Keywords
Retention; Tooth supported overdentures; Thermo-elastic acrylic resin
Introduction
For patients with severely reduced or hopeless dentition planned for total extraction, overdenture may serve as excellent measure, as it is concerned with the continued preservation of alveolar bone around the retained teeth/root pieces/implants. Overdenture also preserves the periodontal sensory mechanisms that guide and monitor gnathodynamic functions, that will improve person’s gnathodynamic functions and psychology, as it preserves the proprioceptive impulses [1].
Using of tooth-supported overdenture is a common form of treatment [2]. Denture pressure on a residual ridge results in bone resorption. The technique of tooth root retention under complete dentures appears to militate against such a force application [3].
Presence of soft tissue and, bony undercuts complicate the treatment plan [4]. One such clinical condition may pose a problem in denture insertion and may even affect the denture esthetics as a bulbous labial cortical plates accompanying severe labial undercut [5]. Various prosthodontics management of the undercuts is done by blocking out undercut on the cast and finishing the denture to the full available height of the vestibule. Alternatively, the height of the denture flange can be reduced to the crest of the undercut (to the survey line when the cast has been surveyed). A reduced border seal may accompany such a denture base adaptation [6].
Through recent advancements in material science, thermoelastic dentures have emerged as a viable option to treat various edentulous conditions. It has shown several advantages over the traditional rigid denture bases. Being flexible, the denture base adapts well in the undercut areas. The amount of adjustment required at time of denture insertion is greatly reduced and this reduces post insertion complaints of denture induced trauma (ulceration) [4]. The material being soft and strong can be made thinner and are light in weight compared to conventional dentures [7].
A multipurpose thermo-elastic acrylic resin material “Versacryl” is heat-sensitive cross-linked acrylic resin that remains thermoelastic after polymerization and chemically bond to the acrylic denture base [8]. Versacryl is relatively rigid at body temperature, but tempering in hot water softens the material. Adjustments are accomplished by first chilling the denture before polishing or grinding. The result is a semi-rigid flange that slides easily over soft-tissue undercuts. This allowed the undercut to act as an active part of the retentive mechanism for the denture. It also reduced the incidence of sore spots and denture irritation [9].
It has been shown that solitary non splinted attachments are less technique sensitive, and easier to clean than bars. Thus, this study was designed to investigate that the retention of tooth supported or retained MOD is affected mainly by attachment type or by denture base material. The null hypothesis was that there will be no significant difference in the MOD retention.
Materials and Methods
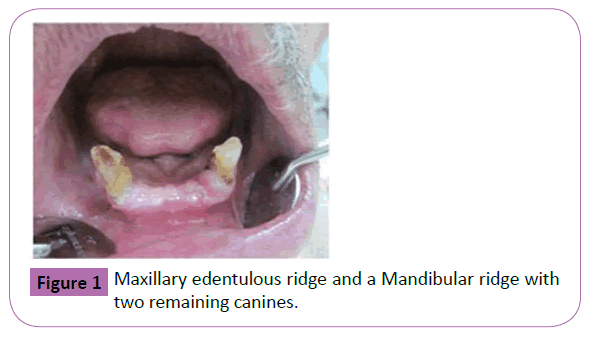
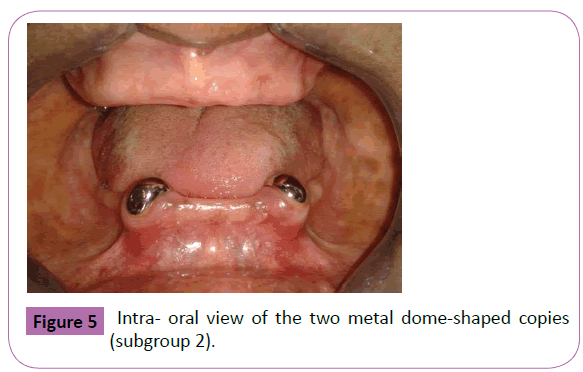
Eighteen consecutive patients of age ranging from 40 to 60 years (mean 50 years) were recruited from the clinic of the Removable Prosthodontics Department. Inclusion criteria for enrollment were; patients have good health with no systemic diseases relating to bone resorption. They had completely edentulous maxilla against partially edentulous mandible in which only two canines were remaining with healthy periodontal attachment with adequate alveolar bone support and crown/root ratio not less than 1:1 as verified by periapical radiographs. The mobility pattern of each retained two mandibular canines was less than grade II (Figure 1). Patients had sufficient interarch space for MOD construction. Each patient was given a detailed description of the procedures and agreed to being randomized. They agreed to be treated by either prosthodontic providers using their preferential treatment modality and signed an informed consent before participation in the follow-up program. The study protocol had been reviewed and approved by the institutional review board.
