Research Article - (2023) Volume 8, Issue 1
Impact of Socioeconomic Status on Adolescent Bariatric Surgery Outcomes in a Quaternary Pediatric Hospital
Mauney Erin1,
Desai Nirav K2,
Mitchell Paul3,
Carmine Brian4,
Fayemi Annemari4 and
Richmond Camilla2*
1Department of Pediatrics, Boston Children’s Hospital, United States
2Department of Gastroenterology, Nutrition, and Hepatology, Boston Children’s Hospital, United States
3Institutional Centers for Clinical and Translational Research, Boston Children’s Hospital, United States
4Department of Surgery, Boston Children’s Hospital, United States
*Correspondence:
Richmond Camilla,
Department of Gastroenterology, Nutrition, and Hepatology, Boston Children’s Hospital,
United States,
Tel: 5128970435,
Email:
Received: 31-Jan-2023, Manuscript No. IPJCO-23-15743;
Editor assigned: 02-Feb-2023, Pre QC No. IPJCO-23-15743 (PQ);
Reviewed: 16-Feb-2023, QC No. IPJCO-23-15743;
Revised: 21-Feb-2023, Manuscript No. IPJCO-23-15743 (R);
Published:
28-Feb-2023, DOI: 10.36648/2572-5394.23.08.006
Abstract
Background: Research on the impact of socioeconomic characteristics on bariatric surgical outcomes in adolescents and young adults is limited.
Objectives: To determine whether race, household income, or insurance type impacted body mass index (BMI) at time of surgery and weight loss at 1 year post-surgery.
Methods: Adolescents and young adults who underwent bariatric surgery at a single center (Boston Children’s Hospital) between 2011 and 2019 were retrospectively reviewed. The primary outcome was BMI percentile at time of surgery and one and 2 years post-surgery.
Results: Among 54 subjects, 83% were female. Racially, 56% were White, 33% were Hispanic, 9% were Black, and 2% were Chinese (cumulatively referred to as people of color [POC]). 22% were publicly insured. There was no statistical difference in BMI at time of neither surgery, nor weight loss at 1 year for subjects on public vs. private insurance, nor by household income. BMI for POC subjects was 8.5% higher than for White subjects’ at time of surgery and 1 year post-op (P=0.02).
Conclusion: Relative to the pool of adolescents and young adults with obesity, our patients were disproportionately female, White, and privately insured, suggesting disparities in surgical access. POC subjects demonstrated less post-surgery weight loss than White subjects, but other socioeconomic variables did not impact weight loss.
Keywords
Adulthood; Weight loss; BMI; Surgery
INTRODUCTION
The prevalence of severe pediatric obesity, defined as a BMI 120% or more than the 95th BMI percentile continues to rise, affecting nearly 6% of children and teens in the United States. Obesity related conditions, including type 2 diabetes mellitus, hypertension, obstructive sleep apnea, and non-alcoholic fatty liver disease are likewise increasing in prevalence. Because 88% of adolescents with BMI>99th percentile remain obese in adulthood, there is an urgent need to develop effective, accessible treatments for pediatric obesity. Adolescents with severe obesity demonstrate minimal change in BMI with lifestyle interventions and there are few FDA-approved pharmacologic options for adolescents. Bariatric surgery in adolescents results in durable weight loss of nearly 30% of pre-surgical BMI, along with resolution of comorbidities such as hypertension and type 2 diabetes mellitus [1-4].
Although pediatric bariatric surgeries are becoming more common, with the rate of such surgeries increasing 1.8 fold from 2012 to 2016, less than 0.4% of pediatric patients eligible for the surgery undergo it (similar to the 0.5% utilization rate among eligible adults) and pediatric weight loss surgery makes up <1% of total weight loss surgeries in the US each year. However, there is a growing evidence base that bariatric surgery is effective in the management of severe pediatric obesity and obesity related conditions [4-9].
Disparities in access are key drivers of the discrepancy between those eligible for weight loss surgery and those who receive it. It is well documented that the prevalence of pediatric obesity is disproportionately higher among those on public insurance (39.6% of publically insured children have obesity vs. 26.7% of privately insured). However, public insurance plans of 44 states cover bariatric surgery among adults, and all states are required to cover all “medically necessary” services for comprehensive obesity services through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. Despite this apparent accessibility to surgical weight management, a recent survey of the National Inpatient Sample, representing nearly 20% of all hospital discharges, found that 72.8% of adult patients undergoing bariatric surgery were privately insured. In the pediatric population, similarly, approximately 80% of patients undergoing bariatric surgery are privately insured. Furthermore, independent of insurance type, adolescents seeking bariatric surgery appear to face additional barriers to care, with one study reporting that fewer than half of adolescents who met clinical criteria for surgery received insurance approval on their first request, as opposed to over 80% of adults [8,10-13].
