Key words
health services, qualitative research,
review, sexuality
Background
People’s experiences of healthcare may affect whether
they decide to seek medical advice, their relationships
with healthcare professionals and, ultimately, may have
an important impact on their treatment and health
status. These healthcare experiences are likely to vary
within the population according to gender, age, ethnicity
and, as investigated in the current review, sexual
orientation.
Although approximately6%of people in theUKare
thought to be lesbian, gay or bisexual (LGB; Department
of Trade and Industry, 2004), little research has
investigated the health status of this group. The
majority of published research relates to HIV, AIDS
and sexually transmitted diseases, and very few studies
have examined general LGB health.
A systematic review has indicated that there are
increased rates of mental disorders, suicide and selfharm
in LGB people (King et al, 2008), and a recent
report on UK-specific LGB healthcare (Meads et al,
2009) showed increased rates of smoking, illicit drug
use and mental health problems such as depression,
eating disorders, self-harming and attempted suicide.
Approximately 50% of LGB patients had revealed
their sexual orientation to their GP. LGB patients’
experiences of health services were generally poor.
Most GP surgeries were not overtly LGB-friendly,
mental health counselling was rated as unsatisfactory,
and some GPs showed negative attitudes towards LGB
patients. However, the reasons for poor experiences
of healthcare among LGB patients were not entirely
clear, and there is a need for further investigation. This
paper examines experiences of healthcare provision
for LGB patients in the UK from the perspective of
both patient and practitioner by undertaking a systematic
review of the qualitative literature. This review
may also be applicable to healthcare settings in other
countries, where there may be instances of similar
relational and institutional barriers.
Methods
Sources
Medline, Medline In-Process, EMBASE, CENTRAL,
PsycINFO, Web of Science (SCI and SSCI) and
Cochrane Library databases were searched for reviews
and primary studies of healthcare provision to LGB
patients published between January 2000 and May
2008. A broad search strategy was used, including
terms related to homosexual, lesbian, gay and bisexual
people, restricted only by publication date and English
language. This search identified both quantitative and qualitative research, and specific qualitative material
related to LGB healthcare was identified subsequently
during title/abstract screening. An Internet search was
conducted using Google, together with additional targeted
searches of selected relevant websites. Citations
from systematic and narrative reviews were checked
for relevant studies.
Study selection
The criteria for study selection were that the research
participants were LGB patients or their practitioners
in the UK, that the studies had been conducted since
January 2000, and that theydescribed experiences related
to an aspect of healthcare. Studies could investigate
any intervention with any comparator group (or no
comparison), but only those with qualitative material
were included. Primary studies that were related to
sexually transmitted diseases, safe sex and sexual behaviour
were excluded.
All identified citations were initially screened by
two reviewers (CM and MP) for inclusion according
to the inclusion criteria. Any disagreements were
resolved through discussion. Full texts were retrieved
for potentially relevant articles, and were processed by
one reviewer. These were checked by a second reviewer
and any disagreements were resolved through discussion.
Data extraction and thematic
synthesis
Qualitative information on experiences of LGB
healthcare from the point of view of patients and
professionals was extracted. Synthesis was undertaken
using an approach similar tometa-ethnography (Britten
et al, 2002), but involving both first-order concepts
(expressions of participants) and second-order concepts
(interpretations or explanations by researchers)
in thematic analysis.Concepts were identified by reading
and re-reading the included papers, and these were
grouped into themes for narrative discussion. Synthesis
was undertaken by a researcher who had no
particular theoretical approach to qualitative research
or LGB healthcare. Data extraction and thematic
synthesis were undertaken by one reviewer. Another
reviewer read papers and checked the findings for
consistency.
Quality assessment
A quality checklist (Wallace et al, 2004) was recommended
by an expert in qualitative research. This tool
highlighted areas of potential bias related to the
theoretical perspective of the study investigators, study
design,methods of participant sampling, data collection, suitability of data analysis, the extent to which reported
data reflected those collected, and the extent to which
the study could be generalised to all LGB individuals.
Quality assessment of the included studies was undertaken
by one reviewer.
Results
Identified studies
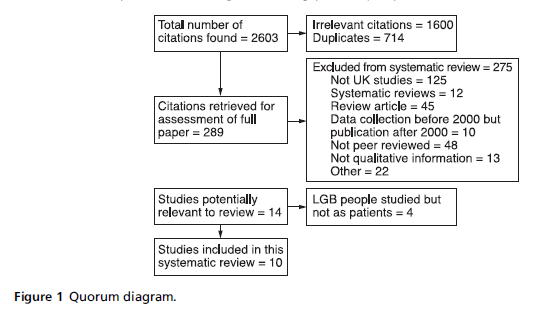
From the searches, a total of 2603 citations were
identified, of which 714 were duplicates. Of the remaining
1889 citations, 233 papers and reports were retrieved
for assessment (see Figure 1). Ten peer-reviewed, published,
qualitative studies were included in the final
systematic review (see Table 1).