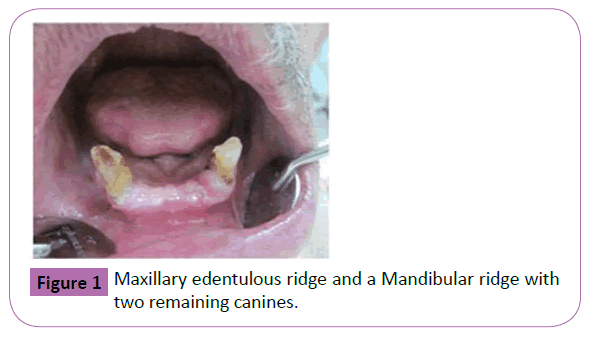
Figure 1: Maxillary edentulous ridge and a Mandibular ridge with two remaining canines.
According to the denture base material, each patient received hard acrylic denture base Group I and thermo-elastic acrylic denture base material Group II. Each group received three types of abutment preparation for each patient (Subgroup 1) received long copying preparation, (Subgroup 2) received short copying preparation and (Subgroup 3) received stud attachment.
Prosthodontic Treatment
Tooth-retained overdenture on long copying
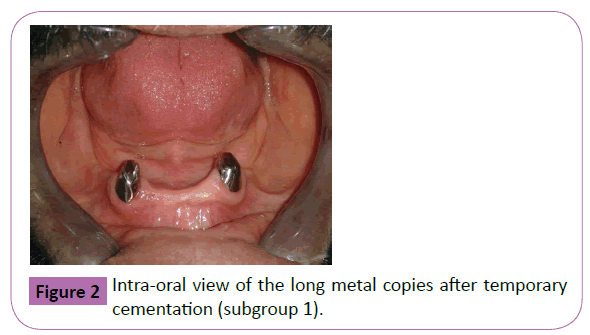
Each patient retained two canines were endodontically treated, reshaped and shortened approximately to a level 3-4 mm above gingival margin to create space for placing high copy and artificial teeth [10]. Construction of the two metal copings followed by their cementation with temporary cement material (Figure 2). A secondary impression for the maxillary arch was made and, mandibular full arch special tray (open tray) was constructed and fenestrated in the abutment areas so, it didn't touch the copings, a selective pressure impression technique was made, duplication of the mandibular master cast was done to make a secondary master cast for the thermo-elastic overdenture construction. Maxillo-mandibular jaw relation records were registered, Semi anatomic acrylic resin teeth of angle 25 were selected, arranged to achieve a balanced occlusion. Maxillary denture was processed from hard acrylic resin (vertex rapid simplified, vertex dental company, Holland).
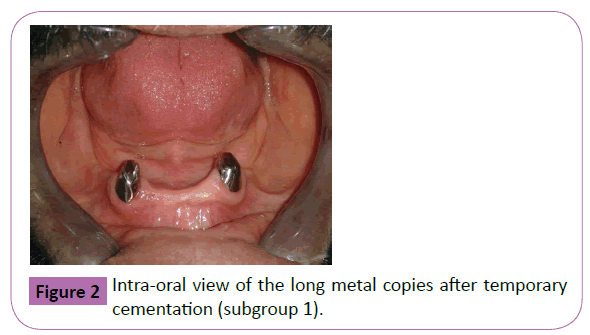
Figure 2: Intra-oral view of the long metal copies after temporary cementation (subgroup 1).
