Key words
audio recording, black and ethnic minority
groups, concordance, cultural competence,
information recall, patient information, primary care
Introduction
It has been known for some time that a significant
percentage of the information given in medical consultations
is forgotten (Goodwin, 2000). To give some
early examples, Anderson et al (1979) showed that
patients only remembered 40% of the information
they were given, and that almost half of what they
recalled was incorrect and had either been imagined or
misconstrued. More recently, McGuire (1996) found
that patients remembered only 25% of the information
they were given, which is less than that reported
by many previous studies into recall (e.g. Anderson
et al, 1979; Rice et al, 1989; Shapiro et al, 1992). This
situation may be due to the fact that medical advice
is usually spoken. Blinder et al (2001) showed that
written information was better remembered and was
associated with greater compliance with the advice given. Written information, however, is not necessarily
appropriate for people with low literacy or for
non-English speakers. The challenge, in such situations,
is to find a medium in which information can be
presented and retained for future reference.
The use of tape recordings has been explored in
secondary care, mostly in oncology settings (McClement
and Hack, 1999; Tattersall et al, 2002). Scott et al
(2003) carried out a systematic review of the literature
and concluded that the provision of audio recordings
or summaries of important consultations could benefit
most adults with cancer. Other specialties in secondary
care have also undertaken trials on the use
of audio tapes. For example, Leahy et al (2005) gave
audio tapes of consultations to preoperative cardiac
surgery patients, and found that patients who received a tape found it of positive value in addressing their
information concerns. Listening to the tape increased
patients’ understanding and their ability to give informed
consent.
Despite these successes, there seem to have been
fewer attempts in primary care to explore the use of
audio recordings in providing information for patients.
This paper describes a project which piloted the
application of a new audio technology to information
giving in primary care, through the use of digital
recording devices (DRDs) to record personalised information
for patients from the Somali population.
Overview of the project
The aim
People who speak English are able to benefit from a
range of information sources mostly barred to those
who cannot read either in their mother tongue or in
English. Therefore, we set out to look at the benefits
experienced by patients in primary care, who could
not communicate in English, of receiving audio information,
in their own language, on a DRD, and to
establish whether the equipment used was suitable for
purpose. At this stage we felt that this was as far as
we could go, although we recognise that it would
ultimately be useful to also establish the effectiveness
of the devices by, for example, testing recall of information.
The equipment
The DRDs used were small (80 � 57 � 10 mm),
inexpensive devices with a unit cost of £4.50 that
allowed up to one minute of audio information to
be recorded. A microphone built into the back of the
device enabled information to be recorded, and a large
button on the front allowed information to be
replayed. The devices were issued with batteries
already inserted and ready to use. No set-up time
was needed. The message time was limited to one
minute, so recording the message had minimal impact
on the overall consultation time. The audio message
on the DRD could also be changed by recording over
any existing audio information, allowing the devices
to be re-used.
The setting and sample
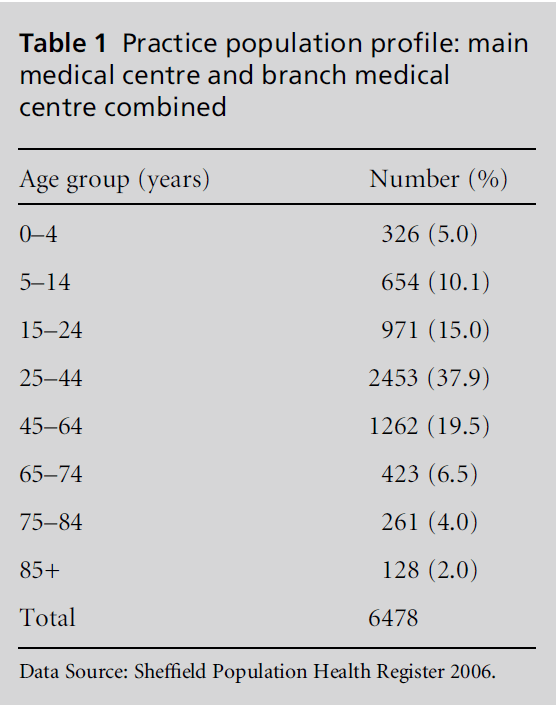
The project was based at a branch of an inner-city
medical centre in Sheffield where Somali people account
for 23.6% of the practice population of 2780
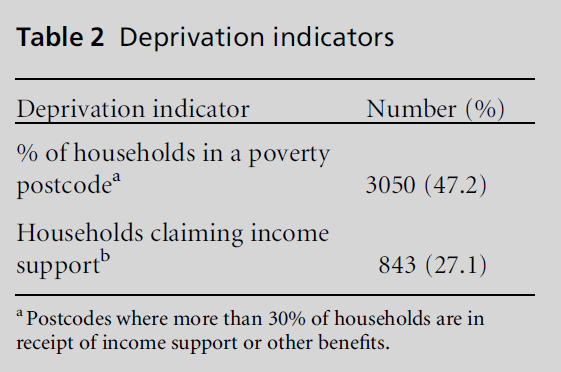
(see Table 1). In terms of deprivation, 27.1% of the
households registered with the main and branch surgery claim income support (see Table 2). The
practice has patients on its books from many different
countries. The Somali population was selected for this
pilot project as Somali patients are frequent users of
the services offered at the practice. As a group, Somali
refugees experience many health and social welfare
