Keywords
Polio vaccine hesitancy; Vaccine diplomacy; Vaccine acceptability
Introduction
Poliomyelitis a single stranded, positive sense RNA virus belonging to the Picornaviridae family once terrified the world. However, the virus has largely been eradicated due to the progression and implementation of successful vaccination programs. Striking suddenly in children under 5 and causing an asymmetrical and ascending paralysis in its victims, polio causes death by paralyzing the muscles of respirations. The first epidemic of polio was seen in the United States in 1894. However, in 1953, Dr. Jonas Salk and his associates at the University of Pittsburgh were successful in developing an inactivated, injected vaccine, which lowered the incidence of Polio in the United States by 85%- 90%. Furthermore, in 1962, the Sabin vaccine was created, which was more economically feasible and easier to administer due to it being administered orally. In 1979, the United States saw its last case of polio caused by a viral strain of the virus due to successful prophylaxis from vaccination protocol [1].
In 1988, the Global Polio Eradication Initiative (GPEI) was formed after a resolution to eradicate polio worldwide was passed by the World Health Assembly. Using the Sabin vaccine, the GPEI has decreased the global incidence of polio by 99.9%. To date, it is estimated that a total of 16 million paralyses have been prevented by the GPEI and 1.5 million lives have been saved. Despite the hard work of the GPEI, the remaining 0.1% of endemic polio cases are seen largely in the poorest and underdeveloped regions of Afghanistan, Nigeria, and Pakistan [2].
In these endemic regions, polio essentially targets children under the age of 5, yielding an irreversible paralysis of the lower limbs in 1 out of 200 cases. Moreover, as a result of paralysis, it is estimated that 5%-10% of the affected individuals succumb to the viral infection as it spreads to their respiration muscles [3]. Aside from the tragic outcome of the virus, it is imperative to vaccinate every child to prevent the spread of illness. In a majority of cases, the illness presents with generic flu like symptoms such as sore throat, fever, headache, and nausea. Moreover, although these symptoms are self-limiting, the virus is still able to spread from an infected person to another before the symptoms appear or within 2 weeks after the first symptom. Furthermore, the virus can be passed from person to person after the resolution of symptoms in an infected person in unsanitary conditions. This is because the virus can survive within an individual’s fecal matter and contaminate food and water sources [4]. This is a particularly important mode of transmission in the underdeveloped regions of these endemic countries due to the lack of proper hygiene and filtration within the water sources. Additionally, due to the lack of financial spending power within the population of these endemic regions, a weakened immune system puts people at a larger risk of contracting the virus.
Albeit the diligent efforts of GPEI, Afghanistan reported 21 cases of the polio virus in 2019, having a total of 8 districts confirmed for the viral infection. Moreover, Pakistan reported 86 cases of polio in 2019, in which the most endemic region was Khyber Pakhtunkhwa [5]. To date, a total of 3 wild strains for polio virus have been found. All 3 strains must have a human host to survive and replicate. However, a strain can only spread between unvaccinated individuals because in vaccinated individuals there is no risk of hosting the viral strains. Due to large vaccination efforts, type 2 wild poliovirus became eradicated in 1999 and a case of type 3 wild poliovirus has not been experienced worldwide since 2012 [3]. The strains found in the endemic region consist of poliovirus type 1 and circulating vaccine-derived poliovirus type 2 (cVDPV) [5].
Amongst the 3 endemic regions, Nigeria does not suffer from wild poliovirus, rather it faces the issue of circulating vaccine-derived poliovirus type 2 [6]. The risk of cVDPV is seen in a region where the oral polio vaccine (OPV) is used. Due to OPV containing a weakened vaccine-virus, an immune response is elicited within the body. Due to this immune response, the vaccine-virus is allowed to replicate within the intestines and develop immunity via the construction of antibodies. During the time of the immune response, the vaccine virus is excreted, which puts large populations of under immunized regions at a risk for contracting the strain [7]. Contrary to endemic countries, the United States uses an injected, inactivated method to administer a polio vaccine. This method is used over the oral vaccine to prevent the possibility of cVDPV. Utilizing this difference, differences in laws and methods of education, the purpose of this paper is to implement vaccination programs used in the United States as a framework to increase vaccination awareness in developing countries. In doing so, vaccination practices to tackle the issues in the remaining endemic regions of poliomyelitis can be improved.
