- (2010) Volume 11, Issue 5
Farshad Frozanpor1,2, Nils Albiin3, Stefan Linder1,Ralf Segersvärd2, Lars Lundell2, Urban Arnelo2
1Division of Surgery, Department of Clinical Science and Education, Karolinska Institutet, Sädersjukhuset
2Division of Surgery and 3Medical Imaging and Technology, Department of Clinical Science, Intervention and Technology (CLINTEC), Karolinska Institutet/Karolinska University Hospital. Stockholm, Sweden
Received May 15th, 2010 - Accepted July 8th, 2010
Context Resection of the body and tail of the pancreas (distal pancreatectomy) is associated with high postoperative morbidity, most of which is due to leakage from the pancreatic transection surface. Objective The aim of the current study was to analyze factors which may affect the risk of pancreatic fistula formation. Patients All consecutive distal pancreatectomies prospectively registered in our hospital database from 1999 to 2007 were included. Clinically relevant pancreatic fistula grades B and C, defined according to the International Study Group on Pancreatic Fistula (ISGPF) definition were assessed. Main outcome measures The impact of patient, tumor, surgery, and radiology-related factors on the risk of pancreatic fistula formation were assessed by univariate and multivariate analyses. Results A distal pancreatectomy was performed in 51 patients (median age: 59 years; range: 26-76 years), 22 of whom had malignant and 29 benign or premalignant disease. Pancreatic fistulas were diagnosed in 17 (33.3%) of the patients. An additional three patients had a local abscess without apparent but assumed pancreatic leakage. Multivariate analysis showed that pancreatic fistulas occurred more frequently after hand suturing of the transection area versus the use of a stapler (69.2% vs. 21.1%; OR: 40.4, 95% CI: 3.36-486; P=0.004) and a large volume of the pancreatic remnant (greater, or equal to, 34 cm3 ) increased the subsequent risk of pancreatic fistula (57.1% vs. 20.8%; OR: 6.14, 95% CI: 1.14-39.0; P=0.035). Conclusions Development of pancreatic fistula after distal pancreatectomy remains a challenge. The volume of the remaining pancreas and the technique of closure of the transected pancreas were found to affect this risk, thus allowing future preventive measures to be explored and evaluated in clinical trials.
Pancreatectomy; Pancreatic Fistula; Surgical Stapling
ISGPF: International Study Group on Pancreatic Fistula
Pancreatic fistula formation remains the Achilles heel of pancreatic surgery and continues to challenge clinicians since it is the main cause of postoperative morbidity and mortality [1, 2]. Several factors, such as a fatty, soft, non-calcified, non-fibrotic gland [3, 4], have been suggested to increase the risk of pancreatic fistulae. In addition, the underlying pathology, e.g. duodenal, ampullary, and distal common bile duct lesions, have been shown to increase the risk. Despite this knowledge, the definition of the details of the risk profile of each individual patient is still an enigma [5, 6].
Resection of the pancreas to the left side of the superior mesenteric vein, defined as a distal pancreatectomy, is performed less frequently than resections of the pancreatic head [7]. Both a lower incidence of disease affecting this part of the pancreas and more advanced stages of cancer at the time of diagnosis explain this difference [7]. Distal pancreatectomy is considered by many surgeons to be a less demanding and complex operation than a Whipple procedure, a view which is far from well substantiated [8, 9]. With centralization of pancreatic resections, the mortality rate has decreased considerably [10, 11, 12, 13, 14, 15, 16, 17, 18], but morbidity remains substantial [10, 11, 12, 13, 14, 15], even after distal pancreatectomy. Overall postoperative morbidity has been reported to range from 9 to 57% [1, 3, 10, 12, 19, 20]. The most common and important postoperative complication after distal pancreatectomy is pancreatic fistula, which may manifest itself as a frank fistula or an intra-abdominal fluid collection. Pancreatic fistula is associated with both local and general complications (e.g. intraabdominal fluid abscesses, wound infection, delayed gastric emptying, respiratory complications and sepsis) but it has additional important implications in terms of the need for revisional surgery and drainage with a prolonged hospital stay [11, 13].
Pancreatic fistula is thought to depend on a variety of factors, some of which are surgeon-dependent [21, 22, 23]. There is, for example, significant variation in and debate about which surgical technique should be used for closure of the pancreatic transection area [5, 24, 25, 26, 27, 28, 29, 30]. Besides this, other risk factors are poorly characterized.
The aim of the current study was to analyze factors which may affect the risk of pancreatic fistulae after distal pancreatectomy.
A study was conducted on a cohort of consecutive patients undergoing distal pancreatectomy between March 1999 and December 2007 at the Karolinska University Hospital. All data on demographics, clinicopathological features, operative information, complications and in-hospital mortality were collected prospectively in the local pancreatic database.