problems. There is high unemployment and poverty
amongst the Somali population generally, with some
studies estimating over 70% unemployment among
Somali men (Rutter, 2006). Between 20% and 70%
of all Somali families in the UK have female heads of
household. This is attributed to civil war, families
being split up when fleeing the country, or divorce
(Rutter, 2006). The refugee experience of many of the
people who have recently arrived from Somalia means
that they suffer from depression, anxiety, posttraumatic
stress disorder and problems of adjustment
related to the change in culture (CVS Consultants and
Migrant and Refugee Communities Forum, 1999).
Many have had little or no education in their home country because of the civil war. They have a limited
knowledge of English, and many adults are not literate
in any language (Rutter, 2006). Audio information
therefore seemed an appropriate tool to pilot in this
community.
Table 1: Practice population profile: main
medical centre and branch medical
centre combined.
Table 2: Deprivation indicators.
All Somali patients over the age of 18 years who
needed an interpreter to accompany them in their
appointment with a health professional were invited
to take part in the study, and receive a personalised
digital recording of information about their health to
take home with them at the end of the consultation.
Patientswere approached by the Somali link worker in
the waiting room, and the study was explained to them
in their own language. Patients who agreed to take part
were asked to sign a consent form. The link worker
explained the content of the consent form to patients
who either signed their name or marked the form with
a cross to signify their consent to receiving an audio
recording device and being contacted at home by
phone a week to 10 days later.
All patients who were approached were given the
option of not taking part and of withdrawing from the
project at any time. North Sheffield Research Ethics
Committee reviewed the project and issued a favourable
opinion.
The link worker
A Somali link worker is employed by the practice, and
this simplified any issues around interpreting. The
link worker was involved in the project from the
beginning and so was well informed and able to give
patients information about the project and ask for
their consent. It would have been more difficult to do
this if we had needed to use a series of different
interpreters from an agency.
The link worker at the practice routinely interpreted
for patients who requested help in GP consultations.
For this project the link worker was asked to
record the summary information given by the general
practitioner (GP) at the end of the consultation onto
the DRD, and to give the patient the recording device
to take home. In most cases, rather than give a
summary of the advice given, the GP asked the link
worker to record information about medication, or
future appointments onto the DRD. All the patients in
this study had a previous history of being accompanied
in the surgery by a link worker who gave an
interpretation of the GP’s verbal summary at the end
of the consultation. This study simply extended that
normal practice, by the interpreter recording their
interpretation of the GP’s verbal information onto the
recording device. A few devices were given out by the
physiotherapist in the practice and these contained
information about how to do specific exercises.
Method and data analysis
A semi-structured questionnaire was drawn up in
consultation with researchers from the University of
Sheffield School of Nursing. This was administered in
a telephone interview undertaken by one of the three
Somali interpreters recruited to the project from the
Community Access and Interpreting Service. Training
was arranged for all the interpreters through the
School of Nursing at the University of Sheffield.
The questionnaire consisted of 13 questions. Of
these, eight were factual questions and five open
questions. The questionnaire was piloted during the
interviewer training to iron out any problems before
the project started. Questions were asked about frequency
of use of the DRD, and whether people other
than the patient had listened. Three factual questions
were included about the equipment’s suitability for
purpose, in terms of ease of use, the clarity of the audio
information and any problems in operating the DRD.