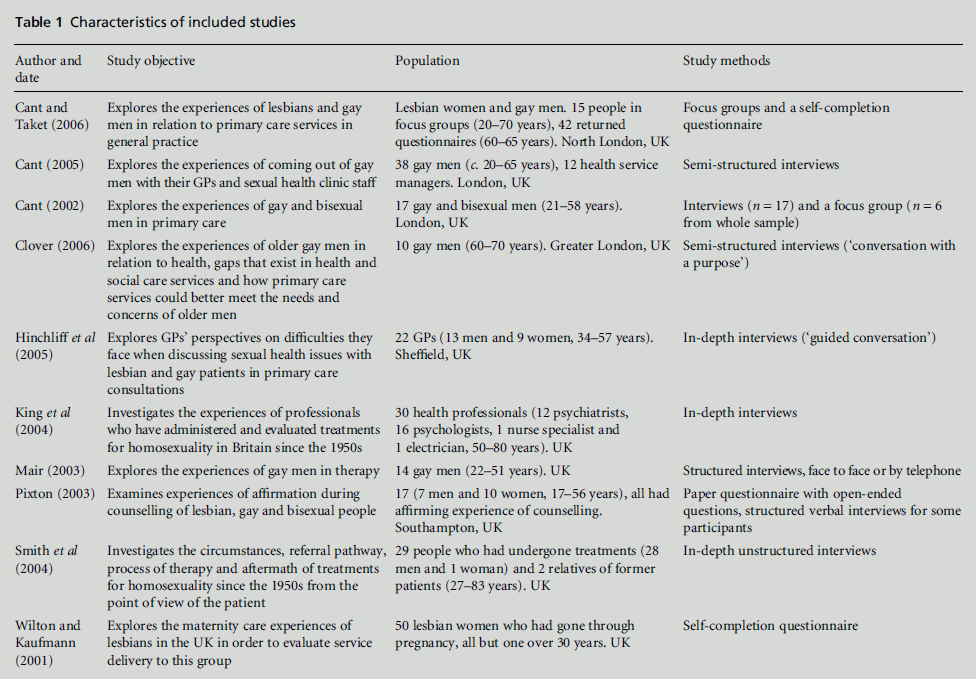
Study characteristics
The ten qualitative studies related to the experiences of
both LGB patients and healthcare professionals. They
addressed issues of patient–healthcare worker communication
and areas of health service provision. All
of the studies were conducted in the UK (four in
London, one in Sheffield, one in Southampton, and in
four studies the exact location was not specified).
Eight studies recounted the experiences of LGB
participants. Of these, four described the experiences
of LGB patients in general practice; three of these
studies concerned adults (Cant, 2002, 2005; Cant and
Taket, 2006) and the fourth concerned older adults
(Clover, 2006). A further two studies described the
experiences of therapeutic counselling for LGB participants
(Mair, 2003; Pixton, 2003), another study
described experiences with regard to the maternity
care of lesbian women (Wilton and Kaufmann, 2001),
and the final study described the experiences of gay men and lesbians who had undergone treatments for
homosexuality (Smith et al, 2004).
Two studies related accounts of practitioners. Of
these, one described GPs’ perspectives on consultations
with LGB patients (Hinchliff et al, 2005), and
the other described GPs’ views about administering
treatments for homosexuality (King et al, 2004).
