- (2016) Volume 0, Issue 0
Cherif Boutros1,2*, Lance Uradomo1,2, Mukul Khandelwal2, Harvinder Singh2, Russell DeLuca2, Yudhishtra Markan2 and Alan Morrison2
1University of Maryland School of Medicine, Baltimore
2University of Maryland Baltimore Washington Medical Center, Tate Cancer Center, Glen Burnie
Received: November 25th, 2015 Accepted: January 25th, 2016
Introduction Despite the decrease in operative mortality of pancreaticoduodenectomy over last decades, operative morbidity remains high and overall survival is still poor. As such, minimally invasive surgery for periampullary malignancy is generally considered of limited value. We assessed the role of a hybrid minimally invasive approach in patients treated for early clinical stage pancreatic and periampullary cancer and analyzed operative and short-term surgical outcomes. Methods We conducted a retrospective analysis of a prospectively maintained hepatobiliary database under IRB approval. All patients who received robotic assisted pancreaticoduodenectomy for pancreatic or periampullary malignancies were included. The surgical approach consisted of a laparoscopic portion including exploration, cholecystectomy, kocherization of the duodenum, mobilization and division of the stomach and intestine. This was followed by robotic dissection of the hepatoduodenal ligament, pancreatic neck and peripancreatic lymph nodes. Finally a mini laparotomy was used to divide the pancreas and perform the reconstruction. Patients’ demographics, operative data, pathology results and short-term outcomes were analyzed. Results Eleven consecutive patients, underwent surgery for clinical stage I and II biopsy proven pancreatic head adenocarcinoma (n=8), neuroendocrine carcinoma (n=2) and duodenal gastrointestinal stromal tumor (n=1). Average operative time was 475 minutes. Average estimated blood loss was 375 mL; there was no perioperative or 90 days mortality. 27% of patients received perioperative blood transfusions. There were no grade B/C pancreatic fistulas. Mean hospital length of stay was seven days and readmission rate was 27%. Pathological examination of the specimen revealed 100% R0 resection with an average lymph node retrieval of 14. Conclusion The hybrid approach is safe and may be an acceptable introduction for a totally robotic pancreaticoduodenectomy. It offers the patients the advantages of a minimally invasive approach, maintains the classical surgical reconstruction phase and provides a flexible platform for the surgeon to gradually integrate the robotic technique.
Minimally invasive surgical procedures; Pancreatic Neoplasms; Pancreaticoduodenectomy; Robotics; Surgery
Over the last decades, a paradigm shift has occurred imposing the application of minimally invasive approach to a variety of surgical procedures. The main advantages of the minimally invasive approach are: less operative blood loss, shorter length of stay, reduced postoperative pain and use of narcotics, and earlier recovery. With time and experience, limitations to the minimally invasive approach became less restrictive. At the same time, the indications became broader, including procedures traditionally reserved for the open approach. As such, pancreatic surgery performed for malignant or borderline/premalignant lesions, dictating onco-pathological resectional parameters, (exposure, resection margins, and regional lymph nodes dissection) are currently performed through small trocar incisions in an increasing number of surgical centers. Moreover, the minimally invasive approach can expand surgical indications to borderline patients otherwise considered poor surgical candidates.
Although laparoscopic pancreaticoduodenectomy was reported in 1994, [1]. Two years before laparoscopic distal pancreatectomy, fewer series have discussed the role and the results of laparoscopic pancreaticoduodenectomy. The reasons are obvious: dissection in laparoscopic distal pancreatectomy is relatively easy, the technique is similar to the open approach, and there is no reconstruction.
In addition to laparoscopic distal pancreatectomy, multiple different techniques have been reported including total laparoscopic, total robotic, robotic assisted laparoscopy, hand assistance, and open reconstruction. Selection criteria were poorly reported, and no prospective or randomized studies have been published.
We started a robotic assisted pancreaticoduodenectomy program in 2012. Our goal was to safely and gradually introduce the robotic technique to maximize the benefits of the minimally invasive approach without compromising the patient outcome that may be affected by a learning curve. The current study reports the early results of this approach.