Methods
The purpose for researching the articles used in this review paper was to identify the issues endemic countries face in their attempts to eradicate polio. Further, another goal of the articles was to utilize methods the United States has implemented to deal with similar issues challenging these endemic countries. Search engines such as PubMed and Google Scholar were used to find articles relating to the hypothesis. These articles would then be used to see if the hypothesis should be accepted or negated.
Upon searching for relevant articles, abstracts were read in various articles. If an article’s abstract shared similar information to another, the latter article was negated. Moreover, if an article spoke about cross border relationships, the article was negated. In order to narrow the search results and find articles that accurately represented the goals for this review, specific search terms were used. These search terms included “the role of immunization laws”, “polio eradication challenges in Pakistan”, “vaccine derived poliovirus in Nigeria”, “polio prevention in the United States”, “mandatory school laws for vaccines”, “educating parents on children vaccines”, “cultural and religious vaccine barriers”, “vaccination effects on herd immunity in the United States”, and “use of inactivated polio vaccine in the United States”. Moreover, to further narrow the articles presented upon searches in the databases, keywords were utilized. Important keywords include: “vaccine hesitancy”, “polio eradication”, “wild polio virus”, “circulatory vaccine derived polio virus”, “vaccine diplomacy”, “vaccine acceptability”, “vaccine refusal”, and “parental decision-making”.
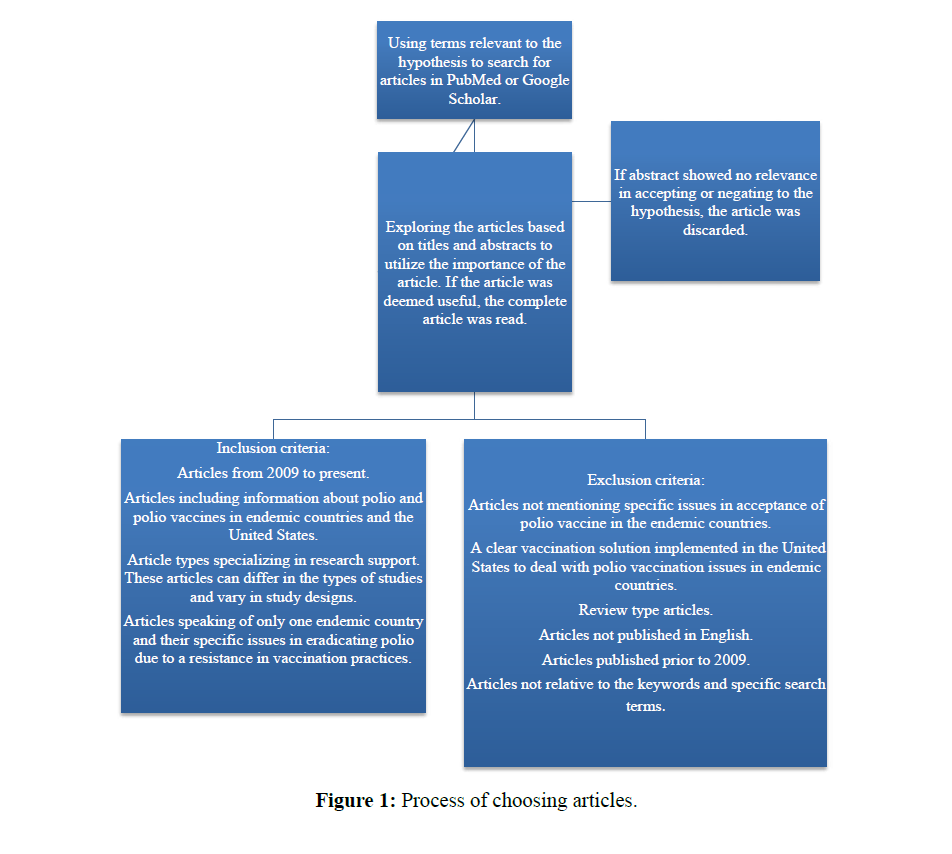
Aside from utilizing search terms and key words to find articles, an inclusion and exclusion criteria was used. Figure 1 illustrates how relevant articles were chosen to be a part of this paper. Exclusion criteria’s included articles written prior to 2009 (a 10-year time frame), research based articles, and articles of relevance to the hypothesis that were not based around a single endemic country or the United States. Moreover, the inclusion criteria included articles of relevance to the hypothesis, and articles having a clear cut solution found within the United States for an issue faced by an endemic country relevant to eradicating polio virus.