All ten studies used qualitative techniques to collect
and analyse data. Eight studies used one-to-one interviews,
described in five of these studies as structured or
semi-structured interviews (Mair, 2003; Pixton, 2003;
Cant, 2005; Hinchliff et al, 2005; Clover, 2006) and in
two of the studies as in-depth, unstructured interviews
(King et al, 2004; Smith et al, 2004). The other interviews
were not described (Cant, 2002). Three studies used
self-completion questionnaires (Wilton and Kaufmann,
2001; Pixton, 2003; Cant and Taket, 2006), while two
involved focus groups (Cant, 2002; Cant and Taket,
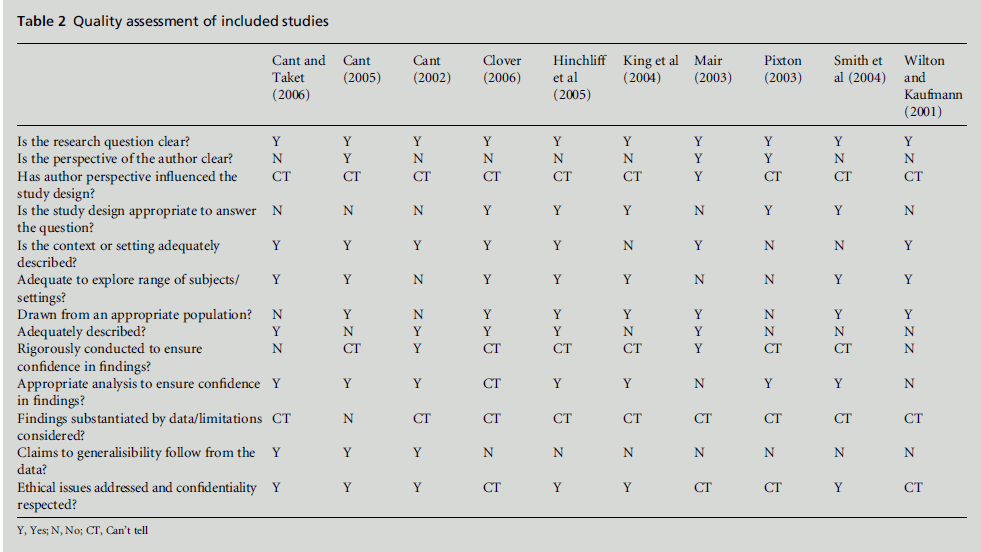
2006).The quality of each study was assessed asmoderate
or good, but the external validity (generalisability)was
often low (see Table 2).
Identified healthcare themes
Two themes were identified, namely potential improvements
in the relationship between healthcare
professionals and LGB patients, and potential improvements
in LGB healthcare at an institutional level.
In the following text, italicised quotes are used to
identify concepts from study participants, and nonitalicised
quotes identify concepts put forward by
study authors.
Improving the healthcare professional–
patient relationship
Barriers to communication between healthcare workers
and LGB patients were identified as an issue in the
majority of studies, and the following themes were identified as important for improving the relationship
between healthcare professionals and LGB patients.
Figure 1: Quorum diagram.
Table 1: Characteristics of included studies
Table 2:Quality assessment of included studies.
AVOIDING HOMOPHOBIA AND HETEROSEXISM
Homophobia in the healthcare setting was cited by LGB
respondents in three studies (Wilton and Kaufmann,
2001; Cant and Taket, 2006; Clover, 2006). Some
medical staff were described as having been ‘judgemental’,
‘patronising’, ‘intrusive’ or ‘rude’, or as having
shown a ‘lack of respect’ (Cant and Taket, 2006, p. 276).
There was some evidence of rough treatment (Cant
and Taket, 2006), poor emotional support for a suicidal
patient (Clover, 2006), and frequent reports of unprofessional
treatment on religious grounds (Wilton
and Kaufmann, 2001; Cant, 2002; Clover, 2006). In
studies of general practitioners, although most of
them showed an open approach to LGB patients, there
were some instances of unconcealed homophobia and
a suggestion of substandard quality of treatment (King
et al, 2004; Hinchliff et al, 2005).
Heterosexism, that is, the assumption that heterosexual
orientation is the norm, was commonly experienced
by LGB participants (Cant, 2002; Cant and
Taket, 2006). One woman recounted being asked
questions in the following conversation: ‘Are you
having sex? – Yes – Are you worried about getting pregnant?
– No – Why not? – My partner’s a woman – Oh
[with reported shock]’ (Cant and Taket, 2006, p. 275).
However, despite a heterosexist attitude being more
common, this was not always the case. For example,
another medical professional strived to ask questions
in a non-heterosexist way ‘Do you have a partner?’ or
‘Who do you live with?... I try and ask those sort of
neutral questions’ (Hinchliff et al, 2005, p. 350). Using
open questions that do not assume heterosexuality
may be an important step in overcoming barriers to
communication.
IMPROVING HEALTHCAREWORKERS’ KNOWLEDGE
Gay and lesbian respondents reported that various
aspects of LGB knowledge were important in discussions
with their GP, and there was concern that doctors
did not understand gay sexual practices (Mair, 2003;
Cant, 2005; Clover, 2006). This concern was also
expressed by GPs, who were worried that their lack
of knowledge about sexual practices might act as a
barrier to discussion (Hinchliff et al, 2005). However,
two other studies suggested that LGB patients did not
necessarily expect doctors to have detailed knowledge
(Wilton and Kaufmann, 2001; Cant, 2002), but that
they should ‘approach their patients with an open mind,
listen to them and engage with their experience.’ As one
gay man commented, ‘they’ve just got to keep their wits
about them and be able to talk intelligently’ (Cant, 2002,
p. 128). A lack of knowledge of terminology may not always limit effective treatment or inhibit good patient–
professional relationships if sensitivity and openness
are used to engage with the patient intelligently.