Definition of Pancreatic Fistula
Patients were categorized as having developed a clinically relevant fistulae (i.e. grade B or C) based on the definitions of the International Study Group on Pancreatic Fistula (ISGPF). In other words, a clinically significant pancreatic fistula is a fistula requiring any therapeutic intervention (grade B) or a fistula with severe clinical sequelae (grade C). The incidence of biochemical leakage (regarded as grade A), defined as any measurable output on, or after, the 3rd postoperative day from an operatively positioned abdominal drain and displaying pancreatic amylase more than 3 times the upper serum reference value, was not included in the analyses of this study.
Preoperative computed tomography or magnetic resonance imaging were analyzed by the same radiologist who was blinded to the postoperative course. The volume of the pancreatic remnant was measured using a Voxar® 3D workstation (Barco NV, Kortrijk, Belgium) with 3D segmentation and volume calculation (Figures 1 and 2). The length and width of the resection plane were measured. The caliber of the main pancreatic duct was measured in the resection plane and in the head of the pancreas, as was the distance of the resection margin from the lesion.
The study protocol conforms to the ethical guidelines of the “World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004. The study protocol was approved by the Ethics Committee of the Karolinska University Hospital, Karolinska Institute, Sweden.
Binary logistic regression analysis was performed to identify the risk factors for pancreatic fistulae, with and without simultaneous adjustment for competing risk factors. Crude associations were studied in a univariate model which was followed by a multivariate analysis of significant factors. Robust standard errors were computed to account for the clustering of patients by a single surgeon. The associations were presented as odds ratios (ORs) with 95% confidence intervals (CIs). The unpaired Students’ t-test was used to compare mean values. Data are presented as medians and ranges or frequencies. All tests of statistical significance were two-sided, and statistical significance was considered to occur at alpha less than 0.05. The statistical analyses were performed using SPSS 17.0 software (SPSS Inc, Chicago, IL, USA).
Patients, Surgery, and Diagnoses
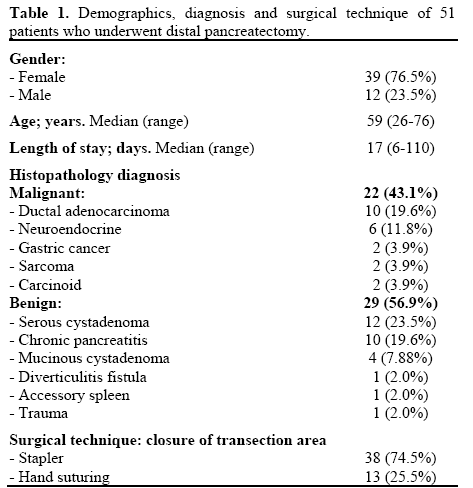
During the study period, a total of 51 patients (39 females, 12 males) having a median age of 59 years underwent distal pancreatectomy. Splenectomy was carried out in 47 patients (92.2%) and the median hospital stay was 17 days. The diagnosis was malignant in 22 patients (43.1%) and benign or premalignant in 29 (56.9%) patients. The transection area was closed by means of a stapler in 38 cases (74.5%) and by hand suturing in 13 (25.5%). These data are shown in detail in Table 1.
Surgical Complications
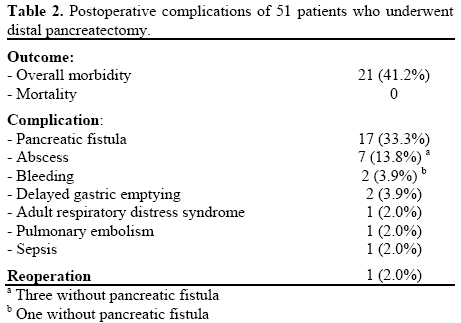
Overall, 21 patients (41.2%) experienced postoperative complications (Table 2). The most common complication was pancreatic fistula, which was observed in 17 patients (33.3%). Three of the 7 patients with intra-abdominal abscesses had a local abscess without apparent pancreatic leakage. The occurrence of a pancreatic fistula increased the median length of hospitalization from 11 (range: 6-16 days) to 30 days (range: 14-110 days) (P=0.014). One patient required reoperation (2.0%); otherwise, complications were treated conservatively without any mortality (Table 2).
