Kaori Yoriki*, Taisuke Mori, Hiroshi Matsushima, Takuro Yamamoto, Tetsuya Kokabu and Jo Kitawaki
Department of Obstetrics and Gynecology, Kyoto Prefectural University of Medicine, Kyoto, Japan
*Corresponding Author:
Kaori Yoriki, MD
Department of Obstetrics and Gynecology, Kyoto Prefectural University of Medicine
Graduate School of Medical Science, 465 Kajii-cho, Kawaramachi-Hirokoji, Kamigyo-ku, Kyoto, 602-8566, Japan
Tel: +81-75-251-5560
Fax: +81-75-212-1265
E-mail: kaorix26@koto.kpu-m.ac.jp
Received date: April 26, 2019; Accepted date: May 09, 2019; Published date: May 13, 2019
Citation: Yoriki K, Mori T, Matsushima H, Yamamoto T, Kokabu T, et al. (2019) Idiopathic Granulomatous Inflammation Presenting as a Malignant Tumor-like Mass in the Uterine Cervix: A Case Report. Gynecol Obstet Case Rep Vol 5:76. doi: 10.21767/2471-8165.100076
Keywords
Granulomatous inflammation; Bulky mass; Uterine cervix; Cervical cancer; Expectant management
Introduction
A granulomatous inflammatory response is a particular type of chronic inflammation characterized by focal clusters of macrophages along with epithelioid and multinucleated giant cells [1]. Although this inflammatory response, induced by various chemical mediators of cell injury, can occur in patients of any age group and involve any tissue [2], it is rarely observed in the uterus. There are a few reports of cervical granulomas detected incidentally during postoperative histopathological examination of extracted cervical or uterine tissue, in conjunction with cervical dysplasia or neoplasia [3]. A granulomatous inflammatory response is triggered by various infectious, autoimmune, toxic, allergic, drug-induced, and neoplastic conditions [4]. A combination of distinct clinical, radiological, and histological features allow for a definitive diagnosis and effective patient care [2]. However, it is difficult to rule out a differential diagnosis of cancer when the granulomatous inflammatory reaction leads to the formation of a bulky mass that resembles a malignant tumor. Additionally, the selection of a course of treatment is difficult when the definitive cause cannot be identified. Herein, we report our experience with the diagnosis and successful expectant management of a patient with extensive and idiopathic granulomatous inflammation that manifested with a malignant tumor-like mass in the uterine cervix.
Case Report
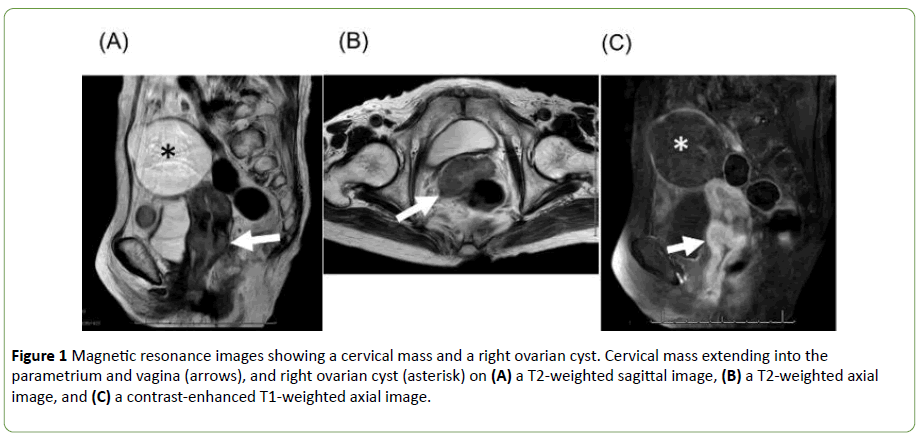
An 88-year-old postmenopausal woman (gravida 3 para 2) presented to our gynecology department with a complaint of abnormal vaginal bleeding. She had no history of diabetes, autoimmune disease, tuberculosis, or allergies, and she was not on any regular medication. On direct vaginal examination (using a speculum) and colposcopy, a mass was detected that appeared to extend from the cervix to the vaginal wall with tissuedamaging effects. Laboratory blood test results showed a total leucocyte count of 7.2 × 109 cells/L with 77.7% neutrophils and 13.4% lymphocytes. The C-reactive protein level was 20.0 mg/L. The levels of tumor markers other than carcinoembryonic antigen (6.0 μg/L) were within normal limits. Magnetic resonance imaging (MRI) revealed a 5.6 cm × 2.8 cm cervical mass extending into the left parametrium and the lower vagina (Figure 1).