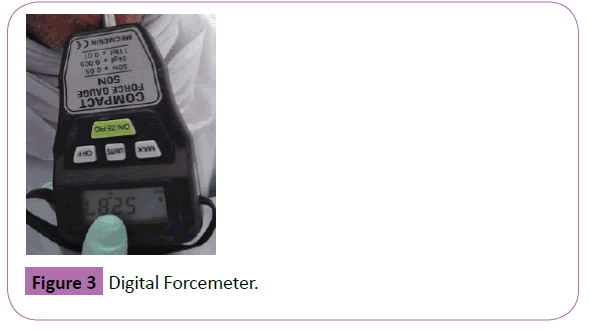
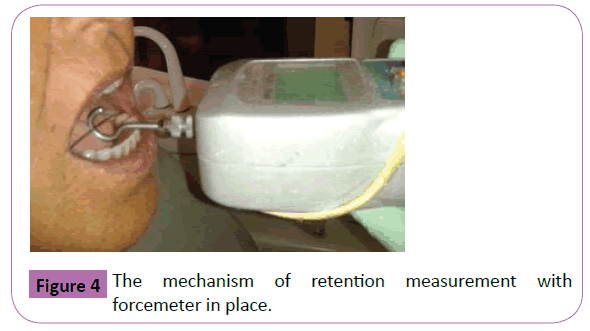
According to the material used in packing, there were two MOD hard acrylic one (Group I) (vertex rapid simplified, vertex dental company, Holland) and versacrylic one (Group II) (Versacryl, apple dental ventures, Ontario, Canada). The two MOD were checked intraorally to ensure complete passivity using a pressure indicating paste. A venting hole was drilled lingually opposite to each house, auto-polymerized acrylic resin was added in the fitting surface of the overdenture around the abutments to read apt the denture, the excess acrylic material was removed and the two dentures were inserted and checked for proper occlusion and retention. Retention of the two MOD were measured in the same patient (for the long copings) after 24 hours and after one month from its insertion date by using a digital forcemeter [11,12] device (Figure 3) (Mecmesin Corp, Virginia, USA) as following: The patient was seated in an upright position with the head resting firmly, brass wire was secured to the MOD buccal and below the first molars with cold-curing acrylic resin so the force meter device could exert a vertical dislodging force on the denture. The hook attachment was placed on the shaft of the force meter device and engaged the center of the brass wire loop, The pull end of the forcemeter was connected to an 0.9 mm orthodontic wire that attached to a distal hook, The forcemeter was pulled vertically (Figure 4) until the denture was elevated [12]. This force was measured in newton and recorded as the denture’s retention. For each patient, three records were taken each time and an average was taken.
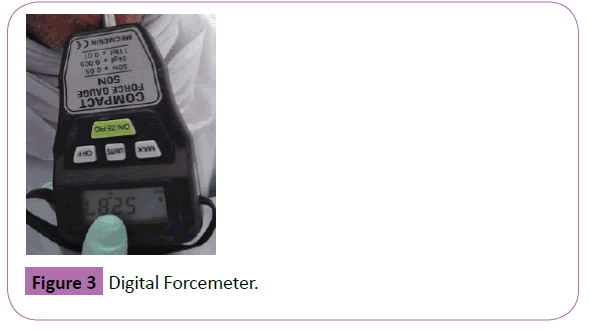
Figure 3: Digital Forcemeter.
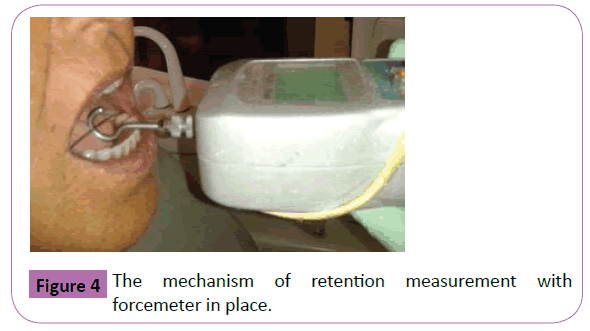
Figure 4: The mechanism of retention measurement with forcemeter in place.
Tooth supported overdenture on short copyings
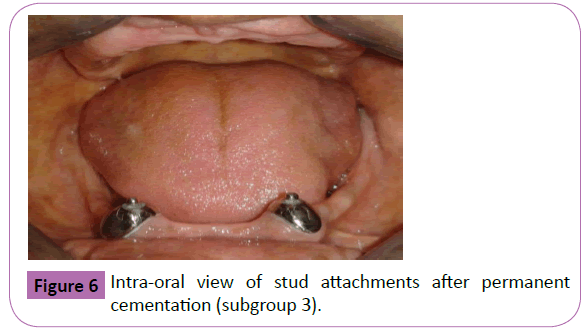
After two months the metal copings were removed and the two abutments were reshaped and shortened more to have a dome shaped preparation approximately 1-2 mm above gingival margin with chamfer finish line [13,14] (Figure 5). Two plastic dowels were selected. An elastomeric impression was made to the prepared abutments and dowels. two metal copings with dowels were tried, and temporarily cemented, two MOD were checked to eliminate any rocking then a functional readaptation with self-cure acrylic resin was made; retention of the two MOD were measured as before for each denture for 24 hours and for one month from its insertion date.
