Original Article - (2018) Volume 19, Issue 3
1Department of Nephrology and Hypertension, University Medical Center, Utrecht, The Netherlands
2Department of Surgery, Amsterdam Gastroenterology and Metabolism, Academic Medical Center, Amsterdam, The Netherlands
3Department of Surgery, University Medical Center, Utrecht, The Netherlands
4Department of Internal Medicine, St. Antonius hospital, Nieuwegein, The Netherlands
5Department of Surgery, St. Antonius hospital, Nieuwegein, The Netherlands
6Department of Gastroenterology and Hepatology, Erasmus MC University Medical Center, Rotterdam, The Netherlands
7Department of Surgery, Radboud University Medical Center, Nijmegen, The Netherlands
Received April 15th, 2018 - Accepted May 10th, 2018
Objective Intravenous fluid therapy is the cornerstone in early treatment of acute pancreatitis. Guidelines recommend a balanced salt solution to obtain a urinary output >0.5 ml/kg/h. However, the clinical practice of intravenous fluid therapy is largely unknown. Methods A post-hoc analysis was performed in a prospective multicenter cohort from 19 centers (August 2008 - June 2012) with predicted severe acute pancreatitis. The urinary output, plasma sodium, potassium, acid-base status, inflammation parameters and need for correction of biochemical abnormalities were evaluated. Results Among 205 included patients, the majority (n=144 (70%)) received normal saline, restricting our analysis to the impact of normal saline infusion. Patients received a median volume of 3000, 3200 and 3000 ml saline at day 1, 2 and 3 of admission, whereas 20 (14%), 18 (12%) and 9 (6%) patients had an insufficient diuresis (≤0.5 ml/kg/h) during those days. Diuretics were given to 68 patients (47%). Patients receiving normal saline had a significant decrease in pH after 48 hours (median from 7.43 to 7.28), acidosis developed in 12 patients (8%) and potassium supplementation was given to 97 patients (67%). Conclusions The current use of normal saline in patients with predicted severe acute pancreatitis is associated with low urine output, need for diuretics and frequent biochemical abnormalities, necessitating correction. Future studies should assess to what extent optimized fluid therapy can improve outcomes.
Diuresis; Fluid Therapy; Pancreatitis; Saline Solution, Hypertonic
SIRS systemic inflammatory response syndrome
Acute pancreatitis has a high annual incidence of 13 – 85/100,000 persons worldwide with mortality up to 20% in case of infected pancreatic necrosis [1, 2, 3, 4, 5]. Persistent (multi) organ failure further increases mortality to 35% [5]. Adequate fluid resuscitation and pain management are the cornerstones in early treatment of acute pancreatitis. Based on retrospective studies, early fluid resuscitation seems to be associated with a reduced incidence of systemic inflammatory response syndrome (SIRS), organ failure and mortality [6, 7]. Current international guidelines for the management of acute pancreatitis recommend vigorous infusion of a balanced salt solution (Ringer’s lactate 5-10 ml/kg/h) to maintain a urinary output of >0.5 – 1.0 ml/kg/h [8]. However, the recommendation for Ringer’s lactate is mainly based on one relatively small and early-terminated randomized trial in patients suffering from mild acute pancreatitis [9]. The latter might explain the fact that many physicians still treat acute pancreatitis patients with normal saline infusion.
The composition of the infusion fluid used has received increasing attention in recent years [10]. Balanced salt solutions better match the composition of blood plasma than the widely used normal saline [11]. In clinical trials in patients with pathologies other than pancreatitis (i.e. renal transplantation, dehydration, abdominal aortic aneurysm surgery), balanced salt solutions have been shown to prevent the development of hyperchloremic acidosis and to reduce the need for blood transfusion compared to resuscitation with normal saline [12, 13, 14, 15, 16, 17, 18]. In acute pancreatitis, balanced salt solutions have been suggested to reduce inflammation [9, 14]. Although metabolic and clinical advantages of balanced salt infusion are promising, convincing evidence for a clinical benefit is lacking. Most clinical outcome studies have used heterogeneous patient populations, various types and volumes of infusion fluids as well as different endpoints, which might have obscured the clinical benefit of balanced salt solutions. Moreover, the effects of large infusion volumes on urinary output, laboratory parameters (i.e. plasma sodium and potassium level, acid-base status) and morbidity (i.e. organ failure) in patients with acute pancreatitis are unknown.
