- (2005) Volume 6, Issue 3
Muhammad Wasif Saif1, Helena Sviglin1, Mark Carpenter2
1University of Alabama at Birmingham (UAB), Birmingham. AL, USA
2Department of
Mathematics and Statistics Auburn University. Auburn, AL, USA
Received November 30th, 2004 - Accepted April 28th, 2005
Context Ethnicity is an important factor known to impact the biology and outcome of many cancers. In pancreatic cancer, African Americans are thought to have a higher incidence and poorer prognosis than Whites. Patients A total 645 pancreatic cancer patients were identified in the database, of which, 530 patients were eligible for this study and retained for the statistical analysis. Of the 530 patients, 137 (25.8%) were Blacks, 393 (74.2%) were Whites, 275 (51.9%) were males and 255 (48.1) were females. Ages ranged from 21 to 93 years with values of 62.3±13.3 years, 64.2±11.6 years, 63.1±10.9 and 64.3±13.3 (mean±SD) for Blacks, Whites, males, and females, respectively. Overall, 132 patients out of 415 (31.8%) were seen in stage I, 61 (14.7%) in stage II, 105 (25.3%) in stage III, 117 (28.2%) in stage IV, while 115 patients (21.7%) had missing stage. Results There were no significant differences between Blacks and Whites with respect to distributions across stages (P=0.422). Adenocarcinoma was the most common histology in both ethnicities with poor differentiation in 47.4% of Blacks and 57.0% of Whites. Overall, 125 (23.6%) received surgery alone, 54 (10.2%) surgery with chemotherapy, 5 (0.9%) surgery with external radiation therapy, 10 (1.9%) external radiation therapy alone, 68 (12.8%) chemotherapy alone, 58 (10.9%) chemo-external radiation therapy, and 210 (39.6%) no therapy. Overall, only 22 patients survived at 5-yr (4.2%). Median survival was 8.0 months for Blacks (95% CI: 6.4-10.2) and 8.1 months for Whites (95% CI: 7.1-9.7) and there was no significant difference in survival between Blacks and Whites (P=0.971). There were more survivors in females (43/255, 16.9%) than in males (25/275, 9.1%; P=0.009), and females had significantly greater survival times as compared to males (P=0.022). Conclusions Pancreatic cancer is a disease of both ethnicities with a slight male predominance among Whites and female predominance among Blacks. We did not find any significant difference in the treatment specific outcome and survival between Blacks and Whites.
African Americans; Ethnic Groups; European Continental Ancestry Group; Pancreatic Neoplasms
AJCC: American Joint Committee on Cancer; B: Black; CALGB: Cancer and Leukemia Group B; F: female; FAMMM: familial atypical multiple-mole melanoma; M: male; SEER: Surveillance, Epidemiology, and End Results; UAB: University of Alabama at Birmingham; W: White (Caucasian); XRT: external radiation therapy
Over the last few decades, the study of pancreatic cancer has assumed a position of growing importance because of its increasing incidence and poor prognosis. Approximately 170,000 new cases of pancreatic cancer, or around 2.1% of all cancers, occur worldwide every year [1]. Cancer of the pancreas is the fifth most common cause of cancer deaths among both males (M) and females (F) worldwide [2, 3] and the fourth most common cancer in the United States, accounting for nearly 30,000 cases. In the United States, this incidence rate reflects a slight decline, observed principally among White (W) males, in which the incidence has fallen from 12.8 cases per 100,000 in 1973 to 9.6 cases per 100,000 in 1997 [3]. The incidence to death ratio is virtually equal and reflects the almost universally fatal outcome for this disease. Therefore, despite the decline in incidence, pancreatic cancer remains the fourth leading cause of death in the USA. There is also evidence that the incidence rate is 50% to 90% higher among Blacks (B) than among W in the United States [4]. In 1995-1999, the average annual age-adjusted incidence rates were 16.6/100,000 for B and 10.7/100,000 for W [4]. Reasons for this 55% excess risk among B are unclear. Pancreatic cancer incidence rates among B living in Africa appear to be low in comparison to those among African Americans [5], suggesting that lifestyle or other environmental factors contribute to the racial disparity in risk in the United States. In addition to several other factors, the black race has also been considered to be predictive of pancreatic cancer mortality. We retrospectively analyzed the data on 645 patients with pancreatic cancer seen at the University of Alabama at Birmingham (1991-2001) to determine impact of race on outcome. The purpose of this study was to evaluate the impact of this ethnic disparity on treatment outcome and disease outcome in terms of survival.