An open question was asked about how people felt
about receiving personalised information to take
home on a DRD, and the interviewer used a series of
written prompts to attempt to draw out more indepth
answers to this question. Two questions were
asked about the type of information recorded, how
useful this had been and what patients would like to be
recorded in the future. Finally, therewas a question for
those who had not used the DRD, asking them to give
reasons for non-use.
Data from the questionnaire were entered onto an
Excel spreadsheet. The number of people and the
amount of data enabled the qualitative analysis to be
performed manually by looking for common themes
in the interpreter’s notes.
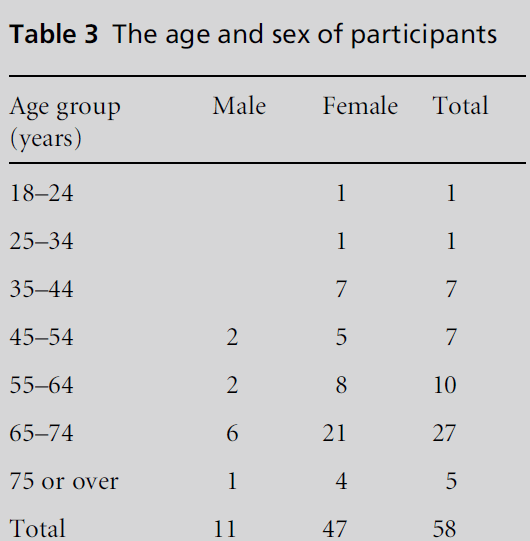
Table 3: The age and sex of participants.
The intention behind the qualitative questions was
to uncover the interviewees’ own interpretations of
the value of the devices. While the prompts reflected
the researchers’ prior assumptions about how the
devices might be useful for the participant, they
nevertheless encouraged the interpreter to explore
all possibilities. This approach recognised that rather
than having an objective meaning, the value of the
devices came from how they were used by the patient
to interact with their particular circumstances of
having limited fluency in the English language. Following
a symbolic interactionist perspective, the data
analysis sought to discover the socially constructed
meanings that the devices had for people’s own lives,
in relation to their GP consultation. This meaning
arose not from the intrinsic value of the devices
themselves, but from how it became created through
the patients’ interaction with understanding their
health. The coding structure focused on examining
the meaningful and symbolic interpretation that the
devices had for the patients themselves.
Administration of the questionnaire
Interviewers wrote down the answers given by the
participants while they were on the phone, with a
questionnaire taking approximately 10 minutes to
complete. Tick box answers were included for some
of the simple factual questions. The interviewers were
not part of the research team and had no stake in the
outcome. They were gender matched with the patients
they were contacting. In some cases the subject did
know the interpreter who administered the questions.
This was important because in a close-knit community,
people do know each other, and it is difficult to be
completely anonymous.
The interviewers initially experienced some problems
in successfully making contact with participants.
Some people could not remember their phone number
accurately and others were living in hostels where
there was only a communal phone. Most of these
problems were solved by the practice checking the
telephone numbers before the consent forms were
passed on to the research team.
Findings
In total 68 people agreed to take part in the project and
received a DRD. Contact was made with 58 of the
participants who were given the opportunity to opt
out of the project before the interviewers began the
questionnaire. No one chose to drop out at this stage.
Of the 58 people who completed a questionnaire, 81%
were women, mainly aged over 55 years (see Table 3).
It was not possible to follow up ten of the people
who had been given a DRD. We do not know whether
they chose not to answer the phone as they did not want to talk to an interviewer, or whether they were
simply unavailable.