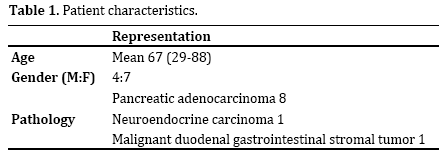
All patients undergoing robotic assisted pancreaticoduodenectomy for malignant indications over two-year period (2012-2014) were identified from a prospectively maintained surgical oncology/ hepatopancretobiliary database, with institutional review board approval. Patients who had their procedure aborted for intraoperative findings of metastatic disease, or with pancreatitis or intraductal papillary mucinous neoplasm as the final pathologic diagnosis were excluded. Patients who had only laparoscopic assistance were excluded. The procedure was offered to patients with clinically early stage pancreatic head cancer (Stage I-II) or periampullary malignancy. Patients who received neoadjuvant chemoradiation therapy or with a history of prior upper abdominal laparotomy were not offered the minimally invasive approach. All included patients underwent a hybrid pancreaticoduodenectomy consisting of laparoscopic, robotic, and a mini laparotomy parts. Patient characteristics are reported in Table 1.
The included patients represent a highly selected group. All patients were preoperatively discussed on a multidisciplinary tumor board. A computed tomography scan of the abdomen with intravenous contrast, pancreatic protocol, was obtained for all patients. Positron emission tomography was obtained to exclude metastatic disease. Patients meeting radiological criteria for early stage, resecTable pancreatic or periampullary malignancies were offered the minimally invasive hybrid approach. We did not offer the hybrid approach to patients who received neoadjuvant chemoradiation because of the expectation of excessive fibrosis in the periportal and pancreatic neck area substantially increasing the difficulty of the minimally invasive approach more difficult. Similarly, we did not offer the hybrid approach to patients with previous upper abdominal laparotomy due to expected postoperative adhesions. As such, this group of highly selected patients represents about only 20% of patients who underwent surgical resection for periampullary malignancy during the same period.
The patient is positioned in supine position on a beanbag, with the arms tucked to the sides and the lower extremities on stirrups to allow the surgeon to stand between the patient legs (French position). Pneumoperitoneum to 15 mm Hg is obtained through a 12 mm infraumbilical trocar followed by placement of two 5 mm trocars in the right and left upper quadrants. After exploration of the abdominal cavity to rule out metastatic disease, the round and falciform ligaments are resected and buttress a percutaneous trans hepatic 3/0 nylon U stich on a Keith needle. The U stich is placed on the left lateral lobe of the liver to allow its retraction and exposure to the gastrohepatic ligament. The lesser sac is accessed by dividing the gastrocolic ligament, the plan of dissection is pursued to the right dissecting and dividing the right gastroepiploic vessels then mobilizing the right hepatic colic flexure and the distal right colon along the line of Todd. Careful exploration of the lesser sac and the root of the transverse mesocolon is conducted to rule out peritoneal metastatic deposit. Two 8mm da Vinci Robotic cannulas are then placed in the right and left per umbilical area. A laparoscopic cholecystectomy is then conducted. The robotic time then starts using da Vinci S surgical system (Intuitive Surgical®). The right hand is instrumented with da Vinci Maryland bipolar forceps while the left hand is instrumented with a da Vinci fenestrated forceps. The patient cart is docked from head position. Kocherization of the duodenum is then performed, and the superior mesenteric vein portal junction is dissected from the lower border of the pancreatic neck. A tunnel is then bluntly dissected using a laparoscopic peanut dissector over the portal vein. The gastroduodenal ligament is dissected. The gastroduodenal artery is divided between hem-olock clips. The common bile duct is dissected and the hepatoduodenal lymphovascular tissue is dissected to be part of the resected specimen. The distal stomach as well as proximal jejunum approximately 10 cm from the ligament of Treitz are divided using endomechanical staplers. The divided Jejunum that will be used for reconstruction is marked with a 0/3 silk suture that is kept long to facilitate its retrieval during the eventual mini laparotomy. The proximal Jejunum is then dissected proximally along its mesenteric border using a radiofrequency energy sealing and cutting device. The ligament of Treitz is divided, and the line of dissection is pursued to meet the previously created plane from the Kocher maneuver, allowing a recuperation of the whole duodenum and proximal jejunum on the right side.