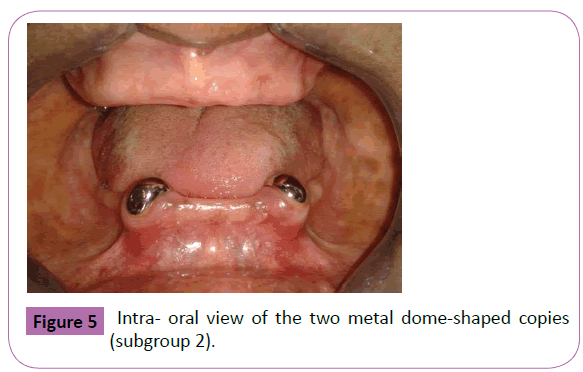
Figure 5:Intra- oral view of the two metal dome-shaped copies (subgroup 2).
Tooth retained overdenture on stud attachment
After another two months the same patient received two stud attachments, two short metal copings were removed, the preparation for the stud attachment was as the same preparation as short copings with dowels. A plastic-threaded stud of size about 3 mm was attached to each waxed dowel copings. Both studs were made parallel to each other using a dental surveyor, waxed dowel coping and the stud assembly was casted in cobalt cromium metal base (Figure 6) and tried in patient mouth, two stud attachments were tried in the patient mouth, cemented by permanent cement. As with the short copings, two MOD were relieved about 1 mm in the two housings and checked to ensure complete passivity; the retention element (matrix) is an integral part of a soft liner of an ordinary acryl denture. A self-cure silicone based soft liner was placed in the two housings as a retentive female unit instead of plastic female caps, [15] the patient was asked to close in its centric occlusion until the soft liner was set, excess material was removed from the venting holes. Retention was measured for both MOD.
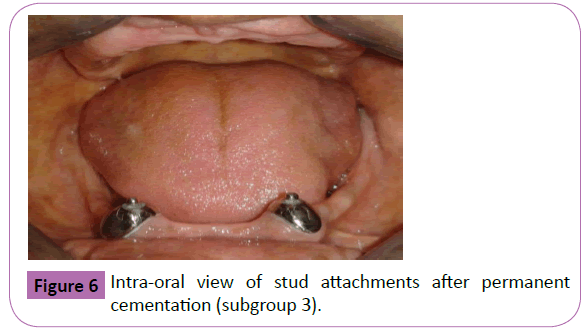
Figure 6: Intra-oral view of stud attachments after permanent cementation (subgroup 3).
Statistical Analysis
The SPSS statistical package for social science version 22 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Shapiro-Wilk test was used to test the normality of the recoded retention values. The data was parametric and normally distributed. Multivariate analysis with repeated measures (ANOVA) was applied to test possible differences in retention force between groups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments).
Subsequently, posthoc tests (least significant difference multiple comparison test) were used for pairwise comparisons of results. For differences between denture types (hard acrylic resin and flexible acrylic resin), and observation times (one day after insertion and 30 days after insertion), paired samples t-test was used. P is significant if <0.05 at confidence interval 95%.
Results
Table 1 shows comparisons of retention values between three subgroups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments) at two observation periods (24 hours after MOD insertion and one month after MOD insertion) for hard acrylic resin.
| |
24 hours after MOD insertion |
One month after MOD insertion |
| Group 1 (X ± SD) |
12.7917 ± 2.19509 |
7.6500 ± 2.86758 |
| Group 2 (X ± SD) |
5.0417 ± 2.52496 |
3.3500 ± 0.23664 |
| Group 3 (X ± SD) |
6.6083 ± 1.56090 |
6.6483 ± 2.94212 |
Repeated measure One Way
ANOVA (p value) |
0.00* |
0.006* |
| F |
37.115 |
9.042 |
| LSD |
6.18 |
3.29 |
Table 1: Comparisons of retention values between different groups at both observation periods for hard acrylic resin.
There was a significant differences between groups 24 hours after MOD insertion (One way ANOVA, p=0.00*) and one month after MOD insertion (One way ANOVA, p=0.006*). Multiple comparison between subgroups are presented in. At 24 hours after MOD insertion, there was a significant difference between subgroup 1 and subgroup 2 and between subgroup 1 and subgroup 3 but there was insignificant difference between subgroup 2 and subgroup 3. At one month after MOD insertion, there was a significant difference between subgroup 1 and subgroup 2 and between subgroup 2 and subgroup 3 but there was insignificant difference between subgroup 1 and subgroup 3 (paired samples t-test).
