-692.