At this point a 10 cm mini upper midline laparotomy is created, centered over the pancreatic neck. The pancreatic neck is divided using electrocautery after controlling the pancreaticoduodenal arcades with 0/3 prolene sutures. The uncinate process is dissected from the portal vein with control and division of direct uncinate process venous tributaries to the portal vein. The superior mesenteric artery can be easily skeletonized if needed to assure negative margins, and the pancreaticoduodenal arterial branches are divided using energy based sealing and cutting device or endomechanical stapler. Finally, the bile duct is divided and the specimen is sent for frozen section evaluation of the uncinate, portal vein surface, pancreatic duct and bile duct margins.
After confirmation of achieving negative margins, the reconstruction phase (child’s reconstruction) is performed. Two #19 Blake drains are placed thru the 5mm right and left upper quadrant trocars to drain the pancreaticojejunostomy and the choledocojejunostomy. A well-vascularized pedicle of omentum is fashioned to wrap the pancreaticojejunostomy. The patients are usually extubated on the Table and transferred to the intensive care unit for postoperative care.
The patient is encouraged to sit on the chair the day of the surgery and ambulate on the first postoperative day assisted by the physical therapy service. Our protocol is to maintain the left Blake draining the pancreaticojejunostomy until the patient tolerates a regular oral diet and the drain has minimal output (<50 mL/24 hrs). We do not routinely measure the amylase content of the drain output before the drain removal. It is usually left in place to be followed in an outpatient basis. The nasogastric tube is removed on the second postoperative day and the patient start on sips of clears advanced as tolerated to a solid diet.
Estimated blood loss (EBL), transfusion requirements, postoperative length of stay (LOS), and complications were assessed. Oncologic data including final pathology, negative margin and number of lymph node retrieval were checked. Data was recorded in a Microsoft Excel (Microsoft, Redmond, WA) database.
Eleven patients underwent a hybrid robotic assisted pancreaticoduodenctomy for pancreatic and periampullary malignancy, Table 2. The average operative time was 475 minutes (mns) (420-526 mns). The average estimated blood loss was 375 mL and three patients (27%) required perioperative blood transfusion. There was no perioperative mortality and the average hospital length of stay was seven days (range 4-16 days). Two patients had LOS longer than10 days. One patient with a postoperative ileus, and the other was an 88 year old with concurrent trimalleolar fracture. The readmission rate was 27%. Three patients were readmitted, one for diarrhea related to clostridium difficile infection and two for poor oral intake and dehydration requiring intravenous access and rehydration.

Postoperative complications included postoperative ileus (n=1) and clostridium difficile infection (n=1). Pancreatic fistula is defined and graded according to the international study group on pancreatic fistula definition [2]. There were no Grade B/C pancreatic fistulas. Final pathology demonstrated pancreatic adenocarcinoma (n=8), pancreatic neuroendocrine tumor (n=2), and duodenal gastrointestinal stromal tumor (GIST) (n=1). All patients had an R0 resection (100% negative margins), and none required reoperation. Average lymph node retrieval was 14 (range 6-17). There was no 90-day mortality. Regarding the eight patients with pancreatic adenocarcinoma, final pathological stage was IA (n=1), IB (n=1), and IIB (n=6). During the follow up period (mean follow up 20 months), three patients developed metastatic disease and subsequently died, while five patients are alive with no evidence of disease recurrence.
Minimally invasive pancreaticoduodenectomy remains a challenging procedure. The technically demanding minimally invasive approach is generally felt to have limited value for malignant pancreatic malignancy. The traditional benefits of a minimally invasive approach, namely less postoperative pain, early recovery and shorter length of stay are masked by the overall prognosis of the aggressive underlying tumor biology. Pure laparoscopic approach is technically demanding specially in soft pancreas with small pancreatic duct. Robotic surgery is meant to be ergonomically appealing for surgeons, but the lack of tactile feedback and the long learning curve may limit its adoption by a large number of pancreatic surgeons.