The greatest retention values were recorded with tooth retained MOD with long copings followed by tooth retained MOD with stud attachments and the lowest retention values were obtained with tooth supported MOD with short copings.
Comparisons of retention values between different subgroups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments) at the 2 observation periods (24 hours after MOD insertion and one month after MOD insertion) for Thermo-elastic resin are presented in Table 2. There was a significant differences between groups 24 hours after MOD insertion (One way ANOVA, p=0.00*) and one month after MOD insertion (One way ANOVA, p=0.006*).
| |
24 hours after OD insertion> |
One month after OD insertion> |
| Group 1 (X ± SD)> |
13.6917 ± 3.44651> |
16.8200 ± 9.89796> |
| Group 2 (X ± SD) > |
5.6000 ± 1.70577 > |
4.0200 ± 0.52031 > |
| Group 3 (X ± SD) > |
9.1150 ± 3.01641 > |
6.6000 ± 2.15128 > |
| Repeated measure One Way ANOVA (p value)> |
0.00*> |
0.006*> |
| F > |
20.56 > |
9.12 > |
| LSD > |
3.51 > |
2.58 > |
Group 1 Tooth retained MOD with long copings, group 2 tooth supported MOD with short copings; group 3 tooth retained MOD with stud attachments, X mean, SD standard deviation, *Significant at 5% level of significance.
Table 2: Comparisons of retention values between different groups at both observation periods for flexible acrylic resin.
Multiple comparisons between groups are presented in At 24 hours after MOD insertion, there was a significant difference between subgroup 1 and subgroup 2 and between subgroup 1 and subgroup 3 and between subgroup 2 and subgroup 3. At one month after MOD insertion, there was a significant difference between subgroup 1 and subgroup 2 and between subgroup 2 and subgroup 3 and between subgroup 1 and subgroup 3 (paired samples t-test). The greatest retention values were recorded with tooth retained MOD with long copings followed by tooth retained MOD with stud attachments and the lowest retention values were obtained with tooth supported MOD with short copings.
Comparisons of retention values between the 2 denture types (hard acrylic resin MOD and Thermo-elastic resin MOD) for different subgroups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments) at 24 hours after MOD insertion used are presented in Table 3. The retention values of Thermoelastic resin MOD was greater than hard acrylic resin MOD for all subgroups 24 hours after MOD insertion but the difference was not significant (paired samples t-test, p>0.05).
| |
Group I (Tooth retained MOD with long copings) |
Group II (Tooth supported MOD with short copings) |
Group III (Tooth retained MOD with stud attachment) |
| Hard acrylic resin OD X ± SD |
12.7917 ± 2.19509 |
5.0417 ± 2.52496 |
6.6083 ± 1.56090 |
| Thermo-elastic acrylic resin OD X ± SD |
13.6917 ± 3.44651 |
5.6000 ± 1.70577 |
9.1150 ± 3.01641 |
| Paired samples t- test (p-value) |
0.426 |
0.661 |
0.069 |
X: Mean, SD: Standard deviation, *Significant at 5% level of significance
Table 3: Comparisons of retention values between the 2 denture types (hard acrylic resin MOD and Thermo-elastic resin MOD) 24 hours after MOD insertion.
Comparisons of retention values between the 2 denture types (hard acrylic resin MOD and Thermo-elastic resin MOD) for different subgroups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments) at one month after MOD insertion used are presented in Table 4. The retention values of Thermo-elastic acrylic resin MOD was significantly greater than hard acrylic resin MOD for all groups I and group II one month after MOD insertion (paired samples t-test, p=0.047 for group 1 and 0.016 for group 2 respectively).
| |
Group I(Tooth retained MOD with long copings) |
Group II(Tooth supported MOD with short copings) |
Group III(Tooth retained MOD with stud attachment) |
| Hard acrylic resin MOD X ± SD |
7.6500 ± 2.86758 |
3.3500 ± 0.23664 |
6.6483 ± 2.94212 |
Thermo-elastic acrylic resin MOD
X ± SD |
16.8200 ± 9.89796 |
4.0200 ± 0.52031 |
6.6000 ± 2.15128 |
| Paired samples t-test (p-value) |
0.047* |
0.016* |
0.961 |
X: Mean, SD: Standard deviation, *Significant at 5% level of significance
Table 4: Comparisons of retention values between the 2 denture types (hard acrylic resin MOD and Thermo-elastic resin MOD) 30 day after OD insertion.
