- (2006) Volume 7, Issue 3
Miguel Perez-Mateo
Department of Internal Medicine, Gastroenterology Unit, Hospital General Universitario de Alicante, Miguel Hern?ndez University. Elche, Alicante, Spain
Alcoholism; carbohydratedeficient transferrin; Cholelithiasis; Diagnosis; Liver Function Tests; Pancreatitis, Acute Necrotizing /etiology
AP: acute pancreatitis; CDT: carbohydrate-deficient transferrin
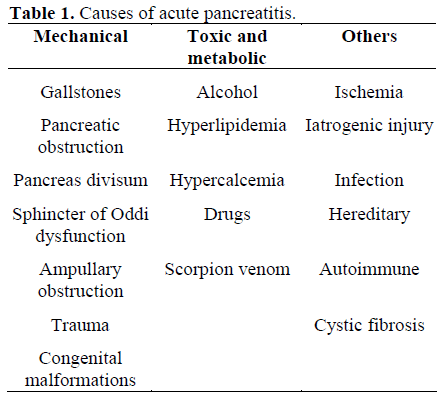
Acute pancreatitis (AP) is a frequent disease which represents 0.15-1.5% of all diagnoses in the emergency room. Although its prevalence varies in different countries and even in different areas of a given country, it is likely that its real prevalence ranges from 200-300 cases per million inhabitants a year [1, 2, 3]. The list of etiologic factors related to its development is shown in Table 1. However, a biliary origin is by far the most frequent cause, followed by an alcoholic origin. Together these etiologies are responsible for 80% of all episodes of AP [4]. In a published series, each one of the remaining possible etiologic causes affected a reduced number of patients with AP.
From a clinical perspective, the characteristics of the episodes of AP having different etiologies are similar and indistinguishable from one another. Modern diagnostic tools permit the identification of the etiology in most cases, and the acronym “idiopathic” has become rare [5]. However, many of these new techniques may not be available in all hospitals, and some of them are restricted to academic hospitals. Furthermore, although the basic clinical characteristics of all episodes are similar, the suspicion of a biliary origin in a patient with severe AP or associated cholangitis may require an ERCP to confirm choledocolithiasis and the removal of the stone. This maneuver improves the clinical evaluation of the patient [6]. Similarly, the identification of the alcoholic origin of an episode of AP, this being the second cause of AP, is relevant in order to decrease expenses, and avoid the use of non-necessary diagnostic tools. In this regard, it is well-known that information obtained by asking the patient or his/her relatives is rarely accurate [7] and questionnaires developed to estimate the intake of alcohol have a low sensitivity and specificity (60-95% and 40-95% respectively) [8].
The association of certain abnormalities in liver function tests in the first days of an episode of AP and biliary etiology were described more than 30 years ago [9]. Since then, different studies intended to design an easy-to-use, reliable and cheap method of identifying the biliary origin of episodes of AP confirmed that these episodes showed levels of AST, ALT, alkaline phosphatase and total bilirubin statistically significantly higher than episodes of AP of a non-biliary origin [10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20].
These studies were included in a metaanalysis [21] which showed that transaminsases are more useful in detecting the biliary origin of AP than the other parameters reported. According to this research, values of transaminases 3 times the upper normal limit show a positive predictive value of 95% for the diagnosis of biliaryinduced AP. Similarly, in order to design a multifactorial predictive system, we have investigated the behavior of different biochemical parameters in a series of 45 cases of AP (33 of biliary origin and 12 of alcoholic origin) [22]. The logistic regression analysis performed based on 4 variables (age, sex, Creactive protein on day 1 and ALT on day 2) accurately predicted the etiology in 97.7% of all cases (44 out of 45 cases), and estimated the likelihood of biliary origin by the application of a mathematical formula.
Thereafter, the introduction of new diagnostic tools raised doubt as to the usefulness of liver function tests in predicting the biliary origin of AP. A seminal study from Ros et al. [23] in a series of 51 patients with “idiopathic” AP reported that age, previous repetitive episodes of AP and abnormal liver function tests were significantly related to the presence of biliary microlithiasis. Grau et al. [24] obtained similar results by examining the bile from 91 patients with “idiopathic” AP. ALT analyzed in the first 24 hours after admission (cut-off equal to 1.2 times the upper normal limit) showed a sensitivity of 73%, a specificity of 86% and a PPV of 92% in predicting the presence of microlithiasis.