IMPROVING PATIENT TRUST
Five studies showed that LGB patients anticipated poor
treatment and/or homophobia from staff (Wilton and
Kaufmann, 2001; Cant, 2002, 2005; Mair, 2003; Clover,
2006). In one study it was noted that ‘anticipation or
fear of differing treatment was more common than
actual experiences of discrimination’ (Clover, 2006,
p. 46). An informant in a different study showed a
general mistrust, and his comment may summarise
the view of many LGB individuals: ‘A doctor’s a doctor,
init’ (Cant, 2005, p. 12). A preconceived notion that
doctors will not understand or approve of homosexuality
may act as a barrier, whereas improving trust may
increase attendance and aid the development of good
patient–professional relationships.
BEING PERCEPTIVE TO THE TERMINOLOGY USED
One study suggested that misunderstandings between
patient and doctor may result from the use of differing
terms to describe homosexuality. Some gay men chose
to describe themselves as homosexual, while others
rejected that term and preferred to describe themselves
as ‘gay’ (Mair, 2003). One respondent described
how this had acted as a barrier ‘... and I kept using the
word ‘‘gay’’ and they kept using the word ‘‘homosexual’’,
and I think it was that that distanced me’ (Mair, 2003,
p. 35). Differing preferences, held by different individuals,
may make communication difficult. It may be
important for doctors to be aware of the words that
each patient uses and to refer to terms that the patient
has chosen to describe their sexuality.
UNDERSTANDING EMBARRASSMENT
Apparent embarrassment or discomfort on the part of
healthcare professionals was identified as a potential
barrier to the relationship between patient and doctor.
In one study, the fact that GPs and/or medical staff
were ‘uncomfortable’ was listed by researchers along
with other clearly homophobic reactions, such as being
judgmental or rude (Cant and Taket, 2006, p. 276). A
gay man in another study reported that ‘I have a feeling
that she is somewhat homophobic really. She might
encourage me to talk [about gay issues] but her face is
saying ‘‘Oh my God!’’’ (Mair, 2003, p. 38). Discomfort
may result from homophobia, but it was suggested
that it might also result from general embarrassment.
In a study of GPs, ‘doctors reported feelings of shyness,
being uncomfortable and not wanting to be intrusive’
(Hinchliff et al, 2005, p. 348), and this embarrassment,
when perceived as homophobia, may have played a
role in the breakdown of communication. LGB patients may need to be perceptive and tolerant of practitioners’
discomfort until relationships of trust and
mutual understanding have developed.
REDUCING OVER-CAUTIOUSNESS
Two studies suggested that communication barriers
may result when healthcare workers and LGB patients
are over-cautious when relating to each other (Wilton
and Kaufmann, 2001; Hinchliff et al, 2005). A female
GP commented that ‘maybe I tread too carefully’
(Hinchliff et al, 2005, p. 349), and a lesbian woman
in another study expressed her frustration with the
healthcare professional’s timidity: ‘Using the word
LESBIAN! (It’s not catching)’ (Wilton and Kaufmann,
2001, p. 209). Humour was identified as promoting a
relaxed atmosphere. For example, one woman’s health
visitor commented ‘Oh, it’s just like that programme on
the telly!’ (Wilton and Kaufmann, 2001, p. 207), and
an LGB participant identified the importance of a bold
approach by both doctors and patients: ‘They ask you
straight out which I think is good ... but you’ve got to be
truthful because to get anything back you have to give
them the information’ (Cant, 2005, p. 14). An extremely
direct approach may not be appropriate in
all cases, and the ideal approach is likely to depend on
many factors, including the patient’s personality,
health needs, personal situation and past experiences.
Healthcare workers must be aware of the particular
needs of each patient in order to communicate with
them in the most appropriate and effective way.