We aimed to evaluate current clinical practice regarding infusion fluid (i.e. volume) in a homogenous multicenter patient population with predicted severe acute pancreatitis between 2008 and 2012, a period in which normal saline was predominantly used, and to describe biochemical parameters. We performed a post-hoc analysis on data collected during a randomized controlled trial, which consisted of a homogenous patient population that was treated with well-documented infusion therapy and of which biochemical parameters had been prospectively collected. Insight into the infusion policy and its effect on biochemical parameters will help to refine future recommendations on type and volume of infusion fluid in pancreatitis patients.
Study Population and Design
In this study a post-hoc analysis was performed in all patients of the ‘Pancreatitis, very early compared with normal start of enteral feeding’ (PYTHON) trial, a randomized controlled, multicenter trial in patients with predicted severe acute pancreatitis conducted in 19 Dutch hospitals (6 university medical centers and 13 large teaching hospitals) from August 2008 through June 2012 [19, 20]. The original trial protocol was approved by the institutional review board of the University Medical Center Utrecht and all the participating centers. Also patients or their legal representatives provided written informed consent [20].
Acute pancreatitis was defined by at least two of the following features: typical abdominal pain, a serum lipase or amylase that was more than 3 times the upper limit of normal, or characteristic findings on abdominal CT-scan [20]. Predicted severe disease was defined by an Acute Physiology and Chronic Health Evaluation (APACHE) II score of 8 or higher [21], a modified Glasgow score of 3 or higher [22], or a serum C-reactive protein (CRP) level higher than 150 mg/L [23], within 24 hours after presentation to the emergency department [20]. In the PYTHON trial, patients were randomized between early nasoenteric tube feeding (within 24 hours after randomization) or oral feeding (within 72 hours) [19, 20]. Intravenous fluid therapy was commenced at the emergency department, as judged by the attending physician, and continued throughout the first days. The trial protocol specified no specific type of fluid therapy. Vital signs and serum markers were used to titrate the amount of fluid [20].
Objective
The objective of the present study was to analyze the infusion regimen (i.e. volume) given during admission and to evaluate the urinary output, plasma sodium and potassium level, acid-base status, inflammatory parameters and the need for correction of biochemical abnormalities. Target urine production was defined as a urine output of >0.5 ml/kg/h according to the current international guidelines for the management of acute pancreatitis [8]. Hypernatremia was defined by a plasma sodium level >146 mmol/L, hypokalemia indicated a plasma potassium level <3.8 mmol/L and acidosis was defined by a pH <7.35.
Statistical Analysis
Categorical data were presented as frequencies and percentages, continuous data as mean and standard deviation (SD) or median and interquartile range (IQR), depending on normality of distribution. The association between the amount of fluid therapy and organ failure was evaluated using the chi-square test for categorical data. T-tests were used for normally distributed continuous variables and Mann-Whitney U-tests for non-normally distributed continuous variables. Correlations were determined with the Spearman’s rank correlation for nonnormally distributed continuous variables. A two-sided P value of less than 0.05 was considered to be statistical significant. All analyzes were performed using IBM SPSS Statistics for Windows (version 21, IBM Corp, Armonk, NY, USA).
Baseline Characteristics and Infusion Regimen
The study population consisted of 205 patients with predicted severe acute pancreatitis. Mean age was 65±15 years. Baseline characteristics are summarized in Table 1.