Recently, endoscopic ultrasound (EUS) has become the most accurate technique for detecting chole- and choledocolithiasis [25]. Hence, several authors have re-evaluated the role of biochemical abnormalities for predicting a biliary etiology in episodes of AP. Ammori et al. [26] reported a sensitivity, specificity, PPV and NPV for liver function tests of 91, 100, 100 and 85%, respectively. When combining this evaluation with EUS, these values reached 98, 100, 100 and 96% respectively. Two similar studies published recently reached similar conclusions. Liu et al. [27] (Hong Kong) performed EUS in a series of 139 patients with AP in the first 24 hours after admission and identified the etiology in all cases. Therefore, the sensitivity of EUS for identifying the biliary origin of AP was 100%. Multivariate analysis disclosed that female sex, age over 58 years, and ALT greater than 150 U/L became independent predictors of biliary origin. With these three factors, the sensitivity was 93% and overall accuracy was 80%. Similar results were obtained by Levy et al. [28] in a multicenter study performed in France and Switzerland. Patients who had a normal abdominal ultrasound underwent EUS. Using this diagnostic approach only 14 patients (7%) remained in the group of “idiopathic” AP. Again, female sex, increased age and increased ALT levels at admission were considered independent predictive variables of biliary origin in the multivariate analysis. The likelihood of biliary origin might be estimated with the formula 1 / (1+exp(4.6967 - 0.0656 x age [years] - 0.6909 x ALT [times of the upper limit of the reference range] + 1.1208 x sex [1 for men, 0 for women]).
Information obtained from recent studies reinforces the idea that early determination of liver function tests still constitutes a valid method for predicting the biliary origin of AP. Traditionally, certain biochemical parameters such as GGT and MCV have been considered in identifying alcoholic etiology of AP episodes. However, it has been shown that these parameters are not useful in distinguishing AP episodes of alcoholic origin from those of other origins [29]. Other studies reported that an increased lipase/amylase ratio is characteristic of AP episodes of alcoholic origin. Gumaste et al. [30] reported that the lipase/amylase ratio has a sensitivity of 91% for detecting the alcoholic origin of AP. In the study by Tenner and Steinberg [31], only alcohol-induced AP showed a lipase/amylase ratio higher than 5 (specificity of 100%, although with a low sensitivity of 31%). However, other investigations reported that the ratio quoted was not useful in differentiating alcoholic from non-alcoholic AP [13, 29, 32, 33]. It has also been reported that both an increase in the plasmatic activity of trypsin [33] or a trypsin-2-alpha1- antitrypsin/trypsinogen-1 ratio [34] correctly identified an alcoholic origin. Our group reported that levels of serum trypsin activity are significantly higher in patients with episodes of AP of alcoholic origin when compared with episodes of other etiologies [35].
The measurement of carbohydrate-deficient transferrin (CDT) may detect an excessive consumption of alcohol [36] and it has been used to detect the alcoholic origin of AP. Jaakola et al. [29] showed that levels of CDT higher than 17 U/L show a 27% sensitivity and 100% specificity in the detection of an alcoholic origin. Our group reported similar results in a group of 70 patients with AP [35]. Furthermore, multivariate analysis of all the parameters evaluated in this investigation, age less than 44 years, plasma CDT greater than 22.5 U/L and trypsin activity greater than 152 U/L correctly identified the alcoholic origin in 98% of the episodes; these results are similar to data published elsewhere [37].
In summary, by means of simple biochemical studies, it is possible to correctly predict the biliary or alcoholic origin of AP episodes in approximately 80% of cases when performed in the first hours after admission. However, a biliary origin needs to be confirmed with imaging techniques before considering any specific form of therapy. The negativity of these markers should suggest investigating other possible etiologic factors with specific analytical or morphological tests.