The hybrid approach described here provides the advantage of a minimally invasive approach with smaller incision, early recovery and shorter length of stay while allowing the surgeon to perform the reconstruction part with a traditional open approach under direct vision and tactile feedback. The laparoscopic part - “the tango” - allows exploration of the abdominal cavity moving rapidly and smoothly in different abdominal fields without having to change camera position or re-docking robotic arms. The robotic part - “the slow” - allows a meticulous dissection and lymph node retrieval in a narrow field with intimate contact with tissues. Finally the "rock and roll” is the portion that allows the surgeon to perform the dissection of the uncinate process from the portal vein and superior mesenteric artery, achieving the negative margin, and perform the reconstruction with a full tactile feed back.
Seventeen years after its first report, a review of 285 patients from different published series who underwent laparoscopic pancreaticoduodenectomy was published [3] with only four studies that included more than 25 patients. This low number of highly selected patients limits our ability to generalize the results of this approach and clearly showed that it did not gain popularity. Nevertheless, the results of these four studies (n=166) revealed a mean operative time of 340 mns, average blood loss of 180 mL, mortality rate of 2% and mean length of stay (reported only in two studies) of seven and 19 days. It was obvious from these data that few centers were able to adopt this technique for highly selected patients.
Most recently, a single study reported a series of 100 consecutive laparoscopic pancreaticoduodenectomy [4]. In addition to its large size, this study provided an important contribution in that it discussed the crucial element of the learning curve. In this series, the complication rate decreased from 33.3% for the first 33 cases to 17.6% for the last 34 cases. Similarly, operative time decreased from 9.8 hours to 6.6 hours, respectively. The mean hospital stay was 14 days, which also decreased from 20.4 days for the first 33 cases to 11.5 days for the last 34 cases. For the 12 patients in the study cohort with invasive malignant disease, the median tumor size was 2.8 cm, and the median number of lymph nodes harvested was 13. All the patients had margin-negative R0 resections.
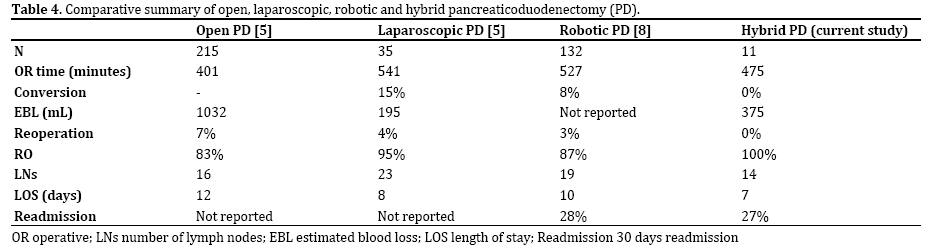
A retrospective comparison study between open (n=215) and laparoscopic pancreaticoduodenectomy (n=35) was published from Mayo clinic [5]. In this study operative blood loss and overall hospital stay were significantly less in the laparoscopic pancreaticoduodenectomy group (195 ml vs. 1000 mL, 8 days vs. 12 days; respectively). At the same time, operative time was significantly longer in the laparoscopic pancreaticoduodenectomy group (541 mns vs. 401 mns). Among malignant cases, tumor size was similar, and the number of retrieved LN was higher in the laparoscopic pancreaticoduodenectomy group (23 vs. 16).
Our study had a 100% R0 resection with a short length of stay of 7 days and average of 14 lymph nodes and operative time of 475 (shorter than a pure laparoscopic approach). The results of our study showed that we could achieve all benefits of a minimally invasive approach through an easily adopted hybrid approach.
The need for a better minimally invasive approach facilitated the introduction of robotic pancreaticoduodenectomy.