In addition to socioeconomic barriers, there are also racial and sex disparities in access to bariatric surgery, with White adolescents undergoing bariatric surgeries 2.5 times more frequently than Black and Hispanic patients, despite severe obesity being more prevalent in these populations. Finally, among both adults and adolescents, male patients are less likely to be referred for bariatric surgery than female patients [14-16].
Alongside inequities in access, there are well-documented disparities in surgical outcomes by socioeconomic status among adults undergoing bariatric surgery. For example, a large national case control study of adult patients undergoing bariatric surgery demonstrated that publicly insured patients have an increased risk of complications compared to privately insured patients, an effect that is not mediated solely by access to care. In adults, studies suggest that Black patients have lower weight loss at one year than White patients, independent of income or payer type, although this finding was not consistent among adolescents [14,17,18].
Given that the majority of the literature in adolescent bariatric surgery relies on administrative databases, there is a paucity of evidence regarding granular, patient level outcomes by socioeconomic status. This study aimed to characterize the population of adolescents undergoing bariatric surgery at a single, large, quaternary pediatric hospital between 2011 and 2019. We investigated whether BMI at time of referral for surgery and at one year post-surgery varied based on race, sex, household income, and insurance type (public vs. private).
Methods
This was a retrospective, single-arm cohort study of all adolescents
who underwent bariatric surgery at Boston Children’s Hospital
between October 2011 and January 2019. Demographic and
clinical data was abstracted from the electronic medical record.
Median household income, census tract minority percentage,
and census tract poverty percentage were determined using the
Federal Financial Institutions Examination Council geocoding system
based on the census tract and the patient’s address. Race
was determined by self-report during registration. Insurance type
(private vs. public) was determined by the patient’s primary insurance
at time of surgery. The decision to use the insurance on record
at time of surgery was due to the high frequency of patients
who reported different insurance payers from the time of initial
visit to time of surgery. The primary outcome assessed was BMI
as a percent of the 95th percentile of BMI for age at time of surgery
and one year post-surgery, based on the Centers for Disease
Control growth charts.
Statistical Methods
Categorical variables are summarized by frequency count and
percentage and compared across dichotomous groups by Fisher
exact test. Continuous variables are summarized as mean ± standard
deviation (SD) and compared across dichotomous groups by
Student’s t-test. The primary outcome, % of the 95th percentile of
BMI for age, was calculated using CDC growth charts and the SAS
program provided at www.cdc.gov. Height and weight measurements
were obtained at clinic visits from the time of the initial
visit until up to 2 years post-surgery; however, due to the sparsity
of data, the analysis was limited to anthropometry measurements
obtained between 30 months pre-surgery and 12 months
post-surgery. Beyond these limits, the number of observations
available for subjects with public insurance is <5 within any 6
month interval.
The primary outcome was modelled over time with a repeated
measures random intercept generalized linear model with cubic
B-splines and knots at 6 months prior to surgery, the time
of surgery, and 6 months post-surgery. The shape of the model
and placement of knots was informed by a nonparametric locally
weighted scatterplot smoothing (LOESS) regression. Changes over
time were adjusted for outcome at the initial clinic visit and were
evaluated for the main effect of insurance type as well as an interaction
effect for insurance type by time. Comparison of more than
two groups was adjusted for multiplicity by Holm’s step down
Bonferroni surgery. All point estimates are presented with 95%
confidence interval (95% CI), with P<0.05 considered statistically
significant. Statistical analysis was performed with SAS version 9.4
(Cary, NC).
Results
Demographics
A total of 55 patients underwent bariatric surgery at our centre
from 10/31/2011 to 01/04/2019. One subject who underwent an
experimental endoscopic sleeve gastrectomy surgery was excluded
from analysis. Patient characteristics are reported in Table 1.
The majority (n=45, 83%) were female. 24 patients (44%) were Black, Latino/a, and Asian people of color (POC). The age at initial
visit ranged from 13.7-22.9 years (mean 17.2 ± 1.8). The majority
were privately insured at time of surgery (n=42, 78%) with a mean census tract household income of $ 88,337 ± 38,390.