IMPORTANCE OF AFFIRMATION
Four studies suggested that affirmation of LGB patients
was important for the development of a trusting relationship
(Wilton and Kaufmann, 2001; Mair, 2003;
Pixton, 2003; Clover, 2006).One gay man commented
that ‘He seemed to realise much more how I felt and he
was very concerned and he obviously seemed to think I
was a nice person’ (Clover, 2006, p. 46). There was also
an indication that ongoing dialogue was important in
order to affirm that the healthcare worker had a
positive attitude: ‘The initial statement ‘‘Gay is fine’’
was there, but there was no ongoing affirmation’ (Mair,
2003, p. 37). In the healthcare setting, although medical
staff may not see their role as primarily one of patient
affirmation, this may be an important contribution to
the emotional well-being of patients, and may help to
build patient trust and improve communication.
Removal of institutional barriers
Other barriers to healthcare were associated with
institutional-level issues, and common themes identified
changes necessary to improve LGB health service
provision.
IMPROVING PROTOCOLS
Two studies highlighted the fact that there was a lack
of appropriate protocols that were generic to both
homosexual and heterosexual patients (Wilton and
Kaufmann, 2001; Cant and Taket, 2006). The authors
of one study commented that ‘The design of the information
systems and the categories offered for recording
information were not inclusive of non-heterosexual
identities’ (Cant and Taket, 2006, p. 275). This was
highlighted as a particular problem by women in a
study of lesbian mothers: ‘My midwife asked me
questions ... that I didn’t really want to answer’ and ‘I
felt pressurised to give his [the father’s] name’, and the
lack of appropriate booking-in protocols was highlighted
by staff ‘apologising for the inadequacies of the
form’ (Wilton and Kaufmann, 2001, pp. 206, 208). A
systematic, transparent approach using a set protocol
that is applicable to people of all sexualities is desirable
in order to avoid inappropriate questions and patient
discomfort.
IMPROVING APPROPRIATE REFERRALS
Three studies suggested a lack of appropriate referrals
to social support groups and sexual health clinics for
LGB people (Cant, 2005; Cant and Taket, 2006;
Clover, 2006). Participants identified the importance
of social support groups (Wilton and Kaufmann, 2001;
Cant, 2005), one participant commenting that ‘The
group has achieved lots for me personally – cos I thought
that I was in a situation that no one else can understand,
but there’s so many other people in that situation in life’
(Cant, 2005, p. 13). However, although self-referral
was common, there was no evidence of GP referral to
these types of groups (Cant, 2005; Cant and Taket,
2006). The importance of support groups was evident
from the attitudes expressed. Lack of knowledge,
reflection or a desire to help may be the cause of the
poor rate of appropriate GP referrals. This may be an
important area for improvement where large benefits
for patients may be achieved.
IMPROVING PATIENT CONFIDENTIALITY
There were suggestions that confidentiality was not
always maintained with regard to issues of sexual
orientation (Wilton and Kaufmann, 2001; Cant, 2002,
2005; Cant and Taket, 2006). Particular fears relating
to confidentiality were that information might be
leaked and affect individuals’ applications to mortgage
and insurance companies (Cant, 2002, 2005; Cant and
Taket, 2006). There was also anxiety that information
might be shared and discussed with other members of
staff (Wilton and Kaufmann, 2001) and subsequently
reach the general community, with damaging effects
(Cant, 2002). The implementation of appropriate rules for confidentiality may reduce the risk of inappropriate
use of patient details and improve confidentiality.
IMPROVING CONTINUITY OF CARE
In one study (Wilton and Kaufmann, 2001), an area
that was identified as particularly important was the
extent to which patients felt that there was continuity
of care. This study examined the maternity experiences
of lesbian mothers, and many relevant comments
were made, for example, ‘I really wish I could
have had continuity of care, the same midwife throughout.
... This would have spared me so much anxiety’
(Wilton and Kaufmann, 2001, p. 209). Continuity of
care may be desirable for all those experiencing healthcare,
but it may be particularly important for LGB
individuals, and especially for lesbian women during
pregnancy and childbirth. Continuity of care limits
the number of times a person is required to reveal their
sexual orientation, and promotes the formation of a
trusting relationship between patient and healthcare
worker.
PROVISION OF LGB-FRIENDLY RESOURCES
A lack of overtly LGB-friendly resources in waiting
rooms was identified as a problem by participants in
a number of studies (Wilton and Kaufmann, 2001;
Cant, 2002, 2005; Clover, 2006). LGB-friendly literature
was seen to reassure LGB patients: ‘It would have been
helpful if literature and other spoken information gave
examples from lesbian or gay families ... so that it was
clear from the outset that there was not prejudice against
us’ (Wilton and Kaufmann, 2001, p. 209), ‘Why not
have some stuff that’s obviously gay ... if you see
something like that it does give you a lot of confidence’
(Cant, 2002, p. 128). A major function of this type of
literature may be to act as an assurance that practices
will be gay-friendly. As suggested by a GP participant in the study by Hinchliff et al (2005, p. 350), this might
also be achieved by presenting a clear non-discriminatory
policy so that ‘people have it in black and white
that they shouldn’t be discriminated against.’