Figure 1: Process of choosing articles.
Many articles were read to gather the information provided in this review paper. However, to ensure that the information is relevant to the hypothesis, a total of 10 articles were used for analysis purposes. The complete list of these articles can be found in Table 1. It is imperative to note that the articles listed in Table 1 were used for both the results and discussions section. If an article was used only for the results section or only for the discussion section, it was cited, but not listed in the Table. Furthermore, to further simplify the data analyzed, Table 2 lists a summary of the number and type of study designs utilized within the paper (Table 2).
| Ref. |
First Author |
Publication Date |
Study Design |
Evidence Level |
Study Population |
Objective |
Results |
| [8] |
Chung |
2017 |
Cross Sectional |
3 |
Parents of children aged 7 or younger |
Assessing influence on parental vaccination decisions |
Healthcare providers, specifically doctors, play an important role in influencing parental decision to vaccinate children. |
| [9] |
Shah |
2019 |
Quantitative |
6 |
Pakhtun journalists covering health issues in high-risk districts for WPV |
Can health covering journalists be a useful resource in the fight to eradicate polio in Pakistan |
Educating Pakhtun health journalists can lead to a gain in important partners to eradicate polio. |
| [10] |
Greenfield |
2015 |
Quantitative |
3 |
Hispanic, Somali, Ethiopian, and Eritrean adolescents. Parents of adolescents, and three focus groups with mothers of 11-18 year olds |
Identifying attitudes and knowledge of adolescent vaccination recommendations amongst varying ethnicities |
Knowledge of beliefs, misperceptions, and concerns can help improve adolescent vaccination in ethnic groups especially if recommended by a physician. |
| [11] |
Murakami |
2014 |
Cross Sectional |
7 |
Lady health workers, local health managers and officials along with mothers of children less than 1 year of age for qualitative study. LHWs and mothers of children less than 1 year of age for quantitative. |
Gather community perceptions of the OPV in Khyber Pakhtun Province. |
PEI needs to focus on local religious and cultural values of the endemic region to gain an acceptance of OPV. |
| [12] |
Iqbal |
2015 |
Case Control |
4 |
Cases of adverse effects submitted to VAERS following the administration of IPV. |
Analyze the adverse effects of IPV and compare them to OPV usage. |
Events following IPV administration were fairly few as IPV was deemed safe when compared to OPV. |
| [13] |
Saleem |
2018 |
Control Trial |
2 |
265 children at 22 weeks seronegative for PV2. |
Evaluating response strategies in occurrence of cVDPV2 outbreaks. |
Adding a dose of IPV along with OPV helps to induce a stronger immune response than OPV alone and decreases the shed of PV2 in feces. |
| [14] |
Jenkins |
2010 |
Case Series |
6 |
Cases of acute flaccid paralysis associated with excretion of type 2 cVDPV, type 1 WPV, and type 3 WPV. |
Compare pathogenicity, the clinical severity, and effectiveness of OPV in varying cases of poliovirus. |
No significant differences were found in the clinical severity, but it was concluded that OPV is more effective for cVDPV than type 1 and 3 WPV. |
| [15] |
Barraza |
2017 |
Qualitative |
6 |
Vaccination laws unique to each state. |
How state mandated laws deal with vaccination preventable illness in cases of outbreaks. |
Through adaptation of new vaccination laws in response to recent preventable illness, state laws have ensured that parents provide children with proper vaccinations to attend school and have made vaccinations more accessible via the extension of health care workers who can administer them. |
| [16] |
Wallace |
2014 |
Qualitative |
6 |
Vaccination protocols for people traveling to and from endemic countries of poliovirus. |
Review protocols placed to prevent the risk of poliovirus from being brought into the United States via travel. |
The CDC has provided people traveling to countries with risks of poliovirus with vaccination programs complying to fit the travelers’ schedule. Moreover, it has also made it mandatory for travelers coming into the US from such places to show proof of vaccination prior to entering. |
| [17] |
Bawa |
2018 |
Cross sectional |
6 |
Nomadic populations moving across Nigerian borders. |
Determining entry and exit points along with resting points of routes taken by nomadic pastoralists. |
There is a need for transboundary policies amongst the border of Nigeria to provide vaccination for prevention of polio from being brought in and out of the country. |
Table 1: Evidence Table of Reviewed Articles.
| Study Design |
Number of Studies Reviewed |
| Cross Sectional |
3 |
| Quantitative |
2 |
| Case Control |
1 |
| Control Trial |
1 |
| Case Series |
1 |
| Qualitative |
2 |
Table 2: Summary of Study Designs Reviewed.