| Characteristics |
Overall |
Public |
Private |
P |
| (n=54) |
(n=12) |
(n=42) |
| Subject |
| Female sex |
45 (83%) |
10 (83%) |
35 (83%) |
1 |
| People of Color1 |
24 (44%) |
5 (42%) |
19 (45%) |
1 |
| Age at initial visit (y), (range 13.7-22.9) |
17.2 ± 1.8 |
17.3 ± 1.0 |
17.2 ± 1.9 |
0.81 |
| Family |
| Household income ($) (range $ 14,634-172,941) |
88,337 ± 38,390 |
72,454 ± 42,497 |
93,390 ± 36,344 |
0.23 |
| <$ 75,000 |
14 (26%) |
5 (42%) |
9 (21%) |
|
| $ 75,000-$ 100,000 |
21 (39%) |
5 (42%) |
16 (38%) |
|
| $ 100,000 + |
19 (35%) |
2 (17%) |
17 (40%) |
|
| Number of insurance plans on the date of initial visit (n=1 unknown) |
|
|
|
0.25 |
| 1 |
24 (45%) |
7 (64%) |
17 (40%) |
|
| 2 |
21 (40%) |
4 (36%) |
17 (40%) |
|
| 3 |
8 (15%) |
0 (0%) |
8 (19%) |
|
| Number of insurance plans on the date of surgery (n=2 unknown) |
|
|
|
0.002 |
| 1 |
30 (58%) |
12 (100%) |
18 (45%) |
|
| 2 |
18 (35%) |
0 (0%) |
18 (45%) |
|
| 3 |
4 (8%) |
0 (0%) |
4 (10%) |
|
| Surgery |
| Months from initial visit until surgery (range 3.9-34.9) |
11.7 ± 7.0 |
12.1 ± 5.5 |
11.5 ± 7.4 |
0.82 |
| Age at surgery (y), (range 14.4-24.0) |
18.2 ± 1.9 |
18.3 ± 1.1 |
18.2 ± 2.0 |
0.75 |
| Type of surgery |
|
|
|
0.74 |
| Sleeve |
31 (57%) |
6 (50%) |
25 (60%) |
|
| Bypass |
23 (43%) |
6 (50%) |
17 (40%) |
|
| No. of overnights, n=1 unknown |
2.8 ± 0.7 |
3.0 ± 0.9 |
2.8 ± 0.7 |
0.32 |
| 1 |
1 (2%) |
0 (0%) |
1 (2%) |
|
| 2 |
17 (32%) |
4 (33%) |
13 (32%) |
|
| 3 |
26 (49%) |
4 (33%) |
22 (54%) |
|
| 4 |
9 (17%) |
4 (33%) |
5 (12%) |
|
Note: 1Includes Black (n=5), Hispanic (n=18), and Chinese (n=1).
Table 1: Subject, family, and surgical characteristics (n=54).
Pre-Surgical Process and Surgical Length of Stay
The average number of months from initial visit to surgery was
11.7 ± 7.0 and did not vary significantly between publicly and privately
insured patients. However, as reported in Table 2, younger
patients had fewer months from initial visit until surgery (9.4 ±
4.5 months for patients aged 14-17 y vs. 14.5 ± 8.4 months for
patients aged 18-24 y, P=0.01). The type of surgery did not vary by
payer type. The type of surgery, RYGB vs. sleeve gastrectomy was
similar across the cohort with a small majority undergoing sleeve
gastrectomy (n=31, 57%). The average length of stay following
surgery was 2.8 ± 0.7 nights and did not vary by payer type.
Post-Surgery BMI Outcomes
Based on the repeated measures model, the mean (95% confidence
interval) among all patients combined for percentage of
95th percentile for BMI was 159% (155%-163%) at 3 months prior
to surgery (a time point which for which all patients were enrolled
for medically supervised weight loss, and thus had data available)
and 149% (145%-153%) at the time of surgery. This fell to 108%
(104%-113%) at 6 months post-surgery (Figure 1).

Figure 1: Change in percent of 95th percentile for BMI for all patients.
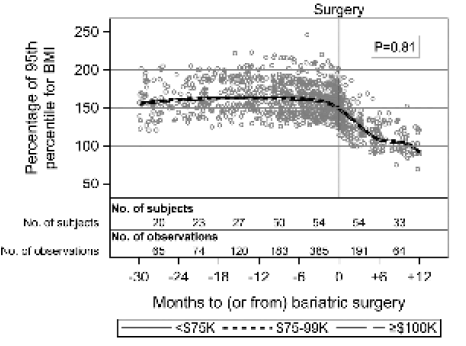
The change in BMI did not vary for: publicly insured vs. privately
insured patients (P=0.93) (Figure 2), census tract household
income (P=0.81) (Figure 3), sex, age, type of surgery, or length
of stay (Table 3). As compared to White patients, POC patients
demonstrated a mean % of 95th percentile for BMI change that
was 8.5% lower (95% confidence interval 1.4%-15.5%), P=0.02
(Figure 4 and Table 2). Similarly, patients from a census tract with
a racial minority percentage ≥ 40% had a mean percentage of 95th percentile for BMI change that was 8.3% lower than those from
a census tract with a minority percentage <40% (95% confidence
interval 0.7% to 15.8%), P=0.03 (Table 2). Patients older than
18 years old had a mean percentage of 95th percentile for BMI
change that was 7.0% lower than those under 18 years (95% confidence interval 0.1% to 14.0%), P=0.05 (Table 2), although there
was not a monotonically increasing effect when looking at the age
by tertiles and the evidence of an effect by age is thus weak.