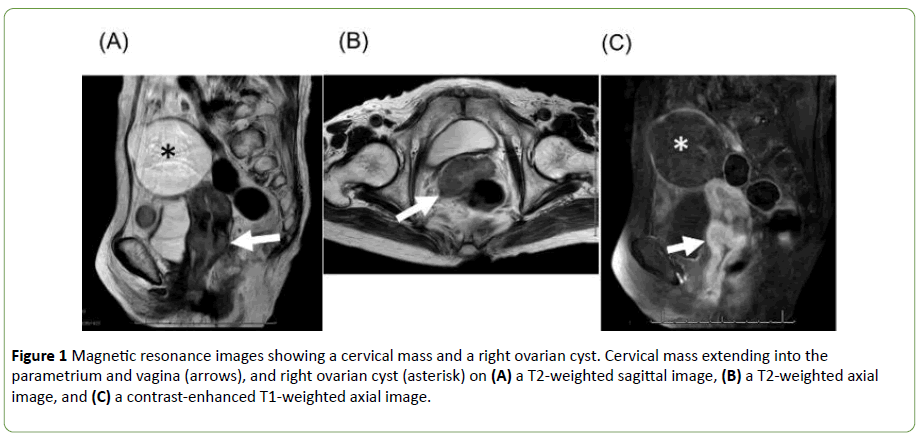
Figure 1: Magnetic resonance images showing a cervical mass and a right ovarian cyst. Cervical mass extending into the parametrium and vagina (arrows), and right ovarian cyst (asterisk) on (A) a T2-weighted sagittal image, (B) a T2-weighted axial image, and (C) a contrast-enhanced T1-weighted axial image.
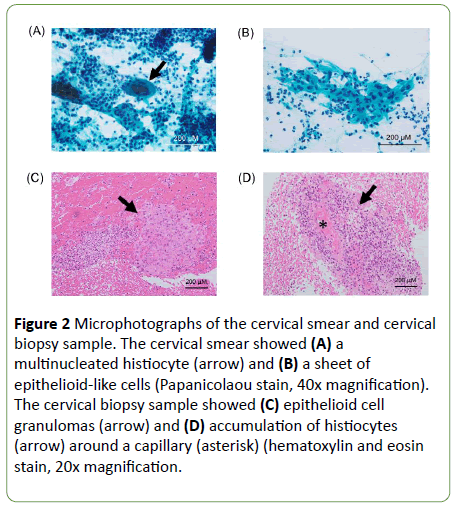
The mass showed an intense contrast-enhancement and a moderate intensity on T1- and T2-weighted MRI, respectively. MRI further revealed a 7 cm right ovarian cyst. Contrast-enhanced computed tomography (CT) of the patient’s chest and abdomen showed no swollen lymph nodes or signs of tuberculosis. Considering the clinical symptoms and imaging findings, we had suspected a diagnosis of squamous cell carcinoma (SCC) or tuberculosis. However, although the initial cervical smear was suspected to indicate SCC or other malignant neoplasms, the re-examined smear was negative for intraepithelial lesion or malignancy (NILM). Instead, clumps of multinucleated histiocytes and epithelioid-like cells were observed against a background of several inflammatory cells such as neutrophils (Figures 2A and 2B).
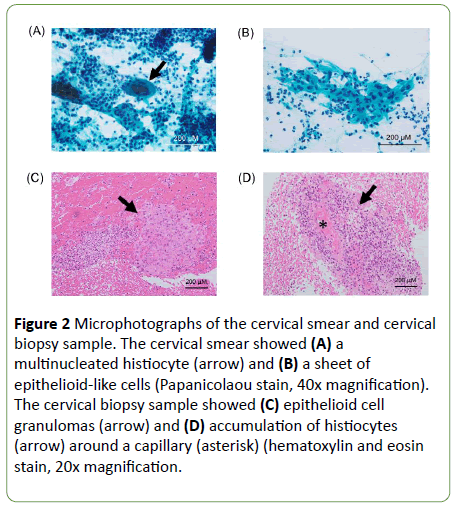
Figure 2: Microphotographs of the cervical smear and cervical biopsy sample. The cervical smear showed (A) a multinucleated histiocyte (arrow) and (B) a sheet of epithelioid-like cells (Papanicolaou stain, 40x magnification). The cervical biopsy sample showed (C) epithelioid cell granulomas (arrow) and (D) accumulation of histiocytes (arrow) around a capillary (asterisk) (hematoxylin and eosin stain, 20x magnification.
The histopathological examination of the cervical biopsy revealed cervicitis with epithelioid and palisading non-necrotizing granulomas composed of clusters of lymphoid cells, histiocytes, and multinucleated giant cells (Figures 2C and 2D). Immunohistochemical staining for CD68 and pancytokeratin revealed the presence of histiocytes and epithelial cells, respectively. Therefore, histologically, no malignancy was detected in the epithelium. Repeated sequential biopsies showed the same result. The Grocott, periodic acid-Schiff (PAS), and Gram staining of the biopsy tissue were negative for fungal bodies and bacteria. A bacterial culture and a polymerase chain reaction assay of the vaginal secretions were also negative for mycobacterium tuberculosis.