IMPROVING TRAINING FOR HEALTHCARE
PROFESSIONALS
In one study that examined the views and experiences
of general practitioners (Hinchliff et al, 2005), many
spoke of the need for better training, particularly in
relation to understanding sexual practices among
lesbian and gay people. However, there was a suggestion
that the important skills may need to be developed
over time. For example, ‘Two participants
described how, through direct experience of lesbians
and gay men consulting about their sexual health, they
had progressively overcome the difficulties which they
faced’, and one GP commented that ‘You almost have
to practise feeling comfortable and familiar’ (Hinchliff
et al, 2005, p. 349). The investigators in this study
highlighted the importance of experimental learning,
identified by doctors as a positive way to become used
to discussing sexual health issues with gay and lesbian
patients (Hinchliff et al, 2005). Real interaction with
LGB patients, rather than theoretical teaching, may be
important for developing skills for good professional–
patient communication.
Discussion
This systematic review covered issues that may be
important for improving health services to LGB individuals.
One factor that was frequently evident, namely
internalised homophobia (Mair, 2003; Smith et al,
2004; Cant, 2005), was not discussed because it was
beyond the scope of the review, but it may be an
important factor for future consideration. Internalised homophobia has been defined as the internalisation
of experienced prejudice and social stigmatisation,
resulting in poor self-regard and internal conflict
(Williamson, 2000). It may manifest itself in denial
of sexual orientation, attempts to change, low selfesteem
and contempt for other LGB individuals (Rainbow
Project, 2009). It may be particularly important
during the teenage years (Scourfield et al, 2008), and
one investigator described how ‘its existence had a
profound impact on my awareness of just how deeply gay
men’s development can be affected by the negative
messages which have been internalised during maturation’
(Mair, 2003, p. 35). Even with positive changes
in health service provision, internalised homophobia
may persist. Suggestions made in the current review
should therefore be applied in the context of possible
internalised homophobia, and awareness among medical
professionals may promote better understanding
of their patients’ needs and responses.
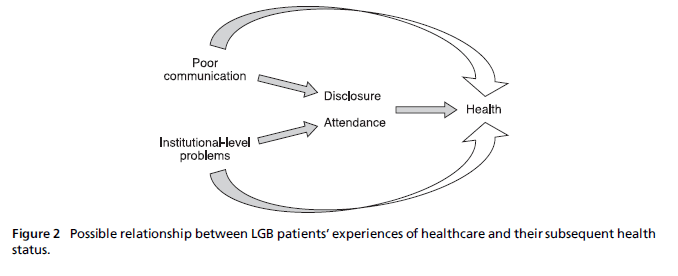
Figure 2: Possible relationship between LGB patientsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ experiences of healthcare and their subsequent health
status.
Validation
It is useful to compare the findings of the present
review with those reported by other investigators.
There is little published literature from the UK to
support or dispute the current findings, but there are a
number of studies fromthe USA and elsewhere which,
despite some limitations of applicability, are useful for
validating the current work, and these are discussed
below.
Consistent with the findings of this review, a review
of lesbian experiences of childbirth in the USA highlighted
the existence of homophobia in health services,
with examples given of poor treatment and unprofessional
conduct (McManus et al, 2006). Experiences
of heterosexism in health services in Australia have
also been described (Hughes, 2007) and, as in the
present review, showed heterosexism at both personal
and institutional levels. In studies included in the
current review, participants commented on the importance
of not making heterosexist assumptions, a
factor that was also highlighted by lesbian women in
another study conducted in Norway (Bjorkman and
Malterud, 2007).
The present review highlighted the fact that many
LGB patients have a preconception that doctors will
show prejudice. A review of lesbian women’s experiences
(McManus et al, 2006) showed that the degree of
disclosure of sexual orientation varied widely between
studies (41–90%), but that more than a third of
women believed that disclosure would negatively affect
their healthcare. Privacy was identified in another US
study as one of the most important factors that
promoted feeling safe in a healthcare setting (Ginsburg
et al, 2002), and issues relating to confidentiality,
frequently cited in studies included in the present review, may also be a concern for LGB individuals in
other countries.
Finally, the importance of training for healthcare
professionals, from the point of view of both patients
and professionals, was also highlighted by researchers
elsewhere. A large review of lesbian and gay healthcare
in Norway identified it as a major barrier to effective
communication (Bonvicini and Perlin, 2003), and this
may be a common inadequacy in many health services.