Results
Implementing educational based programs
In 2012 and 2014, national web-based surveys targeting US parents of children under the ages of 7 were conducted. In the surveys, a total of 2,603 parents participated in 2012 and 2,518 in 2014. The purpose of these surveys was to assess the influences in decision making regarding vaccination practices to their children and to examine the parents’ source of vaccination information. To further simplify the survey, parents were organized by categories of their vaccination decision making. These categories included non-hesitant acceptors, hesitant acceptors, delayers, and refusers. Moreover, to further understand what led the parents to be in their specific category, factors such as source of information and advice providers were considered [8].
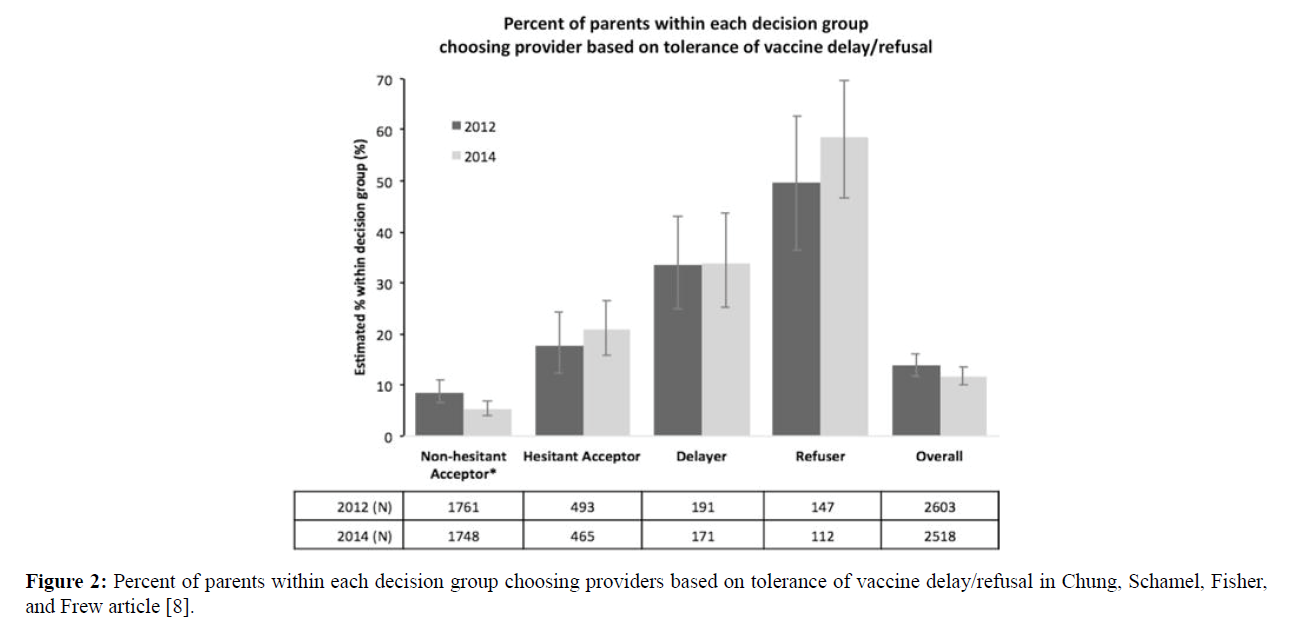
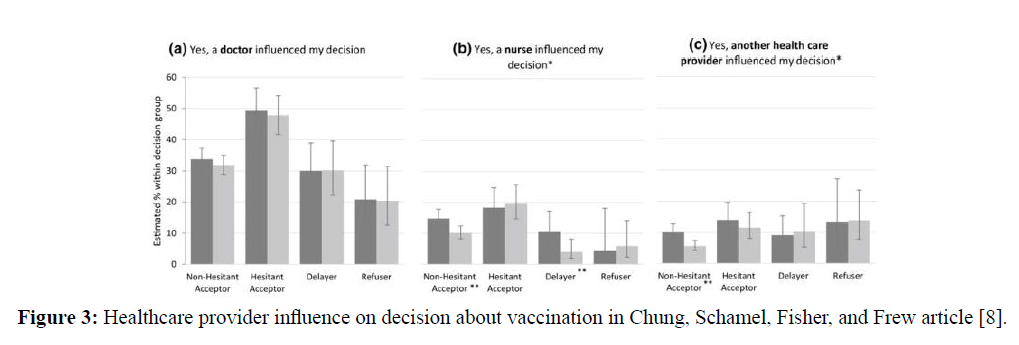
The surveys found that parents who fell in the categories of delayers and refusers were likely to know other parents whose children suffered from adverse effects of vaccines. Moreover, the survey also concluded that these parents were more likely to be a part of a social circle involving parents of similar beliefs for vaccinating their children. As shown in Figure 2, a large percentage of “delayers” (33.4% in 2012 and 33.9% in 2014) and “refusers” (49.6% in 2012 and 58.6% in 2014) chose their primary healthcare providers based on the provider’s ability to agree with the parent’s decisions. However, as shown in Figure 3, parents who fit in the category of “hesitant acceptors” said their decisions to finally vaccinate their children occurred when educated by a physician. This held true for parents who fell in the categories of “delayer” and “refusals” as well. Moreover, as informed in Figure 3, when it came to influencing parents to vaccinate upon the advice of a nurse or another health advisor such as a pharmacist or physician assistant, parents who fell in the category of “non-hesitant acceptors” and “delayers” showed a decrease in influencing power from 2012 to 2014 [8].
Figure 2: Percent of parents within each decision group choosing providers based on tolerance of vaccine delay/refusal in Chung, Schamel, Fisher, and Frew article [8].
Figure 3: Healthcare provider influence on decision about vaccination in Chung, Schamel, Fisher, and Frew article [8].
In June 2019, a quantitative study done in Pakistan involving the recruitment and interviewing of 33 Pakhtun journalists responsible for covering health issues in high risk areas such as Khyber Pakhtunkhwa for wild poliovirus was performed. The study found all 33 journalists to strongly be in favor of the oral polio vaccine and were adamant that children get vaccinated against polio. However, the journalists informed of their struggles to convey information about the vaccines due to a limited health literacy stating that information about the oral polio vaccine is generally received only from officials associated with the OPV campaigns. Lastly, the study found that properly educated health journalists can play a large role towards the eradication of polio in Pakistan [9].