Figure 2: Change in percent of 95th percentile for BMI over time for publicly insured vs. privately insured patients.
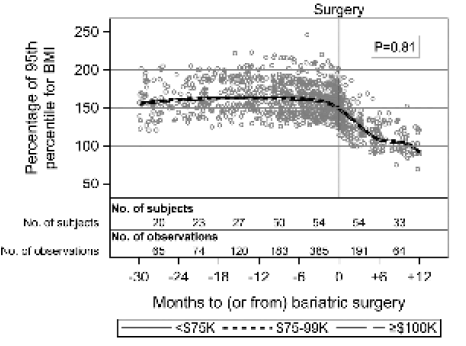
Figure 3: Change in percent of 95th percentile for BMI over time by census tract household income.

Figure 4: Change in percent of 95th percentile for BMI over time for Non-White vs. White patients
| Characteristics |
14-17y |
18-24 y |
P |
| (n=30) |
(n=24) |
| Subject |
| Female sex |
24 (80%) |
21 (88%) |
0.7 |
| POC |
12 (40%) |
12 (50%) |
0.6 |
| Family |
| Household income ($), mean ± SD |
91,210 ± 43,279 |
85,647 ± 31,884 |
0.6 |
| <$ 75,000 |
9 (30%) |
5 (21%) |
|
| $ 75,000-$ 100,000 |
9 (30%) |
12 (50%) |
|
| $ 100,000 or more |
12 (40%) |
7 (29%) |
|
| Number of insurance plans on the date of surgery (n=2 unknown) |
|
|
0.7 |
| 1 |
16 (57%) |
14 (58%) |
|
| 2 |
9 (32%) |
9 (38%) |
|
| 3 |
3 (11%) |
1 (4%) |
|
| Public insurance (vs. private) |
6 (20%) |
6 (25%) |
0.8 |
| Surgery |
| Months from initial visit until surgery, mean ± SD |
9.4 ± 4.5 |
14.5 ± 8.4 |
0 |
| Sleeve (vs. Bypass) Surgery |
17 (57%) |
14 (58%) |
1 |
| No. of overnights, n=1 unknown |
|
|
0.6 |
| 1 |
1 (3%) |
0 (0%) |
|
| 2 |
11 (38%) |
6 (25%) |
|
| 3 |
13 (45%) |
13 (54%) |
|
| 4 |
4 (14%) |
5 (21%) |
|
Table 2: Subject, family, and surgical characteristics by age at the time of surgery (n=54).
Discussion
The pediatric obesity epidemic continues unabated, but disproportionately
affects those least able to access high-quality healthcare.
Within the obesity epidemic overall, the most severe form
of obesity, Class III obesity, defined as BMI>140% of the 95%, has
doubled in prevalence from approximately 1% in 2000 to nearly
2% of the population now. The socioeconomic and racial/ethnic
disparities within the pediatric obesity epidemic are persistent
and the magnitude of these disparities is growing, with obesity
prevalence increasing more rapidly among children that are
Hispanic versus White, and among children from low-income,
low-education households. There has been a recent effort to advance
bariatric surgery as an option for youth with severe obesity,
with the American Academy of Pediatrics recently endorsing the
surgery as safe and effective. However, there is growing recognition
that, if only children with private insurance and higher socioeconomic
status can access bariatric surgery, the surgery may
ultimately exacerbate inequity. It is therefore incumbent upon
centers performing pediatric bariatric surgery to ensure they are
reaching the populations most impacted by severe obesity. In this
study, we report the demographics of our centre’s surgical patients
from 2011-2019, and their weight loss at one year post-surgery
by race, household income, and payer type [1,9,19].
We report that 83% of patients were female, a skewed proportion
relative to the national pool of adolescents and young adults eligible
for bariatric surgery, but mirroring the sex disparities reported
elsewhere in the adolescent and adult literature. One large,
multi-center study found that, among adolescents, severe obesity
was disproportionally enriched in females as compared to males
(61% vs. 39%, respectively) but our population, like those reported
by large national databases of adolescent surgery, reflects
an even larger imbalance by sex in those who undergo surgery versus those who qualify for it. Similarly, in multiple large adult
studies, although men comprise nearly 40% of those eligible for
surgery, they represent only 20% of the population who undergo
surgery. The reasons for this disparity are multifactorial, likely
stemming partially from strong cultural pressures for women and
girls to seek thinness [20-24].