Retrospective review of all patients diagnosed and/or treated for the exocrine pancreatic cancer (International Classification of Diseases for Oncology code equal to 157) first diagnosed from January 1991 to December 2001 at UAB was conducted. Patients presenting with only a clinical impression of cancer, but who came neither for laparotomy or autopsy, were not taken into account. If a patient lacked tissue confirmation, an in-depth medical chart review was conducted to determine the accuracy of diagnosis. A total of 645 patients were identified with a final diagnosis of pancreatic cancer, whether by surgical biopsy or by autopsy. Patients with other periampullary lesions, such as cancer of the ampulla of Vater or cancer of the biliary ducts, were excluded. Patients whose missing parameters could not be found were excluded from the analysis. A total of 530 patients (82.2% of the 645 admitted patients) met the above criteria. Patients who did not die at UAB hospitals were followed-up through contact with tumor registry, their private surgeons, and their relatives. Extent of disease and tumor grade was based on the best available data using a modification of the American Joint Committee on Cancer (AJCC) TNM classification system. Treatment specific outcomes were analyzed and statistical analysis done.
The data collected was race and we have no variable to reflect ethnicity. One might argue that they are the same and, in this case they may be, but we cannot assume that and we have no way to test it. Therefore, we have 'Black' as a race not 'African American' (see keywords) which is an ethnicity. We analyzed data as they was presented to us.
The study was approved by the institutional review committee and conformed to the ethical guidelines of the 1975 Declaration of Helsinki and further revisions. No informed consent was required as it was a retrospective design of study. The use of the term 'race' and 'Black' is contextual and reflects the norms of the times the data were collected, not the judgment or values of the authors or the institutions they are affiliated with.
Descriptive statistics (mean, median, 95% confidence intervals, absolute frequencies and relative frequencies) were computed and summarized. The endpoint for survival analysis was death from any cause. Survival curves were estimated using the Kaplan- Meier method and were compared using the log-rank test. Differences in categorical variables were analyzed using the Mantel- Haenszel liner-by-linear association and the Fisher’s exact tests, while the Student t-test was applied to continuous variables. All statistical summaries and analyses were performed using SAS software (SAS Institute, Cary, NC, USA). P-values that were less than 0.05 were considered significant (i.e., the level of significance used was alpha equal to 0.05).
General Demographics
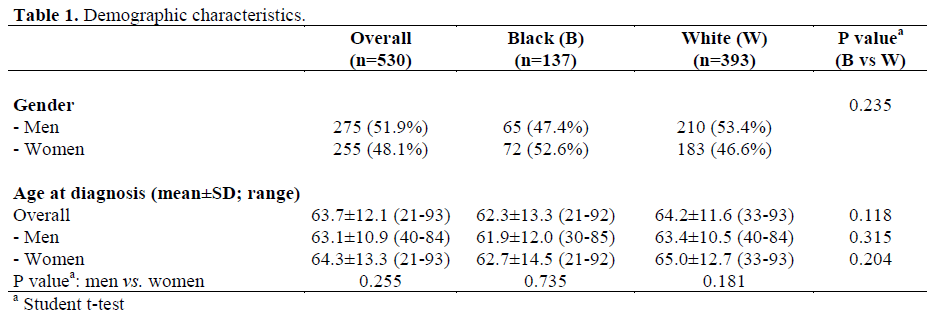
The demographic features of the 530 patients eligible for the study are listed in Table 1. Among them, 137 patients (25.8%) were B (M:F=1:1.11) and 393 (74.2%) were W (M:F=1.15:1). No significant difference for gender was observed (P=0.235). The age distribution according to gender is reported in Figure 1. As shown in Table 1, ages ranged from 21 to 93 years with mean ages of 62.3±13.3 years, 64.2±11.6 years, 63.1±10.9 and 64.3±13.3 (mean±SD) for B, W, M, and F, respectively. There were no significant differences in mean ages between B and W (P=0.118) and between M and F (P=0.255).
Year of Diagnosis
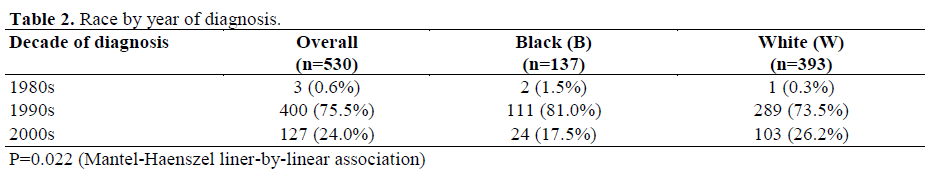
The yearly distribution according to race is depicted in Figure 2 while Table 2 summarizes the data stratified according to decades. W had a significantly higher frequency of diagnoses in the late years (P=0.022).