Comparisons of retention values between the 2 observation periods (24 hours after MOD insertion and one month after MOD insertion) for different subgroups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments) when hard acrylic resin MOD was used are presented in Table 5. The retention values after 24 hours after MOD insertion was greater than values after one month of MOD insertion for hard acrylic resin MOD, but the difference was significant only for subgroup 1 (paired samples t-test, p=0.001).
| |
Group I (Tooth retained MOD with long copings) |
Group II (Tooth supported MOD with short copings) |
Group III (Tooth retained MOD with stud attachment) |
| 24 hours after MOD insertion X ± SD |
12.7917 ± 2.19509 |
5.0417 ± 2.52496 |
6.6083 ± 1.56090 |
| One month after MOD insertion X ± SD |
7.6500 ± 2.86758 |
3.3500 ± 0.23664 |
6.6483 ± 2.94212 |
| Paired samples t-test (p-value) |
0.001* |
0.151 |
0.976 |
X: Mean, SD: Standard deviation, *Significant at 5% level of significance
Table 5: Comparisons of retention values between the 2 observation times (24 hours and One month after MOD insertion) for hard acrylic resin MOD.
Comparisons of retention values between the 2 observation periods (24 hours after MOD insertion and one month after MOD insertion) for different subgroups (tooth retained MOD with long copings, tooth supported MOD with short copings and tooth retained MOD with stud attachments) when Thermoelastic acrylic resin MOD was used are presented in Table 6. The retention values after 24 hours after MOD insertion was greater than values after one month of MOD insertion for hard acrylic resin MOD, but the difference was significant only for subgroup 3 (paired samples t-test, p=0.002).
| |
Group I (Tooth retained MOD with long copings) |
Group II (Tooth supported MOD with short copings) |
Group III (Tooth retained MOD with stud attachment) |
| 24 hours after MOD insertion X ± SD |
13.6917 ± 3.44651 |
5.6000 ± 1.70577 |
9.1150 ± 3.01641 |
| One month after MOD insertion X ± SD |
16.8200 ± 9.89796 |
4.0200 ± 0.52031 |
6.6000 ± 2.15128 |
| Paired samples t-test (p-value) |
0.323 |
0.058 |
0.002* |
X: Mean, SD: Standard deviation, *Significant at 5% level of significance
Table 6: Comparisons of retention values between the 2 observation times (24 hours and One month after MOD insertion) for Thermo-elastic acrylic resin MOD.
Discussion
Overdentures which are supported by the roots of natural teeth have more predictable outcomes because of increased support, stability and retention and decrease in rate of ridge resorption. Overdenture offer both bio-functional and psychological advantages to the patient. The bio-functional advantages include preservation of the residual ridge when the roots are present, maintenance of the proprioceptors for finer coordination of mandibular movement, better support, sparing of the residual ridges from occlusal over loading, minimizing horizontal forces on abutment teeth, and increased masticatory efficiency. Also psychological advantage of overdentures is not rendering the patient completely edentulous.
All patients in this study are free of any bone resorptive diseases as in case of uncontrolled diabetes the oral mucosa also loses resilience, which is necessary for good adaptation of a complete denture. Moreover, patients with bone resorptive disease present a lower level of retention of complete dentures than patients without the disease, since diabetes increases the osteoblastic activity of bone tissue in the mandible and maxilla [16].
All patients which are selected have two remaining mandibular canines, as retaining of mandibular canines has the main concern for alveolar bone preservation particularly in mandibular anterior segment [17]. The canines are stated to be the most richly innervated and sensitive amongst all teeth and thus become the preferred abutment teeth under overdentures. Also due to their long triangular roots they are retained in the system for longer duration [1].
In this study, for hard and thermo-elastic acrylic resin, there was a significant difference between subgroups, 24 hours and one month after MOD insertion. The greatest retention values were recorded with tooth retained MOD with long copings followed by tooth retained MOD with stud attachments and the lowest retention values were obtained with tooth supported MOD with short copings. This may be due to the tapered configuration of the contacting walls generates a compressive inter surface tension. The tension should be sufficiently strong enough to sustain the prosthesis in its place. Furthermore projections above the root surface predictable prosthodontic outcomes because of increased support, stability and retention and decrease in rate of the residual ridge resorption [18]. This is in agreement with Goswami et al. [19] who discussed that telescopic or double crowns have proven to be an effective means of retaining overdenture.
Additionally, the retentive concept in the form of stud and long copy preparation show higher retentive values than supportive concept in the form of short dome shaped preparation. This is in agreement with a study of Jayarsee et al. [20] who explained that retention and stability of overdentures can be improved by attachments. Supportive concept using dome shaped copings usually less retentive as there is less vertical component of root projecting from the gingival so less stability and retention.