Risk Factor Analysis
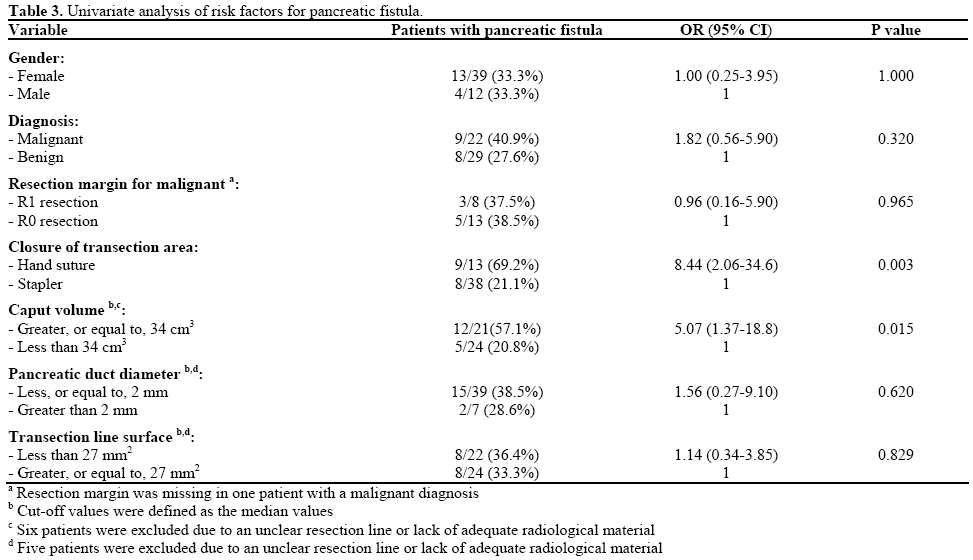
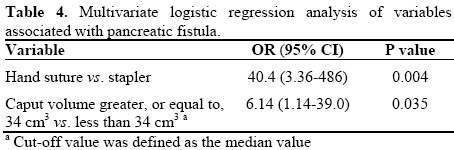
Pancreatic fistulae occurred more frequently after hand suturing (9/13, 69.2%) as compared to the use of a stapler (8/38, 21.1%). At univariate analysis, hand suturing of the transection surface significantly increased the risk of a pancreatic fistula (OR: 8.44; 95% CI: 2.06-34.6; P=0.003). A radiological median value volume of the remaining gland equal to, or greater than, 34 cm3 exerted a negative impact on the risk of a pancreatic fistula (OR: 5.07; 95% CI: 1.37- 18.8) (Table 3). In the subsequent multivariate analysis, both factors remained independent risk factors for pancreatic fistulae (Table 4).
It has clearly been demonstrated that distal pancreatectomy is associated with significant morbidity, which is very much related to the occurrence and perpetuation of a pancreatic fistula. The internationally recognized classification of pancreatic fistula [31] is very helpful in attempts to define those at risk. However, the design of the present analysis, as that of many other studies in the field, does not allow a comprehensive elucidation of issues and consequences related to those fistulae which are grade A and B [1, 5, 10, 20, 22, 32]. However, it is reasonable to assume that abscess formation in close conjunction with the resection area is closely linked to such phenomena. We did not include such abscesses in the final analyses of the pancreatic fistulae because we were unable to detect any pancreatic juice remnant at the time of abscess puncture or drainage.
The surgical method for closure of the transected pancreatic gland is still a matter of debate. A recently performed careful survey of the current literature [5, 19, 24, 33] brought into focus the fact that most studies were of suboptimal quality and underpowered. The conclusion was that additional well-designed, randomized clinical trials were urgently needed. The current study reporting a strong association between pancreatic fistulae and the use of a manual suturing technique reinforces the need for such trials. It is clear that laparoscopic resection of the body and tail of the gland is preferred in many institutions [34, 35, 36]. This operative approach does not resolve the problem of leakage and the morbidity rate is comparable to open procedures [37].
A novel finding of the present study consisted in the association between the size of the remaining gland and the risk of pancreatic fistulae. This is a plausible and logical observation since the larger the volume of the remaining gland, the greater the quantity of actively secreting parenchyma with the potential of exerting detrimental, digestive effects on the sealed transection area. This brings to our attention mechanisms by which the secreted juice from the remaining pancreatic head may be deviated away from the area of the closed transection line. Downstream control by use of a pancreatic stent would be such an option [38]; again something which has to be explored in a clinical trial where enrolled patients must be stratified also with regard to the volume of the tissue drained through the papilla.
We were unable to find any impact of other radiological variables, such as pancreatic and biliary duct diameter, area of the transected surface or gross amount of resected tissue. In this context, it is interesting to recall a recent observation in which dynamic magnetic resonance imaging has been hypothesized to be able to to assess the texture of the gland tissue in the form of high and normal contrast enhancement, thereby having the potential of predicting the risk of leakage after a Whipple resection [32]. If this technology is combined with volume assessments, a novel and precise instrument, with an obvious clinical potential, might well be launched and therefore deserves to be tested in well-designed clinical trial protocols. In conclusion, the development of pancreatic fistulae after distal pancreatectomy remains a challenge. The technique of closure of the transected surface of the pancreas and the volume of the remaining gland were found to affect the risk of pancreatic fistulae.
Authors report no conflict of interest