In 2015, in-person surveys were given to members of diverse ethnic communities in King County, Washington. The purpose of the study was to identify knowledge, attitudes, and barriers of adolescent vaccination recommendations amongst differing communities. Ethnicities asked to take the survey ranged from Hispanic, Somali, Ethiopian and Eritrean. The survey comprised of 45 people falling in the age range of adolescence, 157 parents of adolescents, and three focus groups with mothers of 11 to 18 year olds. Upon the completion of the survey, chi-square testing and Fisher exact testing were used to evaluate difference of opinion within the ethnic groups. The largest reasoning for unvaccinated children in the ethnic groups was a lack of vaccination knowledge in the parental population [10].
Findings were then used to develop brochures that are specific to cultural beliefs addressing misunderstandings about adolescent immunization, recommended adolescent vaccines and vaccine preventable diseases. Furthermore, a presentation highlighting the findings of the survey was given to healthcare providers of specific ethnic communities. This was done because parents in the survey identified doctors as their only source of trusted health information concluding that they would vaccinate their children if recommended by a physician. Following the completion of the presentation, health care providers were surveyed concluding that 80% would be more like to recommend vaccination upon routine visits. These numbers were increased from the 55% of the surveyed HCPs that recommended vaccinations at acute visits and 35% at injury visits prior to the presentation [10].
Due to the Polio Eradication Initiative facing the issue of refusal in acceptance of the oral polio vaccine, a qualitative and quantitative study was performed to collect information in the Khyber Pakhtunkhwa Province. An endemic region for polio virus in Pakistan, the study, which took place in 2007, was done to investigate community perceptions of the OPV and to estimate the prevalence of OPV refusal. Qualitative data focused on community opinions was gathered via a focus group discussion amongst lady health workers (LHWs), mothers of children less than 1 year of age, and interviews with local health managers and officials. Moreover, quantitative data was gathered by giving a questionnaire survey to 200 LHWs and 210 mothers with children younger than 1 year of age [11].