The stability and retention are enhanced by the vertical component of the retained tooth in the alveolar one [21]. But in this study long copings showed higher retention than studs of about (2.4 mm) in diameter opposed by soft liner as a flexible retention system and this is concurred with a study by Koike et al. [22] who stated that the retentive values of the soft liner with ball diameter (1.7 and 2.2 mm) was lower than those obtained by rubber o- ring attachment with the same ball diameter. Concluding that although the retention force of the soft lining material is low owing to the material's low hardness, but a high retention force can be achieved by increasing the diameter of the male rather than increasing the height of the ball.
The results of the present study elucidate that the retention values of Thermo-elastic acrylic resin MOD was greater than hard acrylic resin MOD for all groups, 24 hours and one month after MOD insertion but the difference was significant only for tooth retained MOD with long copings and tooth supported MOD with short copings after one month of MOD insertion This could be attributed to the shape memory of the Thermo-elastic acrylic resins which are polymeric smart materials which possess the ability to store and recover large strains by the application of a prescribed the rmome-chanical cycle in response to an external stimulus, such as temperature [23]. This is in accordance with Tokue et al. [24] that illustrate an important advantage of the thermo-elastic resins that it has an internal memory to return to its original position. Bidkar et al. [25] concluded that the retentive values of Thermo-elastic acrylic was greater than hard acrylic resin as the thermoplastic acrylic resins have higher elasticity and higher molding precision than heat-polymerizing base resins, so, facilitate denture retention by utilizing the undercuts of abutment teeth in the denture base design increasing the retention. Whereas, hard acrylic resins are difficult to address such as insertion in undercut areas, brittleness of methyl methacrylate which leads to fracture [26].
Finally, the time factor has an effect on the retentive values, the retention values at 24 hours after MOD insertion was greater than values after one month of MOD insertion for hard and thermoelastic acrylic resin MOD, but the difference was significant only for tooth retained MOD with long copings with hard acrylic resin and for tooth retained MOD with stud attachments with thermoelastic acrylic resin. This possibly due to the warp age in the heat cure acrylic resin decreasing its fit on the supporting tissue as poly methyl methacrylate absorb water slowly over period of time. This imbibition is due primarily to the polar properties of the resin molecules. Usually a serious warpage and dimensional change in the material are associated with a high percentage of water sorption [27].
For the thermo-elastic denture base material, flexibility is not an advantage in conventional complete dentures as the retentive peripheral seal can be broken in function which may affect the retention [28]. But with the presence of an abutment or attachment with the corresponding undercut, the retentive values were not so decreased. Moreover, by time soft lining materials exposed to the continual influence of a humid environment can lose their soluble components and absorb water. The changes induced by the sorption, solubility, dehydration and oxidization of materials in a humid environment can result in the deterioration of mechanical and functional properties such as hardness which lead to decrease in the retention force [15]. This in agreement with Qudah et al. [29] who confirmed that soft lining become hardener with time and this may be due to leaching of the plasticizers. By thermo cycling provisional chair side soft lining material demonstrates a rapid deterioration at temperature greater than fifty degree.
Conclusion
Within limitations of this study, the following was concluded
The thermo-elastic acrylic resin was more retentive than hard acrylic one -Long copings preparation produced high retentive force following by stud attachments then short copings. Thermoelastic resins (versacryl) have the ability to engage undercut areas while retaining its shape. Short copings preparation with thermoelastic mandibular overdenture showed more retentive values than with hard acrylic mandibular overdenture. The retention forces decreased by time from the first 24 hours and after one month in both thermo-elastic and hard acrylic mandibular overdenture with the preference to the Thermo-elastic one.
Conflict of Interest
The authors claim to have no financial interest, either directly or indirectly, in the products or information listed in the article.
References
- Shah D, Vaishnav K, Matani H, Patel P (2013) Overdenture: conventional to contemporary: a review. J Res Adv Den 2: 24-30.
- Shinde GB, Wadkar AP (2012) Overdenture: A Way of Preventive Prosthodontics. Indian J Dent Adv 4: 863-867.
- Shankar YR, Srinivas K, Surapaneni H, Reddy SVS (2013) Prosthodontic Treatment Using Vital and Non Vital Submerged Roots-Two Case Reports. J Clin Diagn Res 7: 2396-2399.
- Shamnur SN, Jagadeesh KN, Kalavathi SD, Kashinath KR (2010) Flexible dentures-an alternate for rigid dentures. J Dent Sciences and Research 1:74-79.