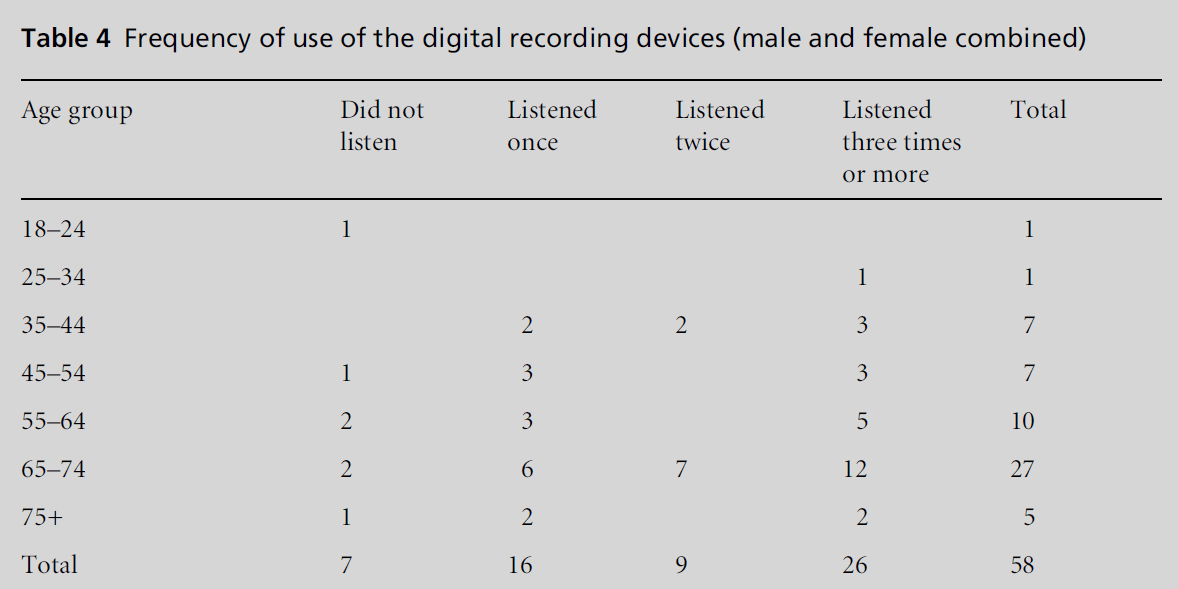
Table 4: Frequency of use of the digital recording devices (male and female combined).
People were at first reluctant to accept a DRD and
take part in the project. The link worker reported that
people liked the idea of being able to take personalised
audio information away with them, but were not sure
about being phoned at home afterwards and asked for
their views in case it had something to do with social
services. They were reassured by the fact that one of the
interviewers who had been trained to carry out the
questionnaire was well known in the community, that
they were given the opportunity to opt out of the
project and didn’t have to answer the questions if they
didn’t want to. After the project had been going a few
weeks, people began to come to the surgery and ask for
a recording device. Word of mouth spread news about
the project through the community, and people decided
they would like to take part.
Did patients listen to the information?
Fifty-one of the 58 interviewees had listened to the
information on the DRD (see Table 4). Of these, 16
people had listened once, nine had listened twice and
26 had listened more than three times, some of them
reporting that they had listened ‘many, many times’,
or ‘several times a day’. The questionnaire showed that
most people had just listened to the information
themselves.However, some people (39%) had allowed
family members to listen to the information as well.
Seven people had not listened to the recording.
Four said they were too busy, hospital visiting or
looking after young children. One could not remember
being given a device, one person’s recorderwas not
working and one person felt that they didn’t need the
recording as they had a good memory. Frequent
listeners tended to be in the older age groups. However
some younger people were also in the group who said
they had listened many times. These were people who,
although they were young, reported having memory
problems, or the information recorded for them was
of a nature that could be listened to many times, for
example, instructions for doing exercises.
Was the audio information useful?
Of the 51 people who had listened to the audio
information, 48 (94%) reported that they thought
the recorded information was useful. Two people said
they would have liked different information to be
recorded. One person felt they had a good memory
and didn’t need information recording and so had not
listened to the message.
Those unable to read English found the devices
especially useful in enabling them to remember
advice given and to overcome problems with written information. For example, many patients mentioned
that they used to forget how to take their prescribed
medication, but the DRD helped them to take it
correctly.
‘I use to forget the way I am taking the medication but
since I got the device I amnot.’ (woman aged 65–74 years)
‘I listen whenever I want to take my medication to make
sure that I am taking the right amount or in the right
time.’ (woman aged 65–74 years)
‘I don’t read or write English so remembering or listening
from the device is a good thing.’ (woman aged 55–64
years)
‘As I cannot read the label of medicine, but listening [to]
the device about the audio information recorded was just
telling me how to take my prescription.’ (man aged 55–64
years)
Patients also said that it helped them to remember
appointments that they would otherwise have forgotten.