The qualitative method found that OPV was refused due to local misinterpretations of the vaccine. It is believed that OPV contained birth control or pork, both of which are against the Islamic beliefs of the residents. Moreover, discovered via the qualitative method, is a shared belief that OPV was a foreign plot against Muslims, and that vaccination was against the fate determined by god. Furthermore, the quantitative survey revealed that lady health workers encountered an OPV refusal up to 33%, while mothers were unwilling to give their children the OPV up to 5.7% of the time [11].
Implementing a change in method of vaccination administration
A case control study performed in the United States was done to analyze the side effects associated with inactivated poliovirus vaccine (IPV). The purpose of the study was to utilize safety measures when it came to the usage of IPV as implementing this form of vaccine is vital for the global eradication of polio. From January 1, 2000 to December 31, 2012, data submitted to the US Vaccine Adverse Event Reporting System (VAERS) was analyzed to gather the side effects of IPV when given individually or in combination with other vaccines for all ages and sexes. The cases that were analyzed were categorized by types of adverse effects. These categories were divided by “non-serious”, “non-fatal serious”, and “death reports”. Furthermore, in the event that a case fell under the death reports category, the cause of death was identified and categorized by body-system (cardiovascular, respiratory, gastrointestinal, etc.). Moreover, to analyze safety profiles of IPV as opposed to oral poliovirus vaccine (OPV), data gathered by VAERS from 1991-2000 was compared for the respective vaccine [12].
A total of 41,792 reports were submitted, in which 39,568 (95%) were for children younger than 7. Out of these 39,568 cases, 38,381 (97%) were for co-administration of vaccines (commonly pneumococcal and acellular pertussis vaccine) given with the IPV. However, only 0-5% of cases submitted were for independent IPV scenarios. Additionally, of the collected cases, 34,880 (88%) fell under the non-serious category, 3,905 (10%) cases fell under the non-fatal serious category, and 783 (2%) were death reports. The most common non-serious events were injection-site erythema (29%) and pyrexia (38%) for non-fatal serious events. Of the cases that resulted in death reports, the majority (96%) were seen in children less than 1 year of age with 52% reporting the cause to be sudden infant death syndrome. Moreover, when comparing IPV to OPV, the safety profiles of combining each vaccination with whole-cell pertussis vaccines or with acellular pertussis vaccines were similar. It was concluded from the study that when compared to the 250 million doses of IPV given in the United States from 2000-2012, few adverse events were reported and no new vaccination safety issues were identified [12].
A randomized controlled trial was performed in Pakistan to evaluate existing response strategies in cases of circulating vaccine derived polioviruses type 2 (cVDPV2) outbreaks. In the trial, 265 children at 22 weeks of life, all of whom were seronegative for poliovirus type 2 (PV2) were assigned to one of four study groups. The groups consisted of 1 dose of trivalent oral poliovirus vaccine (tOPV), monovalent OPV 2 (mOPV2), tOPV along with a dosage of inactivated poliovirus vaccine (IPV), and mOPV2 with IPV type 2 [13].
Upon collection of stool and blood samples, seroconversion was achieved 48% in groups with 1 dosage of tOPV, 76% in mOPV2, 98% in tOPV along with a dosage of IPV, and 100% in mOPV2 with IPV type 2. Moreover, the trial found mOPV2 to be more immunogenic than tOPV alone and OPV to be more immunogenic when combined with IPV than when given by itself. Furthermore, shedding of PV2 in feces was lowest when tOPV was combined with IPV as opposed to it being the highest when given by itself. Hence, from the study, it can be concluded that adding IPV to OPV not only improves immunological response, but also helps to decrease the shed of PV2 in feces [13].
A case series study was performed in Nigeria following the outbreak of circulating vaccine-derived poliovirus (cVDPV) in 2010. The purpose of the study was to analyze the pathogenicity, the clinical severity, and the effectiveness of oral poliovirus vaccine in cVDPV as opposed to wild-type poliovirus (WPV). To carry out the study, cases of acute flaccid paralysis associated with fecal excretion of type 2 cVDPV, type 1 WPV, and type 3 WPV were identified from January 1, 2005 to June 30, 2009 [14].