In addition to disparities by sex, racial disparities in bariatric surgery
access have been reported. For example, White adults are
more than 1.5 times as likely to undergo bariatric surgery as patients
from other races. In a large national cohort of pediatric bariatric
patients (to which our center contributes), 60%-70% were
White. Our population was slightly more than half (54%) White,
mirroring these national trends. Of note, more than 40% of the
residents of Boston, the city in which our center is located, are
Black or Hispanic, and the prevalence of obesity among Black and
Hispanic adults in Boston is nearly twice that of White adults. The
drivers of this racial disparity in access to bariatric surgery are
multifactorial, including differing attitudes toward and education
about bariatric surgery by race, decreased likelihood of PCP referral
to surgery of Black and Hispanic patients relative to White
patients, and increased likelihood of racial minorities to be publically
insured relative to White patients. Differential insurance
status by race is important because multiple studies have demonstrated
that patients with private insurance are significantly more
likely to undergo bariatric surgery and have better outcomes than
patients with public insurance. We report that only 12/54 (22%)
of the patients who underwent bariatric surgery at our center
were solely covered by public insurance at time of surgery (Table
1). This proportion is not representative of insurance coverage of
the overall pool of patients who meet clinical criteria for bariatric
surgery, most of whom have public insurance.. Although public
insurance in Massachusetts, where our center is located, covers
bariatric surgery, patients with public insurance often face barriers
including insurance denials which they may be inadequately
resourced to appeal. Additionally, qualifying for bariatric surgery
typically requires six months of supervised medical weight loss
management, including frequent visits which may represent an
untenable burden to patients of lower financial means and prevent
them from sucessfully completing pre-surgery programs
[9,10,13,25-34].
With regards to outcomes, we found no difference in weight loss
trajectory by sex (Table 3), suggesting that weight loss surgery is
equally effective in young females and males and pointing to the
need for increased awareness of and access to this surgery among
male adolescents and young adults. This is in line with the adult
literature on bariatric surtery outcomes, which largely reports no
difference in weight loss by sex [35].
| Covariate |
Difference (95% CI) |
P |
| Sex (ref. female) |
2.5 (-6.0, 10.9) |
0.6 |
| Race (ref. white) |
8.5 (1.4, 15.5) |
0 |
| Age ≥ 18y at surgery (ref. <18y) |
7.0 (0.1, 14.0) |
0.1 |
| Household income* |
- |
0.8 |
| $ 75,000-<$ 100,000 (ref. <$ 75,000) |
-0.5 (-10.2, 9.3) |
|
| ≥ $ 100,000 (ref. <$ 75,000) |
-2.8 (-12.6, 7.0) |
|
| ≥ $ 100,000 (ref.$ 75,000-<$ 100,000)) |
-2.3 (-10.6, 6.0) |
|
| Census tract minority percentage ≥ 40% (ref. <40%) |
8.3 (0.7, 15.8) |
0 |
| Census tract poverty percentage ≥ 10% (ref. <10%) |
-5.9 (-13.1, 1.4) |
0.1 |
| Sleeve surgery (ref. bypass) |
-0.2 (-8.2, 7.7) |
1 |
| Length of stay at surgery |
- |
0.6 |
| 3 days (ref. 2 days) |
3.6 (-3.8, 11.0) |
|
| 4 days (ref. 2 days) |
1.5 (-10.3, 13.3) |
|
| 4 days (ref. 3 days) |
-2.1 (-13.9, 9.6) |
|
| Number of post-op visits |
beta=-0.5 ± 0.6 |
0.4 |
Note: * Household income estimated by Federal Financial Institutions Examination Council (FIFEC) census tract data for patient’s zip code at time of surgery
Table 3: Effect of covariates on change in percentage of 95th percentile for BMI.
We additionally found that POC patients had less weight loss relative
to White patients post-surgery, with no difference by surgery
type. Since the weight loss curves generated by our model
are parallel, the differences in weight loss by race are likely attributable
to POC patients presenting at heavier weights overall,
rather than suggesting some physiologically different response to
bariatric surgery by race. In the adult literature, White patients
have a higher percentage of excess weight loss than do Black or
Hispanic patients with Roux-en-Y gastric bypass, but not with
sleeve gastrectomy, potentially due to bypass being preferentially
performed among patients with increased comorbidities. Cultural
factors may contribute to decreased weight loss among POC patients. These factors including meal sharing within extended families
among Hispanic communities and the valuing of larger body
types in POC populations. Systemic racism, which has resulted in
POC populations living in neighbourhoods that have built environments
that do not promote physical activity and low availability
of healthy foods also likely drives poorer weight loss outcomes
for POC patients. Other potential reasons for this discrepancy in
weight loss by race may be related to the limitations of BMI measurement
(i.e., for a given BMI, White children have greater body
fatness than Black children) or indicative of the need for greater
support and follow-up post-surgery for minority children at our
center [36-40].