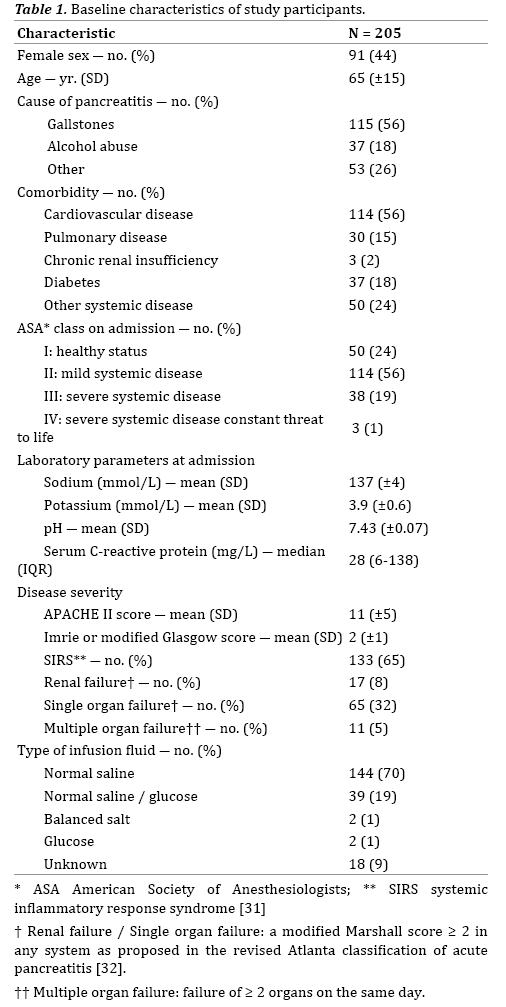
The majority of patients received intravenous fluid resuscitation with normal saline (144 patients, 70%), while only 2 patients (1%) were treated with a balanced salt solution. Forty-one patients (20%) were treated with a glucose-containing solution and in 18 patients (9%) the type of infusion fluid was not specified.
In patients receiving normal saline, the median volume was 3000, 3200 and 3000 ml at day 1, 2 and 3 respectively, thereafter the volume decreased quickly (Figure 1). Both total volume as well as volume per kg body weight were relatively stable during the first 72 hours, but decreased thereafter. Because the majority of patients were treated with normal saline, no comparison could be made between the administration of normal saline and a balanced salt solution. Therefore further analysis on biochemical parameters was performed solely in the patients receiving normal saline.
Diuresis in Patients Receiving Normal Saline
On the day of admission, patients who were treated with normal saline had a limited diuresis that increased in the following days (Figure 2). Table 2 shows patients who achieved the target urine production of >0.5 ml/kg/h during the first 72 hours. In 111 (77%), 89 (62%) and 85 (59%) patients the data on urine production at 24, 48 and 72 hours, respectively, were lacking.
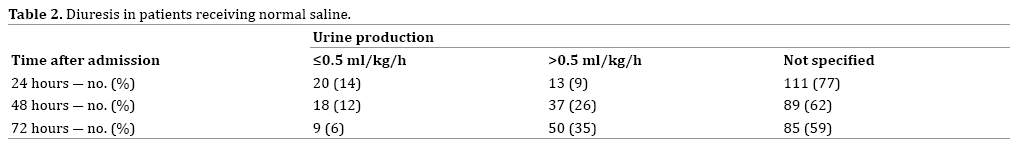
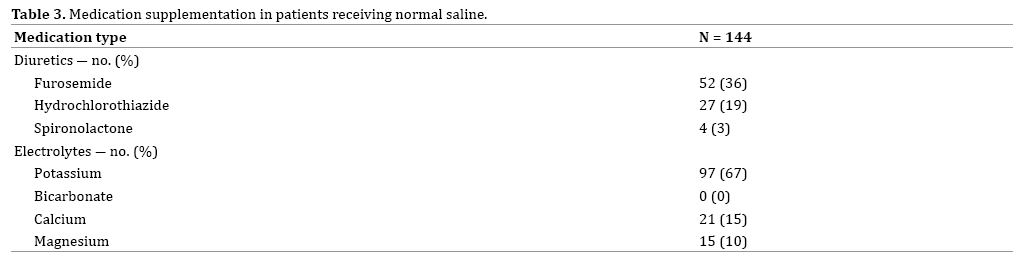
Patients who did not reach the target urine output had a median diuresis of 0.39 ml/kg/h (IQR 0.33 – 0.47 ml/ kg/h) at 24 hours, 0.37 ml/kg/h (IQR 0.25 – 0.41 ml/kg/h) at 48 hours and 0.37 ml/kg/h (IQR 0.12 – 0.44 ml/kg/h) at 72 hours. As a result of the large volume of infusion fluid administered with a limited diuresis, the fluid balance was positive during the first 3 days (Figure 3), with a significant mean weight increase of 3.1±3.7 kg (P=0.002). Diuretics were given to 68 patients (47%) during admission. In these cases, furosemide was primarily used (Table 3).