These international studies indicate that the
current work may therefore be applicable to healthcare
settings in other westernised countries. However,
its applicability to less developed countries, for which
there may be no published literature, is unclear.
Limitations
The current review highlights issues that affect relationships
between LGB patients and healthcare professionals,
and barriers to healthcare at the institutional
level. However, it does not provide evidence for a
causal link between these issues and subsequent LGB
health. One possible hypothesis is that these factors
have a direct impact on health or that they may affect
attendance at health services and disclosure of sexuality
to GPs, which in turn has an impact on health
status (see Figure 2).
The connection between these factors may seem
logical, but the degree of influence is uncertain, and
this may limit the usefulness of the current review.
Further research may be required to bring to light the
extent to which patient experiences of healthcare affect
their subsequent health status. However, despite this
limitation, the review describes experiences of healthcare
that may in themselves be considered important
end points. Like all patients, LGB patients may reasonably
expect to encounter respect, professionalism and
engagement in the health service, and issues relating to
experiences of healthcare may therefore be seen as
important in their own right.
The changing legal and social climate may also pose
some limitations to the interpretation of this review.
In the UK, there have recently been a number of
legislative changes, such as the Equality Act (Sexual
Orientation) Regulations 2007 (Office of Public Sector
Information, 2007), which makes discrimination in
the provision of goods and services on the basis of
sexual orientation unlawful, and applies to public
bodies such as the NHS. In addition, from September
2008, the Department of Health Lesbian, Gay, Bisexual
and Transgender Advisory Group (Department of
Health, 2008) was established to inform service development
and improvement.
These legal and political changes are welcome
reforms that are likely to have a positive impact not
only on the legal rights of LGB individuals, but also on attitudes and practices in general society. The current
review brings together all of the available research to
date, but the studies included in the review were conducted
before many of the recent legislative changes.
This review may therefore be a better reflection of
barriers to LGB healthcare that existed five years ago,
and does not necessarily reflect present-day status.
However, it may take time for the legal changes to
result in social change, and it is likely that many of the
issues highlighted in the review are still relevant. It
may be of interest to compare the findings of this
review with future research in order to assess the
impact of the legal changes on barriers to LGB health.
The current review may be limited by the amount of
published research available. The aim was to report
only on material of relevance to the UK, so that the
review might be directly applicable to the UK population.
However, this restricted the amount of information
available and excluded the larger body of
literature from the USA. In addition, the majority of
included studies were conducted in London (four
studies) or other large cities (one study in Sheffield
and one in Southampton). It appears likely that the
data will have been derived mainly from LGB patients
living in large urban centres, and may not be representative
of those living in smaller towns or villages.
Despite these limitations, the findings appear to be
consistent with those from studies and reviews conducted
in other countries and settings, which suggests
that the current review provides a reliable representation
of barriers to positive experiences of LGB
healthcare.
Quality assessment of qualitative studies continues
to be an area of controversy. Despite using a checklist
that was considered to provide a reasonable assessment
of study quality (Wallace et al, 2004), there were
still likely to be areas of uncertainty. This is due not
only to the ability of the checklist to identify areas of
bias, but also to uncertainty in relation to the question
‘What is a good piece of qualitative research?’ The
generalisability of the included studies was highlighted
as an important issue in applying them to the whole
LGB population, and in order to address this limitation
the findings were presented in a transparent
way, referring to the details of studies, such as population
and setting, when reporting the results.
The appropriateness of conducting systematic reviews
of qualitative research may be questioned. It is
debatable whether information from studies with
different population samples, different experimental
aims and different methods of data collection can
be considered and grouped within the same themes.
Themes in this review can also only reflect research to
date, and will inevitably fail to identify issues that have
not yet been identified in primary studies.
Conclusion
This systematic review may be limited by the quantity
and applicability of published research, and is unlikely
to cover every important issue. However, despite these
limitations, it continues to highlight many important
issues in LGB healthcare, providing direction for
equality-driven change. Recommendations from this
review are that there is a need for the following:
• specific training for healthcare professionals in relation
to LGB patients and their health
• information for healthcare professionals about relevant
social groups and health establishments for
referrals
• LGB- or non-sexuality-specific literature to be made
available in healthcare establishments
• protocols that make no assumptions about sexual
orientation
• strict measures to ensure confidentiality for LGB
patients
• better continuity of care for LGB patients.
Future research may involve investigation of the relationship
between LGB patients’ experiences of healthcare
and their subsequent health status. In addition,
future research, if compared with the findings of the
current review, may allow recent legal and political
changes to be assessed in the light of their impact on
LGB individuals’ health.