Finally, we found no difference in change in BMI over time by either
insurance status (publicly insured vs. privately insured) or
by census tract average annual household income (>$ 75,000 vs.
<$ 75,000) (Figures 2 and 3). This is in keeping with the adult literature,
which suggests that public insurance status itself is not
associated with poor weight loss outcomes, after controlling for
race. The lack of differences in weight loss at one year by these
markers of socioeconomic status suggests that bariatric surgery
is effective, at least in the short-term, for patients regardless of
payer or household income, and highlights the need to engage
publicly insured patients in bariatric surgery centers.
Our study has several strengths and limitations. The strengths
of our study include the granularity of the anthropometric data
over time, permitting a robust model of weight change by various
demographic and socioeconomic markers in a relatively limited
patient population. The standardized follow up in our center
permits comparison of matched weights over time. Many other
studies reporting disparities in obesity outcomes rely on administrative
databases that do not include this level of detail. However,
our study is retrospective and from single center with a relatively
small number of patients, and may thus be underpowered to
detect differential outcomes for certain variables. Given the lack
of patient reported income data, we, like other authors, used
census code zip code as a proxy for income, which may obscure
patient level variability within zip codes? Finally, our primary outcome
of weight loss at one year is short-term and may not reflect
long term results. The one year cut off was necessary to ensure
a robust data set, given significant attrition to long-term follow
up, a common challenge of working with young adults undergoing
bariatric surgery. However, recent data suggests that shortterm
weight loss outcomes are useful predictors of long-term
success, as the majority of weight loss among adolescents and
young adults undergoing bariatric surgery takes place within the
first year after surgery and short-term metrics such as greater %
excess weight loss at three months can predict the long-term durability
of weight loss.
Conclusion
In conclusion, we report that our centers demographic data
echoes that of a nationally representative sample of adults
demonstrating that the majority of bariatric surgeries are performed
in White, privately insured patients, although those eligible
for bariatric surgery have lower family incomes, lower education
levels, and greater proportion of POC race than those not
eligible for surgery. Our results point to several potential areas
for quality improvement and further research. Most notably, our
center and other bariatric centers like it must strive to understand the referral patterns and patient access issues that drive
the population of surgical patients to differ significantly from the
overall population of eligible patients with severe obesity. Many
paediatricians remain reticent to refer adolescents for bariatric
surgery regardless of race or socioeconomic status. The adult
literature demonstrates, however, that patients who have been
recommended bariatric surgery by their physicians are nearly five
times as likely to undergo surgery than those whose physicians do
not recommend it, and that men and patients who are Black are
less likely to be referred for surgery than are women and patients
who are White. Similarly, one study found that 85% of parents
counselled by their paediatrician about bariatric surgery would
consider it for their child, compared to only 35% of parents who
did not receive counselling. It is clear, therefore, that education
of primary care providers will be a key tool to ensure that all patients,
including/especially those who are POC, male, and/or publicly
insured have equal access to bariatric surgery. Additionally,
insurance reform must provide coverage for bariatric surgery in
medically qualified patients.
Our institution, like many other pediatric academic hospitals nationwide,
recently announced the establishment of an institute
for health equity. Given the clear benefits of bariatric surgery for
severe obesity, the disproportionate burden of severe obesity on
already marginalized populations, and the multifactorial nature of
barriers to accessing bariatric surgery, the field of Pediatrics has
a profound opportunity to advance health justice by diversifying
the population of patients who have access to this life-saving intervention.
Author Contributions
• Erin Mauney made substantial contributions to the analysis
and interpretation of data for the work, drafted the work,
gives final approval of the version to be published, and agrees
to be accountable for all aspects of the work in ensuring that
questions related to the accuracy or integrity of any part of
the work are appropriately investigated and resolved
• Paul Mitchell made substantial contributions to the analysis
and interpretation of data for the work, drafted the work,
gives final approval of the version to be published, and agrees
to be accountable for all aspects of the work in ensuring that
questions related to the accuracy or integrity of any part of
the work are appropriately investigated and resolved
• Camilla Richmond made substantial contributions to the
analysis and interpretation of data for the work, drafted the
work, gives final approval of the version to be published, and
agrees to be accountable for all aspects of the work in ensuring
that questions related to the accuracy or integrity of any
part of the work are appropriately investigated and resolved
• Brian Carmine made substantial contributions to interpretation
of data for the work, gives final approval of the version
to be published, and agrees to be accountable for all aspects
of the work in ensuring that questions related to the accuracy
or integrity of any part of the work are appropriately
investigated and resolved
• Annemari Fayemi made substantial contributions to interpretation
of data for the work, gives final approval of the version
to be published, and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy
or integrity of any part of the work are appropriately
investigated and resolved
• Nirav Desai made substantial contributions to the analysis
and interpretation of data for the work, drafted the work,
gives final approval of the version to be published, and agrees
to be accountable for all aspects of the work in ensuring that
questions related to the accuracy or integrity of any part of
the work are appropriately investigated and resolved.