Histology and Anatomy
Adenocarcinoma was the most common histology in both ethnicities (n=476, 89.8% ductal adenocarcinoma) with poor differentiation in 224 (57.0%) of W and 65 (47.4%) of B (P=0.059). Cystadenocarcinoma was the most common non-adenocarcinoma (8/54, 14.8%) with predominance in young B females (n=5). Among W, more than 80% of the tumors were located in the head of the pancreas (299/373; 80.2%), followed by tail (n=39; 10.5%), and body (n=35; 9.4%), while the location was not specified in 20 (5.1%) patients. Among B, about 80% of the tumors were also located in the head of the pancreas (99/126; 78.6%), followed by the body (n=15; 11.9%), and tail (n=12; 9.5%), while it was not specified in 11 (8.0%) (location: B vs. W, P=0.702).
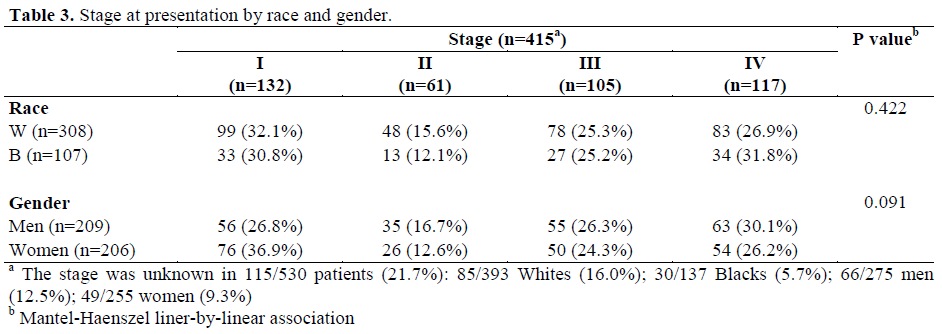
Overall, 132 (24.9%) patients were seen in Stage I, 61 (11.5%) in Stage II, 105 (19.8%) in Stage III, 117 (22.1%) in Stage IV, and 115 (21.7%) were of unknown stage (Table 3). The stage was not significantly related to race (P=0.422) and sex (P=0.091).
Therapy
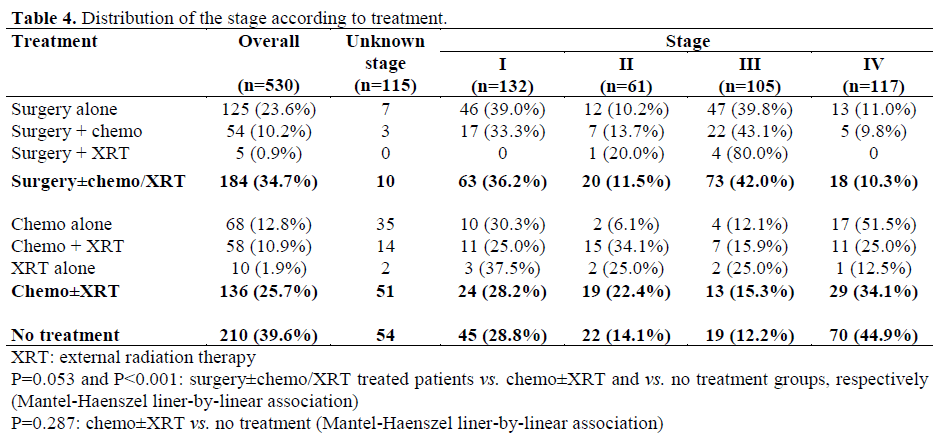
Overall, 125 (23.6%) received surgery alone, 54 (10.2%) surgery with chemotherapy, 5 (0.9%) surgery with external radiation therapy (XRT), 10 (1.9%) XRT alone, 68 (12.8%) chemotherapy alone, 58 (10.9%) chemo-XRT, and 210 (39.6%) no therapy (Table 4). Of those that received no treatment, 54 (25.7%) had no stage declared, while of the 156 known stages, 45 (28.8%) presented in stage I, 22 (14.4%) presented in stage II, 19 (12.2%) in stage III, and 70 (44.9%) in stage IV. Of the 184 patients that received surgery alone or in combination with chemotherapy or XRT, 10 (5.4%) had no stage declared while of the other 174 patients, 63 (36.2%) were in stage I, 20 (11.5%) in stage II, 73 (42.0%) in stage III, and 18 (10.3%) in stage IV. Of the 136 that received XRT or chemotherapy alone or in combination, 51 (37.5%) had no stage declared while of the other 85 patients, 24 (28.2%) in stage I, 19 (22.4%) in stage II, 13 (15.3%) in stage III, and 29 (34.1%) in stage IV. The patients that underwent surgery ± chemo/XRT presented a higher stage (P=0.053 vs. chemo±XRT; P<0.001 vs. no treatment).