- Chaturvedi S, Shah M, Ghodpage SL, Kulkarni M, Gill S (2013) Unconventional prong dentures - a case report. Int J Dent Clinics 5: 49-50.
- Ramasamy CH, Abraham (2011) A Prosthodontic Management of Undercut Tuberosities: A Clinical Report. JCDR 5: 1692-1694.
- Dhiman CR, Chowdhury LR (2009) Midline Fractures in Single Maxillary Complete Acrylic vs Flexible Dentures. MJAFI 65: 141-145.
- Zaki DYI, Moussa ARA, Abouzeid AW (2012) Dynamic Mechanical Thermal Analysis of a Multipurpose Thermo-Elastic Acrylic Resin with Different Softener/Hardener Monomer Ratios. Aust J Basic and Appl Sci 6: 695-699.
- Abrams S, Hellen W(2006) Fabrication of an overdenture covering a torus palatinus using a combination of denture base materials: a case report. Dent Today 25: 76-77.
- Dhir R (2005) Clinical assessment of the overdenture therapy. J Indian Prosthodont Soc 5:187-192.
- Schmitz JF(1966) Measurement of the efficiency of the platinum-cobalt magnetic implant. J Prosthet Dent 16:1151-1158.
- Burns DR, Unger JW, Coffey JP, Waldrop TC, Elswick RK Jr(2011) Randomized, prospective, clinical evaluation of prosthodontics modalities for mandibular implant overdenture treatment. J Prosthet Dent 106:12-22.
- Lord JL, Teel S(1969) The overdenture. Dent Clin North Am 13:871-881.
- Shetty O, Tolani P, Rathod (2013) A Oral rehabilitation using customized intra-radicular Dalbo attachments. J Interdiscip Dentistry 3:36-42.
- Chladek W, Chladek G, Wrzus-Wielinski M, Zmudzki J(2010) Examinations on retention of overdentures with elastic frictional attachments JAMME 43:205-213.
- Cristina de Lima D, Nakata GC, Balducci I, Almeida JD(2008) Oral manifestations of diabetes mellitus in complete denture wearers. J Prosthet Dent 99:60-65.
- Shah FK, Gebreel A, Elshokouki AH, Habib AA, Porwal A(2012) Comparison of immediate completedenture, tooth and implant-supported overdenture on vertical dimension and muscle activity. J Adv Prosthodont 4:61-71.
- Singh K, Gupta N(2012) Telescopic denture- A treatment modality for minimizing the conventional removable complete denture problems: A Case Report. JCDR 6: 1112-1116.
- Goswami R, Mahajan P, Siwach A, Gupta A(2013) Telescopic overdenture: Perio-prostho concern for advanced periodontitis. Contemp Clin Dent 4:402-405.
- Jayasree K, Bharathi M, Nag VD, Vinod B (2012) Precision Attachment: Retained Overdenture. J Indian Prosthodont Soc 12:59-62.
- Lord JL, Teel S (1974) The overdenture: patient selection, use of copings, and follow-up evaluation. J Prosthet Dent 32:41-51.
- Koike T, Ueda T, Noda S, Ogami K, Patil PG, et al.(2013) Development of new attachment system with soft lining material for implant-retained complete denture.Int J Prosthodont Restor Dent 3:21-24.
- Zhang CH, Wei H, Liu Y, Tan H, Guo Z (2012) Enhanced toughness and shape memory behaviors of toughed epoxy resin. High Perform Polym 24: 702-709.
- Tokue A, Hayakawa T, Ohkubo C(2013) Fatigue resistance and retentive force of cast clasps treated by shot peening. J Prosthodont Res 57:186-194.
- Bidkar DS, Hazari P, Bhoyar A, Agarwal S (2011) Flexible Overdenture: A Clinical Case Report IJCD 2(4):88-91.
- Singh JP, Dhiman RK, Bedi RP, Girish SH(2011) Flexible denture base material: A viable alternative to conventional acrylic denture base material. Contemp Clin Dent 2:313-317.
- Al-NoriAKh, Ali AA, Rejab LT(2007) Water sorption of heat–cured acrylic resin. Al-Rafidain Dent J 7: 186-194.
- Tandon R, Gupta S, Agarwal SK(2010) Denture base materials: From past to future. Indian J dent Sci 2:33-39.
- Qudah S, Huggett R, Harrison A(1991) The effect of the thermocyclingon the hardness of the soft lining materials. Quintessence Int 22:575-580.