Conflict of Interest
The authors declare they have no conflicts of interest.
References
- Skinner AC, Skelton JA (2014) Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA pediat 168(6): 561–6.
[Crossref] [Google Scholar]
- Freedman DS, Mei Z, Srinivasan SR (2007) Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The bogalusa heart study. J pediat 150(1): 12–7.
[Crossref] [Google Scholar]
- Knop C, Singer V, Uysal Y (2015) Extremely obese children respond better than extremely obese adolescents to lifestyle interventions. Pediat obes 10(1): 7–14.
[Crossref] [Google Scholar]
- Inge TH, Courcoulas AP, Jenkins TM (2016) Weight loss and health status 3 years after bariatric surgery in adolescents. New England J Med 374(2): 113–23.
[Google Scholar]
- Kyler KE, Bettenhausen JL, Hall M (2019) Trends in volume and utilization outcomes in adolescent metabolic and bariatric surgery at children’s hospitals. J Adoles Healt 65(3): 331–6.
[Crossref] [Google Scholar]
- Campos GM, Khoraki J, Browning MG (2020) Changes in utilization of bariatric surgery in the united states from 1993 to 2016. Annals of Surg 271(2).
[Crossref] [Google Scholar]
- Inge TH, Zeller MH, Jenkins TM (2014) Perioperative outcomes of adolescents undergoing bariatric surgery: The Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study. JAMA pediat 168(1): 47–53.
[Crossref] [Google Scholar]
- Tsai WS, Inge TH, Burd RS (2007) Bariatric surgery in adolescents: Recent national trends in use and in-hospital outcome. Arch Pediat & Adoles Med 161(3): 217–21.
[Crossref] [Google Scholar]
- Armstrong SC, Bolling CF, Michalsky MP (2019) Pediatric metabolic and bariatric surgery: Evidence, barriers, and best practices. Pediat 144(6): e20193223.
[Crossref] [Google Scholar]
- Hennings DL, Baimas-George M, Al-Quarayshi Z (2018) The inequity of bariatric surgery: Publicly insured patients undergo lower rates of bariatric surgery with worse outcomes. Obes surg 28(1): 44–51.
[Crossref] [Google Scholar]
- Bethell C, Read D, Goodman E (2009) Consistently inconsistent: A snapshot of across-and within-state disparities in the prevalence of childhood overweight and obesity. Pediat 123: S277–86.
[Crossref] [Google Scholar]
- Lee JS, Sheer JLO, Lopez N (2010) Coverage of obesity treatment: A state-by-state analysis of medicaid and state insurance laws. Pub healt rep 125(4): 596–604.
[Google Scholar]
- Inge TH, Boyce TW, Lee M (2014) Access to care for adolescents seeking weight loss surgery. Obes 22(12): 2593–7.
[Crossref] [Google Scholar]
- Nunez Lopez O, Jupiter DC, Bohanon FJ (2017) Health disparities in adolescent bariatric surgery: Nationwide outcomes and utilization. J Adoles Healt 61(5): 649–56.
[Crossref] [Google Scholar]
- Perez NP, Westfal ML, Stapleton SM (2020) Beyond insurance: Race-based disparities in the use of metabolic and bariatric surgery for the management of severe pediatric obesity. Surg Obes Related Dis 16(3): 414–9.
[Crossref] [Google Scholar]
- Johnson-Mann C, Martin AN, Williams MD (2019) Investigating racial disparities in bariatric surgery referrals. Surg Obes Related Dis 15(4): 615–20.
[Crossref] [Google Scholar]
- Wood MH, Carlin AM, Ghaferi AA (2019) Association of race with bariatric surgery outcomes. JAMA surg 154(5): e190029–e190029.
[Crossref] [Google Scholar]
- Singh GK, Siahpush M, Kogan MD (2010) Rising social inequalities in US childhood obesity, 2003–2007. Annals Epidem 20(1): 40–52.
[Crossref] [Google Scholar]
- Campoverde Reyes KJ, Misra M, Lee H (2018) Weight loss surgery utilization in patients aged 14-25 with severe obesity among several healthcare institutions in the United States. Front in Pediat 6: 251.
[Crossref] [Google Scholar]
- Fuchs HF, Broderick RC, Harnsberger CR (2015) Benefits of bariatric surgery do not reach obese men. J Laparoendoscopic & Advan Surgi Tech 25(3): 196–201.