The data also revealed that surgery was performed more frequently in W (102/393) than in B (23/137) (26.0% vs. 16.8%; OR= 1.74, 95% CI: 1.05-2.87; P=0.035).
Survival
Of the total 530 patients, 462 (87.2%) died with a median survival of 6.8 months (95% CI: 6.2-7.6), while the median follow-up for the 68 (12.8%) survivors was 30.9 months (95% CI: 27.5-46.2). The overall median survival was 8.1 months.
Among B, 120 (87.6%) patients died with median survival 6.6 months (95% CI: 5.0-8.2) and 17 (12.4%) survived with median followup of 46.2 months (95% CI: 30.9-57.7). Among W, 342 (87.0%) patients died with a median survival of 6.9 months (95% CI: 6.2- 7.7) and 51 (13.0%) patients survived with a median follow-up of 28.5 months (95% CI: 22.9-43.3). Overall median survival was 8.0 months for B (95% CI: 6.4-10.2) and 8.1 months for W (95% CI: 7.1-9.7) and there was no significant difference in survival between B and W (P=0.971).
For M, 250 (90.9%) patients died with a median survival of 6.9 months (95% CI: 6.2- 7.9), while 25 (9.1%) patients survived with a median follow-up of 40.5 months (95% CI: 23.1-48.9). For F, 212 (83.1%) patients died with median survival of 6.7 months (95% CI: 5.7-8.0) and 43 (16.9%) patients survived with a median follow-up of 29.4 months (95% CI: 24.1-48.4). There were more survivors in females than in males (F: 43/255, 16.9%; M 25/275, 9.1%; P=0.009) and the increased survival for females over males was statistically significant (P=0.022). Within patients who underwent surgery alone, B patients had median survival of 13.8 months (95% CI: 6.3-20.1; n=23) compared to 16.4 months in W (95% CI: 11.4-22.0; n=102) (P=0.711). The two B patients who received surgery and XRT had median survival of 17.4 months compared to 21.0 months of the three W patients. In chemotherapy-treated patients, W had slightly worse survival of 6.8 months (95% CI: 5.0- 10.0; n=53) but not significantly different (P=0.390) when compared to the B survival of 7.4 months (95% CI: 5.5-10.0; n=15,). B patients with chemo-XRT (n=17) had median survival of 11.0 months compared to 10.0 months of W (n=41) (P=0.910). Overall, we have found 190 (35.8%) 1-year survivors, 90 (17.0%) 2-year survivors and only 22 (4.2%) 5-year survivors among our population. The survival rate was not significantly different between B and W patients (P=0.971; Figure 3) while there was an increased survival for females over males (P=0.022; Figure 4).
We did not find any significant differences in the mean ages between B and W, as well as between M and F, and no significant differences between B and W with respect to distributions across stages. Also, no interesting differences were observed in treatment specific outcomes between the two ethnicities. B patients seem to benefit at par compared to W patients. Our data are similar to the Surveillance, Epidemiology, and End Results (SEER) data published in section XXI-4 [2] with respect to stage distribution, and 5-year relative survival rates.
For several decades, the incidence of pancreatic cancer has been 50% to 90% higher among B than among Whites (W) in the United States [1, 4]. The purpose of this study was to evaluate the impact of this racial disparity on treatment outcome and disease outcome. The common risk factors for pancreatic cancer include cigarette smoking (30%) [6], long-term diabetes mellitus (10%) [7], family history of pancreatic cancer (5- 10%) [8], inherited disorders (3%) [9, 10, 11, 12], and history of pancreatitis (5%) [13]. In a population-based case-control study of pancreatic cancer diagnosed in Atlanta (GA), Detroit (MI), and 10 New Jersey counties (526 cases and 2,153 population controls) [14], the investigators found that the determinants of the higher incidence of pancreatic cancer among B than among W differed by sex. Among M, established risk factors (cigarette smoking, long-term diabetes mellitus, family history of pancreatic cancer) account for 46% of the disease in B and 37% in W, potentially explaining all but 6% of the excess risk among B. Among F, however, other factors appear to contribute to the racial disparity, notably moderate/heavy alcohol consumption (more than 7 drinks per week) and elevated body mass index (above the first quartile). When these less accepted risk factors were combined with the established risk factors, 88% of the disease in B F and 47% in W F were explained, potentially accounting for all of the excess risk among B in F study population. This study suggested that, among M, the established risk factors (mainly cigarette smoking and diabetes mellitus) explain almost the entire B/W disparity in incidence. Among F, however, other factors appear to contribute to the racial disparity, notably moderate/heavy alcohol consumption and elevated body mass index. In the absence of these factors, pancreatic cancer incidence rates among B probably would not exceed those among W of either sex.