For instance:
‘I am elderly woman, I always forget appointment, but
now the device helps me.’ (woman aged 65–74 years)
Older people and those with memory problems felt
that the DRD was useful, as they were aware that they
forgot many things:
‘I have got hard time remembering things so to have it
recorded helps me.’ (woman aged 65–74 years)
Was the equipment suitable?
Most patients (98%) found the DRDs robust and easy
to use and had no problems using them. The DRDs were delivered with the batteries already inserted for
immediate use and a spare set enclosed. In a proportion
of the devices the batteries were not working
and needed to be replaced, but this appeared to be the
only problem reported and was simple to remedy.
Only one person could not get the device to work.
Comments were made about the fact that the
devices were small enough to be carried around
anywhere and that they were perceived as being useful.
‘I think this is a fantastic piece of tool and I think many
people will benefit from it.’ (man aged 45–54 years)
The questionnaire asked people what the DRD had
helped them remember. Most responses related to
remembering appointment times or how to take
medication. People were also asked what sort of
information they would like to be recorded next time.
People could clearly see the benefit of the information
that had been recorded for them, but were also able to
extrapolate how the DRDs could be used and the sort
of information that they might find useful in the
future. Nineteen people came up with a broad range
of ideas other than medication or appointments that
they would like to be recorded, for example: information
about healthy diets, the side-effects of medication,
and health correspondence.
People can have high expectations of technology.
The link worker reported that initially some people
expected that at the right time the DRD would be
activated to remind them of whatever they needed to
do, to take medication or go for their appointment.
This facility is beyond the scope of the DRD that was
piloted and would be a much more expensive and
complex device to set up.
Discussion
When assessed against the aims of the study, the above
findings indicate that the majority of patients perceived
clear benefits in their use of the DRDs. This
strong support for the DRDs needs to be considered
against a number of contextual factors.
Methodology
Given that an inclusion criterion for recruitment was
that the patient routinely needed an interpreter to
accompany them into the GP consultation, it was
always likely that the sample would be skewed towards
older people for two reasons. Firstly, older people are
more likely to have health problems and secondly,
they are less likely to be fluent in English and therefore
more likely to need an interpreter.As noted earlier, the
Somali community has a greater preponderance of
female heads of household. This, together with the
working pattern of the link worker, who covered only
morning sessions, could account for the skewed nature
of the sample. We do not know whether we would
have obtained different results if more men and
younger people had been interviewed.
The nature of the qualitative data collected may
have been limited by the use of interpreters as interviewers.
Despite receiving training in basic interviewing
skills at the start of the study, the interpreters could
not be expected to follow a qualitative paradigm to
probe for participants’ views in the same way that an
experienced researcher would. This may have limited
the richness of the data collected and inevitably made
the researchers’ analysis dependent on those aspects of
the interview that the interpreter chose to focus on,
and to make notes of.
Evaluating the perceived benefits of aDRDamongst
a community of people, many of whom are vulnerable,
presents many challenges. Comments from the
link worker highlighted how people are likely to be
suspicious and reluctant to take part in anything
where they need to be followed up and contacted at
home.
Factors affecting acceptance of the
DRDs by patients
While this study investigated the acceptance of the
DRDs it did not control for the content of information
recorded. The nature of the information would clearly
be expected to influence the patients’ perceived benefits
of the devices. The fact that people were able to
extrapolate how the DRDs could be used in the future
and the sort of information that they might find useful
suggests that the participants felt the DRDs had value. Also, the fact that people took the initiative to ask for
a DRD when they came to the surgery appears to
indicate that the devices had value to members of the
Somali community.
However, the findings also showed that a minority
of participants had not listened to the information
(see Table 4). This acts as a reminder that the DRDs
may not be appropriate in every situation, and there
may need to be some discretion in distributing devices,
based on who would benefit. Other studies into the use
of audio tapes such as one by Leahy et al (2005) found
that some people preferred not to listen to the audio
information they were given and that this may have
had something to do with their preferred coping
mechanism.
The devices were piloted in a practice where staff
were interested in new ideas that could potentially
benefit their patients, and co-operated fully with the
study. The use of the DRDs elsewhere would be
dependent on the willingness of staff to participate.