[Crossref] [Google Scholar]
- Aly S, Hachey K, Pernar LIM (2020) Gender disparities in weight loss surgery. Mini-invasive Surg 4.
[Google Scholar]
- Hecht LM, Pester B, Braciszewski JM (2020) Socioeconomic and racial disparities in bariatric surgery. Obes surg 1–5.
[Crossref] [Google Scholar]
- Steinberger AE, Youngwirth LM, Kim SE (2021) Adolescent bariatric surgery: Racial disparities in 30-day outcomes using the mbsaqip from 2015 to 2018. Obes Surg
[Crossref] [Google Scholar]
- Griggs CL, Perez NP, Goldstone RN (2018) National trends in the use of metabolic and bariatric surgery among pediatric patients with severe obesity. JAMA pediat 172(12): 1191–2.
[Crossref] [Google Scholar]
- Woolford SJ, Clark SJ, Gebremariam A, Davis MM (2010) To cut or not to cut: Physicians’ perspectives on referring adolescents for bariatric surgery. Obes Surg 20(7): 937–42.
[Crossref] [Google Scholar]
- Massachusetts Department of Public Health (2021) Massachusetts obesity statistics.
[Google Scholar]
- Lynch CS, Chang JC, Ford AF (2007) Obese african-american women’s perspectives on weight loss and bariatric surgery. J Gen Internal Med 22(7): 908–14.
[Crossref] [Google Scholar]
- Corral I, Landrine H (2019) Racial differences in the predictors of interest in bariatric surgery in the rural, southeastern USA. J Racial Ethn Healt Dispar 6(3): 481–6.
[Crossref] [Google Scholar]
- Wee CC, Huskey KW, Bolcic-Jankovic D (2014) Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J gen inter med 29(1): 68–75.
[Crossref] [Google Scholar]
- Cohen RA, Martinez ME, Zammitti EP (2016) Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2015. Nat Healt Interview Surv.
[Google Scholar]
- Martin M, Beekley A, Kjorstad R (2010) Socioeconomic disparities in eligibility and access to bariatric surgery: A national population-based analysis. Surg Obes Rel Dis 6(1): 8–15.
[Crossref] [Google Scholar]
- Ortega E, Morínigo R, Flores L (2012) Predictive factors of excess body weight loss 1 year after laparoscopic bariatric surgery. Surg Endos 26(6): 1744–50.
[Crossref] [Google Scholar]
- Coleman KJ, Huang YC, Hendee F (2014) Three-year weight outcomes from a bariatric surgery registry in a large integrated healthcare system. Surg Obes Rel Dis 10(3): 396–403.
[Crossref] [Google Scholar]
- Daniels SR, Khoury PR, Morrison JA (1997) The utility of body mass index as a measure of body fatness in children and adolescents: Differences by race and gender. Pediat 99(6): 804 LP - 807.
[Crossref] [Google Scholar]
- Capodilupo CM, Kim S (2014). Gender and race matter: The importance of considering intersections in Black women’s body image. J Counsel Psych 61(1): 37.
[Crossref] [Google Scholar]
- Boone-Heinonen J, Diez-Roux A V, Goff DC (2013) The neighborhood energy balance equation: Does neighborhood food retail environment+physical activity environment obesity? The cardia study. PloS one 8(12): e85141.
[Crossref] [Google Scholar]
- Melton GB, Steele KE, Schweitzer MA (2008) Suboptimal weight loss after gastric bypass surgery: Correlation of demographics, comorbidities, and insurance status with outcomes. J Gastrointes Surg 12(2): 250–5.
[Crossref] [Google Scholar]
- Dreber H, Thorell A, Torgerson J (2018) Weight loss, adverse events, and loss to follow-up after gastric bypass in young versus older adults: A scandinavian obesity surgery registry study. Surg Obes Rel Dis 14(9): 1319–26.
[Crossref] [Google Scholar]
- Chu L, Howell B, Steinberg A (2019) Early weight loss in adolescents following bariatric surgery predicts weight loss at 12 and 24 months. Pediat Obes 14(8): e12519.
[Crossref] [Google Scholar]
- Singh UD, Chernoguz A (2020) Parental attitudes toward bariatric surgery in adolescents with obesity. Surg Obes Rel Dis 16(3): 406–13
[Crossref] [Google Scholar]
Citation: Erin M, Desai Nirav K, Paul M, Brian C, Annemari F, et al. (2023) Impact of Socioeconomic Status on Adolescent Bariatric
Surgery Outcomes in a Quaternary Pediatric Hospital. J Child Obesity. 8:006.
Copyright: © 2023 Erin M. This is an open-access article distributed under the terms of the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source
are credited.