Considering the results of all investigations, the patient was diagnosed with idiopathic granulomatous cervicitis. She was followed regularly without any therapeutic intervention. After 6 months, a repeat MRI showed partial reduction of the mass with the contrast-enhancement extending to the vagina, both parametria, and the posterior bladder, consistent with a finding of chronic inflammatory disease.
Discussion
We herein describe a case of idiopathic granulomatous inflammation of the cervix in an 88-year-old woman with spontaneous resolution. Granulomatous inflammation is rarely observed during histological examination of tissues derived from the female genital tract. A retrospective study over a 10-year period revealed a prevalence of cervical granulomas of only 1.1% (12/1,090 cervical specimens) [3]. This form of inflammation is a non-specific finding, whereas granulomas presenting as a well-defined mass or lesion may have several potential diagnostic etiologies. The histologic pattern of the granulomatous inflammation is also a helpful predictor of diagnostic etiology. Two broad forms of well-defined granuloma, as defined by their etiology, are the foreign-body giant cell granulomas and immune granulomas. The clinicopathologic features of 22 cases of uterine cervical granulomas recorded in the published studies are summarized in Table 1 [3,5-9]. Regardless of their necrotizing or non-necrotizing histopathology, most of these recorded cases with granulomas had presented subsequent to an earlier biopsy or surgery. However, in our case, the diffuse cervical granuloma had proliferated widely throughout the tissue section and was not of a “foreign-body” type. It was therefore considered idiopathic, as the etiology could not be identified. The patient had no history of gynecological surgery or systemic granulomatous disorders, and laboratory findings suggestive of fungal or mycobacterial infections were also absent. There are older reports of rare diffuse granulomas, mostly restricted to the uterine endometrium, which indicated a localized reaction without an obvious cause [3]. In another recorded case of diffuse granulomas of the uterine cervix, the inflammatory reaction was identified in a large loop excision specimen, while remaining undetected on three consecutive cervical smears [8]. Our case with diffuse and idiopathic granulomatous inflammation presenting as an overt, visible mass in the cervix was unusual.
| Authors (year) |
Number of Cases |
Age (years) |
Symptoms |
Previous biopsy or surgery (interval time) |
Lesion location |
Pathologic findings |
Examination for infectious diseases |
Procedure |
Follow-up |
| Christie AJ, et al. (1980) |
1 |
24 |
No |
Colposcopic biopsy (3 months) |
Multiple granulomas |
Necrotizing |
Serologic chlamydia test-positive |
Conization |
N/A |
| Severe dysplasia |
| Evans CS, et al. (1984) |
3 |
1) 68 |
1) No |
1) Radiation therapy for Endometrial cancer (6 weeks) |
N/A |
Necrotizing |
Negative |
1) TAH+BSO+partial vulvectomy |
N/A |
| 2) 23 |
2) severe pelvic pain |
2) D&C (2 years) |
1) Focal residual endometrial cancer and Bowen's disease |
2) Hysterectomy |
| 3) 58 |
3) No |
Cervical biopsy (2 weeks) |
3) Conization |
| Wilson GE, et al. (1990) |
1 |
29 |
No |
Cesarean section (6 months) |
Focal granuloma |
Necrotizing |
Negative |
Hysterectomy |
N/A |
| Almoujahed MO, et al. (2002) |
12 |
22-81 |
N/A |
10 cases (83%), colposcopic biopsy conization, cerclage, and so on (median, 2.3 months) |
Focal granuloma (all cases) |
Non-necrotizing |
N/A |
1 Case with severe dysplasia, TAH |
Well (most cases), median, 19 months (1 month to 9 years) |
| Foreign body-type |
| Focal hemorrhage |
| Winters U, et al. (2005) |
1 |
22 |
No |
Cervical smears and colposcopic biopsy |
Diffuse granuloma |
Adjacent to CIN1 and CIN2 |
Negative |
Large loop excision of the transformation zone |
Well, 6 months |
| Kelly P, et al. (2006) |
4 |
22-85 |
N/A |
No (all cases) |
2 Cases, multiple granulomas; 2 Cases, a single granuloma |
Non-necrotizing |
Negative |
3 Cases. Hysterectomy: 1 Case, cervical loop biopsy |
Well, 3-45 months |
| N/A: not available; TAH: total abdominal hysterectomy; BSO: bilateral salpingo-oophorectomy; D&C: dilatation and curettage; CIN: cervical intraepithelial neoplasia |
Table 1: Published cases of uterine cervical granulomas.