Future application
The findings have highlighted the perceived benefits of
the DRDs among the Somali population, especially
among older members of the community who are less
likely to speak English. We would suggest that these
benefits may also apply to other non-English-speaking
populations, including the recent influx of new populations
from the EU. TheDRDs could have several uses
in the health sector, to inform, to educate or to jog
people’s memories, and could find applications in
prescribing, or giving lifestyle advice, as well as contributing
to concordance with advice given during a
consultation.
While the DRD’s maximum recording time of one
minute proved to be adequate in the context of
summarising the consultation, different applications
may have different recording time requirements. One
GP at the practice wanted to give out more than one
DRD to each patient to allow longer messages to be
recorded. The cost of the DRD increases with the
length of the recording time. A longer recording time
may put the device out of reach of many budgets. One
minute certainly gives more flexibility than most
inexpensive DRDs on the market at present, which
allow only 10–20 seconds to be recorded. However,
technology is moving fast and it is quite likely that in
the future low-cost devices will be available with a
longer recording time that would give greater flexibility.
The DRDs can be re-used, as each time a newmessage
is recorded it wipes out the old message. Their re-use is
dependent on patients returning with them at their
next appointment. There could be a danger in giving
patients more than one device as messages could get out of date or mixed up. Some formof labelling on the
outside of the device may help overcome this problem.
Conclusion
This project looked at the benefits patients perceived
of being given personalised audio information to take
home with them. The results seem to indicate that for
older people from this practice population, and for
those with memory problems, the recordings were
useful to patients.
The DRDs were reliable, used frequently and found
to be acceptable. They were used to record information
about appointments and medication, and patients
identified other types of information they would find
useful. It is also possible to see that DRDs would be
equally useful in a health setting for any ethnicminority
population who had problems with written or spoken
English.
The feedback received from participants implies
that a small investment in DRDs could have an impact
on attendance rates and compliance with prescribed
medication. This in turn could contribute to reducing
any waste of NHS resources. A more extensive study
would need to be carried out to verify this, and the cost
of theDRDs would need to be considered against these
additional patient benefits.
Acknowledgment
We are grateful to the staff at Hanover Medical Centre
in Sheffield for all their help in undertaking this
project
FUNDING BODY
This research was funded by the Dorothy Dixon
Barrow Award in Sheffield.
COMPETING INTERESTS
None.
References
- Anderson JL, Dodman S, Kopelman M and Fleming A(1979) Patient information recall in a rheumatologyclinic. Rheumatology and Rehabilitation 18:18–22.
- Blinder D, Rotenberg L, Peleg M and Taicher S (2001)Patient compliance to instructions after oral surgicalprocedures. International Journal of Oral and MaxillofacialSurgery 30:216–19.
- CVS Consultants and Migrant and Refugee CommunitiesForum (1999) A Shattered World, the Mental Health Needsof Refugees and Newly Arrived Communities. London: CVSConsultants.Godwin Y (2000) Do they listen? A review of informationretained by patients following consent for reductionmammoplasty. British Journal of Plastic Surgery 53:121–5.
- Leahy M, Douglass J, Barley V, Jarman M and Cooper G(2005) Audiotaping the heart surgery consultation: qualitativestudy of patients’ experiences. Heart 91:1469–70.
- McClement SE and Hack TF (1999) Audio-taping theoncology treatment consultation: a literature review. PatientEducation and Counselling 36:229–38.
- McGuire LC (1996) Remembering what the doctor said:organization and adults’ memory for medical information.Experimental Aging Research 22:403–28.
- Rice GE,Meyer BJF andMillerDC (1989)Using text structureto improve older adults’ recall of important medicalinformation. Educational Gerontology 15:527–42.
- Rutter J (2006) Refugee Children in the UK. Buckingham:Open University Press.Tattersall MH and Butow PN (2002) Consultation audiotapes: an underused cancer patient information aid andclinical research tool. Lancet Oncology 3:431–7.
- Scott J-T, Harmsen M, Prictor MJ et al (2003) Recordings orsummaries of consultations for people with cancer(Cochrane Review). The Cochrane Library, Issue 2. Oxford:Update Software.
- Shapiro DE, Boggs SR, Melamed BG and Graham-Pole J(1992) The effect of varied physician affect on recall,anxiety, and perceptions in women at risk for breast cancer: an analogue study. Health Psychology 11:61–6.