CONFLICTS OF INTEREST
None.
References
- BjorkmanMandMalterudK(2007) Being lesbian ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â does thedoctor need to know? Scandinavian Journal of PrimaryHealth Care 25:58ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â62.
- Bonvicini KA and Perlin MJ (2003) The same but different:clinicianÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âpatient communication with gay and lesbianpatients. Patient Education and Counseling51:115ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â22.
- Britten N, Campbell R, Pope C et al (2002) Using metaethnographyto synthesise qualitative research: a workedexample. Journal of Health Services Research and Policy7:209ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â15.
- Cant B (2002) An exploration of the views of gay andbisexual men in one London borough of both theirprimary care needs and the practice of primary carepractitioners. Primary Healthcare Research and Development3:124ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â30.
- Cant B (2005) Exploring the implications for health professionalsof men coming out as gay in healthcare settings.Health and Social Care in the Community 14:9ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â16.
- Cant B and Taket A (2006) Lesbian and gay experiences ofprimary care in one borough in North London, UK.Diversity in Health and Social Care 4:271ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Clover D (2006) Overcoming barriers for older gay men inthe use of health services: a qualitative study of growingolder, sexuality and health. Health Education Journal65:41ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â52.
- Department of Health (2008) Lesbian, Gay, Bisexual andTransgender AdvisoryGroup; www.dh.gov.uk/en/Managing yourorganisation/Equalityandhumanrights/DH_4136008 (accessed February 2009).
- Department of Trade and Industry (2004) Final RegulatoryImpact Assessment: Civil Partnership Act 2004. London:Department of Trade and Industry.
- Ginsburg KR, Winn RJ, Rudy BJ et al (2002) How to reachsexual minority youth in the health care setting: the teensoffer guidance. Journal of Adolescent Health 31:407ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â16.
- Hinchliff S, Gott M and Galena E (2005) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âI daresay I mightfind it embarrassingÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢: general practitionersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ perspectiveson discussing sexual health issues with lesbian and gaypatients. Health and Social Care in the Community 13:345ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
- Hughes M (2007) Older lesbians and gays accessing healthand aged-care services. Australian Social Work 60:197ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â209.
- King M, Smith G and Bartlett A (2004) Treatments ofhomosexuality in Britain since the 1950s ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â an oral history:the experience of professionals. BMJ 328:429.
- King M, Semlyen J, Tai SS et al (2008) A systematic review ofmental disorder, suicide and deliberate self-harm inlesbian, gay and bisexual people. BMC Psychiatry 8:1ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â17.
- McManus AJ, Hunter LP and Renn H (2006) Lesbianexperiences and needs during childbirth: guidance forhealth care providers. Journal of Obstetric, Gynecologic andNeonatal Nursing 35:13ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â23.
- Mair D (2003) Gay menÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s experiences of therapy. Counsellingand Psychotherapy Research 3:33ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â41.
- Meads C, Pennant M, McManus J et al (2009) A SystematicReview of Lesbian, Gay, Bisexual and Transgender Health intheWest Midlands Region of the UK Compared to PublishedUK Research. Birmingham: West Midlands Health TechnologyAssessment Collaboration, Unit of Public Health,Epidemiology and Biostatistics, University of Birmingham.Office of Public Sector Information (2007) The Equality Act(Sexual Orientation) Regulations 2007; www.opsi.gov.uk/si/si2007/uksi_20071263_en_1 (accessed February 2009).`
- Pixton S (2003) Experiencing gay affirmative therapy: anexploration of clientsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ views of what is helpful. Counsellingand Psychotherapy Research 3:211ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â15.
- Rainbow Project (2009) Internalised Homophobia; https://rainbow-project.org/dev/node/41 (accessed February 2009).
- Scourfield J, Roen K and McDermott L (2008) Lesbian, gay,bisexual and transgender young peopleÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s experiences ofdistress: resilience, ambivalence and self-destructive behaviour.Health and Social Care in the Community 16:329ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â36.
- Smith G, Bartlett A and King M (2004) Treatments ofhomosexuality in Britain since the 1950s ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â an oral history:the experience of patients. BMJ 328:427.
- Wallace A, Croucher K, QuilagarsDet al (2004) Meeting thechallenge: developing systematic reviewing in social policy.Policy and Politics 32:455ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â70.
- Williamson IR (2000) Internalized homophobia and healthissues affecting lesbians and gay men. Health EducationResearch 15:97ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â107.
- Wilton T and Kaufmann T (2001) Lesbian mothersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ experiences of maternity care in the UK. Midwifery 17:203ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â11.