Subsequently, multiple studies reported the feasibility and safety of robotic pancreaticoduodenectomy in highly selected patients. Again, as with laparoscopic distal pancreatectomy studies, the selection criteria were poorly defined. Initial experience is well reported in two studies that included more than 50 patients [6, 7]. The total number of patients included in these two studies was 110 patients, conversion rate was 31%, operative time 487 minutes, operative blood loss 327 ml, pancreatic fistula rate 31- 22%, hospital length of stay (22, 10 days) and mortality of 2%.
Most recently, a single institution review of robotic pancreatic surgery from Pittsburgh [8] included the largest number of robotic pancreaticoduodenectomy patients. In this study, 132 patients received robotic pancreaticoduodenectomy mainly (80%) for malignant lesions. Operative time was 527 minutes ± 103. Conversion rate was 8.3% and reoperation rate was 3%. The mean length of hospital stay was 10 days with readmission rate of 28%. Among cancer patients R0 resection was achieved in 87% of cases and average lymph node retrieval was 19. The two most important points from this study are: First, he trend of increasing robotic pancreaticoduodenectomy over four years period, replacing the laparoscopic approach and exceeding the open approach in 2012. Second is the effect of learning curve experience in reducing the grade III-V complications rate after 88 robotic pancreaticoduodenectomy [27 of 88 (30%) vs. 6 of 44 (16%); P < 0.05].
Our hybrid approach offers less operative time than purely robotic surgery with similar decrease in LOS and similar readmission rate. Most importantly, the hybrid approach can be adopted by a laparoscopic surgical oncologist to achieve these results with early experience and provide a safe, reproducible platform for the surgeon to increase the robotic component of the procedure if needed.
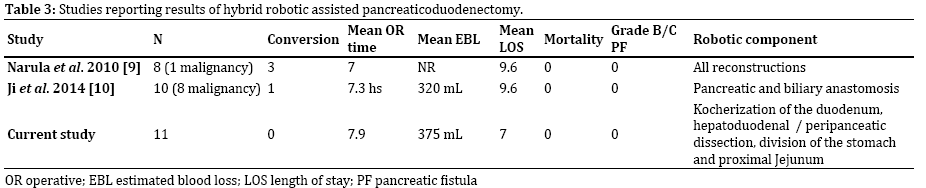
Previous studies reporting early results of hybrid robotic pancreaticoduodenectomy are listed on Table 3. The main difference between our current study and previous reports that we elected to perform the reconstruction phase in the open portion of the procedure.
It is clear that laparoscopic pancreaticoduodenectomy failed to be adopted in most surgical centers, likely due to the complexity of the procedure and the reconstructive phase. On the other hand, robotic pancreaticoduodenectomy is rapidly gaining popularity in high volume pancreatic surgery centers among highly specialized surgeons. However, three points need to be emphasized; First, all these reports of robotic pancreaticoduodenectomy showed the feasibility and safety of this new technology but fail to clearly improve the outcome of this complex procedures compared to the traditional open approach. Second, selection criteria of patients to be candidates for robotic pancreaticoduodenectomy need to be better defined and should include more factors beyond BMI, previous abdominal surgery such as pancreatic and bile duct size and the firmness of the pancreatic parenchyma. Third, the extensive learning curve for this complex procedure limits its application in most of the pancreatic surgery centers. A more simplified technique needs to be created to make robotic pancreaticoduodenectomy a reproducible procedure. A summary of results of studies reporting experience in open, laparoscopic, robotic pancreaticoduodenectomy with the current hybrid approach is reported on Table 4. To be noted, that these studies include a heterogeneous group of patients with different stage of pancreatic cancer, BMI and different selection criteria [9, 10].
This report represents our first experience in hybrid robotic surgery. Based on these results we are planning to introduce more technical robotic time to the hybrid pancreaticoduodenectomy. As the reconstruction phase is the Achilles heel of the pancreaticoduodenectomy, a robotic reconstruction may be added for a selected group of patient with firm pancreatic parenchyma and dilated pancreatic and bile ducts.
We advocate that our hybrid approach with laparoscopic, robotic and open components - “the Tango, Slow and Rock and roll” - is a good model to begin the integration of robotic pancreaticoduodenectomy in a higher number of pancreatic surgery centers.
Authors declare no conflict of interests for this article.