Plasma Electrolytes and Acid-Base Status in Patients Receiving Normal Saline
The plasma sodium level increased significantly during admission, compared to baseline, for patients receiving normal saline (1.8 mmol/L at 24 hours, 2.6 mmol/L at 48 hours and 2.2 mmol/L at 72 hours). Hypernatremia was present in 2 patients (1%) at 24 hours, 4 patients (3%) at 48 hours and 6 patients (4%) at 72 hours.
There was a significant decrease of the mean plasma potassium from 3.9±0.6 mmol/L to 3.7 ± 0.5 mmol/L at 72 hours. During admission 97 patients (67%) were treated with potassium supplementation (Table 3). Hypokalemia occurred frequently in patients receiving normal saline, with 66 patients (46%) at 24 hours, 77 patients (53%) at 48 hours and 89 patients (62%) at 72 hours, while at these times more than 50% already was treated with oral or intravenous potassium supplementation.
In addition, during the first 48 hours, administration of normal saline was associated with a significant decrease in pH from 7.43±0.07 to 7.28±0.13 (Figure 4) with subsequent development of an acidosis (pH <7.35) in 8% of patients.
Morbidity and Mortality in Patients Receiving Normal Saline
The patients in this study with predicted severe acute pancreatitis had significant morbidity and mortality. At baseline 67% met the criteria for severe inflammatory response syndrome. At that same time, 6% of the patients receiving normal saline had multiple organ failure, 8% had renal failure and 31% had single organ failure. Six months after inclusion, 8% of the patients had died.
The present study shows that, between 2008 and 2012, fluid therapy in patients with predicted severe acute pancreatitis was suboptimal. Most patients were treated with normal saline with volumes less than currently recommended. Due to this fact, no comparison could be made regarding outcomes between patients receiving normal saline and patients receiving a balanced salt solution. For the patients receiving normal saline, the urinary output target seemed to be reached in only a minority of patients and in a substantial number of patients hemodynamic and metabolic disturbances occurred. Regarding the use of normal saline in this patient cohort it should be noted that the guidelines, which recommend aggressive infusion of a balanced salt solution aiming at a urinary output of >0.5 ml/kg/h, were introduced one year after the randomization for the PYTHON trial was finished [8]. Despite the fact that the diuresis goal was reached and registered in only 35% of patients, a significant mean weight increase occurred with the need for administration of diuretics in 47% of patients. In addition, patients receiving normal saline infusion had a significant increase in plasma sodium level in the first 72 hours and a significant decrease in plasma potassium level despite potassium supplementation was given in 67% of these patients. Finally, acidosis developed in 8% of the patients.
This study found that that infusion therapy with normal saline led only in a minority of patients to the currently recommended urine output of >0.5 ml/kg/h, while many patients suffered from volume overload as indicated by the applied diuretic therapy. The main goal of infusion therapy is to ensure adequate tissue perfusion. However, one might question whether urine output truly reflects tissue perfusion, which possibly explains the low level of recommendation (weak) in the current international guidelines [8]. Interestingly, the amount of chloride a specific infusion fluid contains, plays an important role in the effect of infusion fluid on diuresis. Infusion fluids containing supra-physiological concentrations of chloride, as is the case with normal saline, will induce intrarenal vasoconstriction, suppress renin and subsequently decrease glomerular filtration rate [11, 24, 25]. The ensuing decrease in diuresis increases the risk of intravascular volume overload. One might speculate that with the use of the recommended balanced salt solutions, with a more physiological chloride content, diuresis will better reflect intravascular volume, and therefore prevent the need for diuretic therapy [11].