This case had two important clinical considerations. First, the cervical granulomatous inflammation needed to be distinguished from a cervical carcinoma. The cervical mass was bulky and hemorrhagic. Moreover, contrast-enhanced MRI and CT revealed a good marginal enhancement of the mass with little central staining. These clinical and radiological findings resembled those of a cervical squamous cell carcinomatous tumor with central necrosis. The prognosis of a cervical carcinoma that has infiltrated the parametrium and the vagina is poor, and aggressive treatment with surgery, radiation, or chemotherapy is mandated in such patients [10]. Additionally, the possibility that malignant tumors may be associated with granulomatous inflammation should be considered. Therefore, in these cases, malignant tumors should be ruled out using histopathological examination following extensive tissue sampling.
Second, we found that idiopathic cervical granulomatous inflammation can recede without any therapeutic intervention including surgery or antibiotic administration. The treatment of a granulomatous inflammation should be based on causative factors. In many cases of those listed in Table 1, the coexistence of a chronic granuloma was unexpectedly discovered on histological examination oaf specimen obtained from a hysterectomy or a biopsy procedure performed for other diseases, e.g., cervical dysplasia. These granulomas were microscopic, almost asymptomatic, and not identified on their own as a discrete pathological feature. All previously reported patients with idiopathic cervical granulomas had undergone a hysterectomy or cervical loop biopsy, although not for the treatment of these particular lesions [9].
Although our patient persented witha bnormal vaginal bleeding, she was too old to be offered an extended resection of a cervical lesion involving extrauterine structures. We thus chose to follow an expectant management protocol. Even in the absence of any active treatment, the cervical mass was observed to partially reduce in size after 6 months. Three other cases of diffuse uterine granulomas have been monitored in a similar fashion, without undergoing hysterectomy. One of the patients was diagnosed with sarcoidosis after 16 months, while the two remaining patients experienced no symptoms during 7 and 88 months of follow-up [3]. It is unclear whether a patient with an idiopathic cervical granuloma should be treated surgically since there are only a few recorded cases [9]. Based on our experience with this patient, we suggest that an expectant management or watchful waiting without any treatment may be a viable approach for patients with idiopathic cervical granulomatous inflammation.
Conclusion
An idiopathic cervical granulomatous inflammation can be simply monitored without any therapeutic intervention after the definitive exclusion of a malignancy using histopathological examination, even if its appearance resembles that of cervical cancer.
Acknowledgement
The authors thank Dr. Yukiko Morinaga, Ms. Mikiko Ogura, and Ms. Yukiko Nakagawa, Department of Pathology, Kyoto Prefectural University of Medicine for their helpful advice regarding the pathological findings.
Author Contributions
All authors conceived of the presented idea. K. Y. and T. M. developed the theory and wrote the manuscript. J. K. supervised the findings of this work. All authors contributed to the final version of the manuscript.
Conflict of Interest
The authors declare that they have no conflicts of interest to report and nothing to disclose.
Informed Consent
Informed consent was obtained from the patient.
References
- Williams GT, Williams WJ (1983) Granulomatous inflammation - A review. J Clin Pathol 36: 723-733.
- Shah KK, Pritt BS, Alexander MP (2017) Histopathologic review of granulomatous inflammation. J Clin Tuberc Other Mycobact Dis 7: 1-12.
- Almoujahed MO, Briski LE, Prysak M, Johnson LB, Khatib R (2002) Uterine granulomas: Clinical and pathologic features. Am J Clin Pathol 117: 771-775.
- James DG (2000) A clinicopathological classification of granulomatous disorders. Postgrad Med J 76: 457-465.
- Christie AJ, Krieger HA (1980) Indolent necrotizing granulomas of the uterine cerfix, possibly related to chlamydial infection. Am J Obstet Gynecol 136: 958-960.
- Evans CS, Goldman RL, Klein HZ, Kohout ND (1984) Necrobiotic granulomas of the uterine cervix. A probable postoperative reaction. Am J Surg Pathol 8: 841-844.
- Wilson GE, Haboubi NY, McWilliam LJ, Hirsch PJ (1990) Postoperative necrotising granulomata in the cervix and ovary. J Clin Pathol 43: 1037-1038.
- Winters U, Watson AJ, Dalal NR (2005) A case of diffuse granulomas of the cervix. J Obstet Gynaecol 25: 225.
- Kelly P, McCluggage WG (2006) Idiopathic uterine granulomas: report of a series with morphological similarities to idiopathic ovarian cortical granulomas. Int J Gynecol Pathol 25: 243-246.
- Quinn MA, Benedet JL, Odicino F, Maisonneuve P, Beller U, et al. (2006) Carcinoma of the cervix uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet 95 Suppl 1: S43-103.