- (2006) Volume 7, Issue 1
Lucia Calculli1, Raffaele Pezzilli2, Riccardo Casadei3, Marta Fiscaletti1, Giampaolo Gavelli1
Departments of 1Radiology, Department of 2Internal Medicine and 3Department of Surgery, Sant’Orsola-Malpighi Hospital. Bologna, Italy
Pancreatitis; Pancreatitis, Acute Necrotizing; Pancreatitis, Alcoholic; Diagnostic Imaging; Tomography, X-Ray Computed
ARDS acute distress respiratory syndrome; CT: computed tomography; MDCT: multidetector computed tomography; THAD: transient hepatic attenuation difference
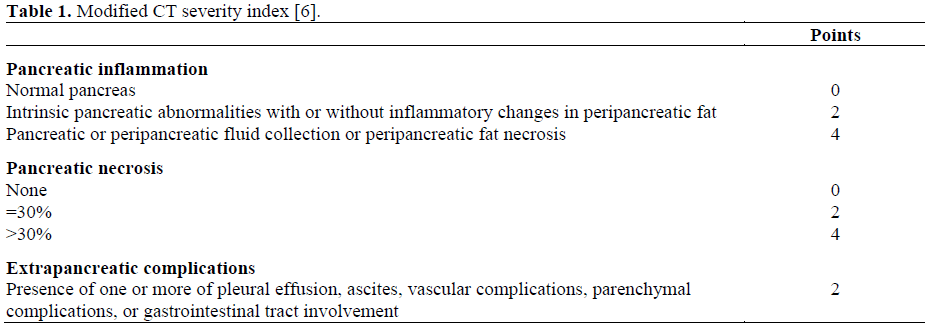
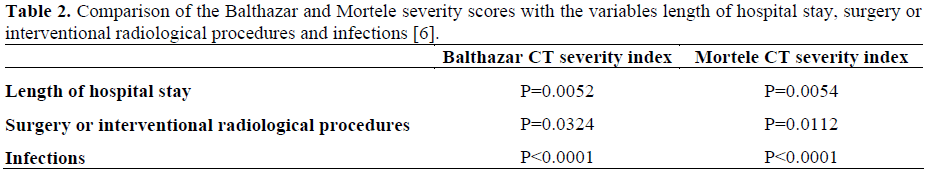
In clinical practice, it is important to establish the severity of acute pancreatitis as soon as possible. At present, the assessment of the severity of acute pancreatitis is defined according to the Atlanta clinical criteria [1]. From the clinical point of view we know that the severity of acute pancreatitis is related to the age of patients, the male sex, and the alcoholic and idiopathic etiology of the illness [2]. Furthermore, from a microbiological point of view, the infection of the necrosis reaches a peak in the third week from the onset of an acute attack of pancreatitis [3]. Imaging plays an important role in answering the clinical question: is the pancreatitis mild or severe? The best way to answer to this question is to determine the presence of pulmonary or pleuric alterations at chest Xray, associated or not with an increase in serum creatinine greater than 2 mg/dL. This simple severity assessment has already been demonstrated in clinical practice and a multicenter Italian study was published in 1999 [4]. The authors demonstrated that in 539 acute pancreatitis patients, 163 of whom (30.2%) had necrotizing pancreatitis, the presence of pulmonary or pleural alterations with or without a creatinine concentration greater than 2 mg/dL had a sensitivity of 60% and a specificity of 88% in evaluating the presence of necrosis, a sensitivity of 73% and a specificity of 75% in evaluating the presence of infected necrosis, and a sensitivity of 90% and a specificity of 76% in evaluating the mortality rate. However, computed tomography (CT) and the recently introduced multidetector CT (MDCT) had an important role in defining not only the presence of pancreatic alterations but also the presence of associated extrapancreatic involvement; in fact, the MDCT permits us to confirm the clinical diagnosis of acute pancreatitis, to establish the etiology of the illness, to weigh the necrosis, and to evaluate the follow-up of the pancreatic and extra-pancreatic complications. Even if the MDCT is a more sensitive technique than a traditional spiral CT, the timing of the appearance of necrosis using this technique was not changed; in fact, the presence of necrosis is well-visualized after 48-72 hours from the onset of acute pancreatitis. The MDCT has changed the traditional Balthazar score [5] in assessing the severity of acute pancreatitis. With this technique, which is faster than the traditional spiral CT, we can obtain more information about the involvement of peri- and extrapancreatic organ involvement; more information may be obtained regarding involvement of the portal vein, the mesenteric superior vein, the mesenteric superior artery and celiac trunk. Furthermore, we can also obtain information about pleural and pulmonary alterations. Thus, a new CT severity index has been proposed by Mortele et al. [6]. These authors have reported that the MDCT severity index (Table 1) was highly related to hospital stay, surgery or interventional radiological-related procedures and the presence of infection (Table 2).
What does MDCT add to what is already known about the imaging of acute pancreatitis? The first important point is that MDCT is able to exactly define the pancreatic involvement: the edema (Figure 1), stranding (Figure 2), fluid collections (Figure 3), necrosis of the gland (Figure 4), and peripancreatic fat (Figure 5) is easily recognized with this technique. MDCT is also able to reveal the presence of infection of the necrosis with high resolution (Figure 6), the development of pseudocysts (Figure 7), and the possible link between the pseudocysts and the pancreatic ducts (Figure 8).
However, as reported above, the advantage of this new technique is the diagnosis of extrapancreatic alterations. MDCT is highly sensitive in evaluating the presence of pleural and pulmonary lesions as pleural effusions (Figure 9), pulmonary infiltrates and acute distress respiratory syndrome (ARDS; Figure 10). Using “ad hoc” software, MDCT is also able to demonstrate the multiplanar reconstruction for the study of the vascular system and the pancreatic ducts to evaluate the presence of spleen involvement (Figure 11), the transient hepatic attenuation difference (THAD) (Figure 12), the presence of pseudoaneurisms (Figure 13) or thrombosis of the splenic vein (Figure 14).
MDCT recognizes small lesions such as the presence of small pancreatic cancers which may be associated with a mild acute pancreatitis in about 6% of the cases [7] (Figure 15).
This technique is of assistance to clinicians with interventional radiological procedures such as the sampling of the necrosis for microbiological assessment (Figure 16), and the percutaneous treatment of fluid collections and pseudocysts in high risk patients.