Currently, there are no comparable studies that have described the use of normal saline in patients with predicted severe acute pancreatitis and their urinary output, need for diuretics, plasma electrolytes and pH. Two previous studies have only described other biochemical parameters and clinical outcomes. Aboelsoud et al. investigated 198 patients with acute pancreatitis, admitted to the intensive care unit (ICU), who received a median amount of 5600 ml normal saline (130 patients) or 7200 ml Ringer’s lactate (68 patients) in the first 24 hours [26]. Patients receiving normal saline had a significant higher mortality, decrease in serum bicarbonate and increase in serum chloride, as compared to those receiving Ringer’s lactate. However, the ICU stay was significantly longer in the Ringer’s lactate group. Wu et al. compared 21 patients who were treated with normal saline with 19 patients treated with Ringer’s lactate and showed that infusion of a mean volume of 4500 ml Ringer’s lactate, led to an 84% reduction in SIRS and a significant lower CRP level at 24 hours from baseline [9]. The study of Aboelsoud is comparable to the present study regarding the number of patients receiving normal saline. However, both studies of Aboelsoud and Wu used a larger volume of infusion fluid, described a shorter time period and did not investigate the urinary output, use of diuretics, plasma electrolytes and pH. In addition, there is one study that investigated 103 patients who received 1000 ml Ringer’s lactate or normal saline, followed by a 5% glucose solution (1000–1500 ml) and a multi-electrolyte solution (500–1000 ml) [27]. There was no significant difference in pancreatic necrosis, administration of enteral nutrition, duration of hospital stay and mortality between the two groups. It is difficult to compare the latter study to our study because of an entirely different composition of infusion fluid. The present study gives an overview of biochemical parameters in severe acute pancreatitis patients receiving a large volume of normal saline, although it was not possible to confirm causality in our post-hoc analysis.
The development of acidosis in the present study is in agreement with previous studies on infusion therapy in other diseases. Four studies in kidney transplant patients showed that normal saline infusion (2868 – 6100 ml) significantly induced metabolic acidosis (pH 7.28 – 7.36), whereas infusion of a balanced salt solution did not affect the acid-base status [16, 17, 28, 29]. However, it is important to note that renal transplant patients differ from pancreatitis patients with respect to the underlying disease and therapeutic interventions. Up to now, only 2 studies have investigated a non-surgical population. Williams et al. studied healthy volunteers who were treated with normal saline and, after a cross-over, received Ringer’s lactate, wherein normal saline led to a significant decrease of pH (from 7.42 to 7.38) and increase in serum sodium level (from 140 to 141 mmol/L) [12]. Hasman et al. confirmed the decrease in pH (from 7.40 to 7.36) in dehydrated patients in the emergency department who were treated with normal saline [18]. It is of note that the follow up in these two latter studies is relatively short (1-2 hours compared to more than 3 days in the present study), thereby possibly overlooking metabolic disturbances that occur after 2 hours.
A significant decrease in serum potassium level, as seen in our study, has so far been shown in one other study. Chua et al. retrospectively studied patients with a diabetic ketoacidosis who received 4425 ml of normal saline and had a significant decrease in serum potassium level (from 5.6 to 4.3 mmol/L), however this effect might also be explained by other interventions like insulin infusion [30]. The previous mentioned studies of Hadimioglu and Hasman showed a non-significant decline in serum potassium with normal saline and O’Malley even showed an increase in serum potassium (from 4.2 to 5.1 mmol/L) [16, 17, 18]. The result of this last study could be explained by the fact that the kidney transplantation in itself can be associated with a potassium release due to tissue damage. Interestingly, despite the fact that balanced salt solutions contain potassium, the infusion of these solutions was not associated with a significant increase in potassium.
The most important limitations of the current study are the lack of randomization and retrospective design with post-hoc analysis and concomitant missing data. However, it is the first study outlining the actual clinical practice in the Netherlands regarding the use of infusion fluid in predicted severe acute pancreatitis. In addition, it is tempting to speculate that infusion policies play a crucial causal role in the development of metabolic disturbances and fluid overload.
In conclusion, low urine output, need for diuretics and biochemical abnormalities necessitating correction were seen in a considerable amount of patients with predicted severe acute pancreatitis, treated with normal saline. Future intervention studies should assess to what extent optimized fluid therapy (i.e. amount and composition) can improve morbidity and mortality in patients with predicted severe acute pancreatitis.
AES, JvG, ACA, MGB and MBR designed the protocol of the present study. AES, CB, OJB and SvB collected the data. AES and JvG analyzed the data. AES drafted the manuscript together with JvG, ACA, OJB, MGB and MBR. All co-authors (JvG, ACA, CB, OJB, WJB, HCS, MJB, HvG, SvB, MGB and MBR) critically edited the manuscript and approved the final version.
There are no conflicts of interest and no sources of funding.