Increased incidence of pancreatic cancer in B may be attributable to genetic disparity [15, 16, 17]. Increased incidence of pancreatic cancer is seen in some breast cancer families with BRCA1 and BRCA2 mutations [18]. The cumulative risk of pancreas cancer to age 75 years among BRCA2 gene carriers has been reported to be around 7% (95% CI: 1.9-19%), compared to 85% in carriers of BRCA1 and BRCA2 mutations for breast cancer. Pancreatic cancer is probably the second most common cancer in familial atypical multiplemole melanoma (FAMMM) syndrome, an autosomal, dominantly-inherited disorder with reduced penetrance for the disease [10]. The association between the FAMMM phenotype inclusive of malignant melanoma and pancreatic cancer appears to be particularly significant in patients and families with CDKN2A (P16) mutation [9]. However, the role of genetics in this ethnic disparity is not known. Pernick et al. analyzed clinicopathologic characteristics of tumors in 410 patients (166 B and 244 W) with pancreatic cancer [19]. B had significantly higher rates of K-ras mutations to valine than did W (58% vs. 22%, respectively; P=0.015). They also found less frequent Fas expression (4% vs. 24%, respectively; P=0.048) and a trend toward more frequent strong HER2 expression (39% vs. 18%, respectively P=0.11) in B than in W.
Papillary epithelial neoplasm of the pancreas occur more commonly in young patients with a predilection for young black females. They have a good prognosis allowing conservative surgery, that may lead to a better outcome in such patients. The histological study of the specimens strongly suggests an endocrine tumor but all histological and immunocytochemical endocrine stains are negative. The ultrastructural study of these tumors has revealed the existence of borderline forms between these tumors and endocrine tumors [20].
Impact of socioeconomic statues on pancreatic cancer was evaluated in a survival data from eight Cancer and Leukemia Group B (CALGB) protocols [21]. They were examined for patients with different tumors including pancreatic cancer (n=174). After accounting for differences in survival rate attributable to type of cancer, initial performance status, age, and 14 other protocol-specific prognostic indicators, the additional predictive value of socioeconomic status was evaluated. Ethnicity (W vs. non-W) was not a significant predictor of survival time, but income and education were. People with lower annual incomes (below US$ 5,000 per year in the years 1977 to 1981) and those with lower educational level (grade school only) showed survival times significantly shorter than those with higher income or education, respectively. These survival differences were associated with, but could not be fully explained by, severity of disease at initial presentation. Socieoeconomic status continued to exert a small but significant impact on cancer survival, even after controlling for all known prognostic variables. Economically and educationally disadvantaged cancer patients may require treatment programs that include education about treatment and compliance, even after an initial diagnosis is made and treatment is initiated. The pitfalls of retrospective study are well known, but some conclusions may well be drawn from this study. The strengths of this study include the relatively large sample size. Several limitations of the study should be mentioned. Medical care could not be evaluated adequately, because only broad categorizations of chemotherapy or radiotherapy were documented. This is a retrospective study and no information about general risk factors is available.
We did not find any significant differences in the mean ages between B and W, as well as between M and F, and no significant differences between B and W with respect to distributions across stages. Also, no interesting differences were observed in treatment specific outcomes between the two ethnicities. B patients seem to benefit at par compared to W patients. Prospective studies aimed at confirming these results, understanding ethnic differences in pancreatic cancer incidence and survival, genetics and/or molecular epidemiology, collecting data on availability and outcome to treatment and monitoring beyond the immediate postdiagnosis period to assess the medical care environment beyond the confines of pancreatic carcinoma are warranted
We thank Yolanda Graham for collecting data at Tumor Registry. This study was presented at ASCO 2003 in Chicago, IL, USA