The study found no significant differences in clinical severity amongst the paralysis in 278 cases of cVDPV type 2, 2323 cases of type 1 WPV, and 1059 cases of type 3 WPV. Moreover, it was estimated that trivalent oral polio vaccine (tOPV) has an effective rate of 38% against the prevention of paralysis in scenarios involving type 2 cVDPV. Furthermore, the study concluded that tOPV has an effect rate of 13% when used for prevention of type 1 WPV, and 20% for type 3 WPV. Hence, the study concluded that tOPV is more potent for prophalxysis of type 2 cVDPV than it is for type 1 WPV and type 3 WPV [14].
Implementing law mandated programs for vaccination
A qualitative study was performed to identify state vaccination policies in the United States. The study focused on mandatory vaccination policies required for school entrance and healthcare worker vaccinations. Furthermore, the study focuses on expanding vaccine access granting healthcare workers such as pharmacists’ permission under law to administer vaccination. This study was done following the outbreak of measles, a previously eradicated illness due largely to vaccination practices. However, the study found the cause of the outbreak to be individuals who deliberately chose to forego vaccination [15].
In order to decrease outbreaks in vaccine preventable illness, all 50 states in the US have mandatory vaccination laws. For instance, if a child isn’t vaccinated per state requirements, they can’t be enrolled in public or private schools. In order for a child to be enrolled in school, proof of vaccination for MMR and polio must be provided. Furthermore, having unique laws for each state allows the state to act in the best interest of its population and deal with any ongoing crisis. For example, the study found that one measles outbreak from late 2014 to early 2015, originating from a California theme park resulted in 125 cases and spread through 8 states. Amongst these 125 cases, 110 were seen in California residents of whom 45% were unvaccinated and 43% had status of unknown vaccinations. Following the outbreak, California passed a law making it more difficult for parents to avoid mandatory vaccinations for their children. The law restricted parents who seek vaccination exemption for personal or religious beliefs, allowing children only to be exempt from vaccination practices for medical reasons. Another way states have started to increase vaccination practices have been through the passage of laws allowing pharmacists to administer vaccines. In doing so, patients are granted access to immunization in situations where there is insufficient access [15].
A qualitative study was performed to analyze CDC vaccination protocol in the United States for individuals traveling to and from polio circulating countries. Before traveling to a country at risk for poliovirus, CDC states that all travelers should ensure that they have received the age appropriate dosage of poliovirus vaccine. Being a mandatory vaccine for infants and children in the US, it is essential that IPV is administered at ages 2, 4, and a final dosage at an age later than 4 after 6 months of a previous dosage. However, in events that an infant or child is at risk for travel to a region of poliovirus circulation, an accelerated schedule can be used in which the first dosage is given to infants at an age greater than 6 weeks and is followed by the second and third dosage after 4 weeks of the first. As such, there are also vaccination protocols to be followed by adults who are planning to travel to such places as well. For adults, 2 doses should be given in intervals between 4-8 weeks and a third dosage should be administered 6-12 months after the second. However, in circumstances where time does not permit for regular administration, vaccination can be given specific to the allotted time frame. If there are greater than 8 weeks before the set travel date, 3 doses of IPV can be given 4 weeks apart. However, if there are less than 8 weeks, but greater than 4 weeks, 2 doses of IPV are administered 4 weeks apart. Moreover, if less than 4 weeks are available, a single dosage of IPV is recommended. Furthermore, the US has strict laws in place for residents of countries with polio wanting to visit. In order to depart from their homeland, proof of vaccination is required between 4 weeks and 12 months before the date of departure [16].
A cross sectional study was performed in Nigeria following the identification of a nomadic population migrating to Nigeria from outside the international border. The purpose of the study was to collect entry and exit points from nomadic pastoralists, resting points, and health-seeking behaviors via informant interviews and questionnaires. Upon collecting the information, vaccination teams provided groups amongst the identified routes with OPV from February to April 2016 [17].
The study allowed 2015 children under the age of 5 to be vaccinated in February with OPV. However, of these 2015 children, 264 had never received a dosage of the vaccine. Moreover, in March, 1864 children received the vaccination, of which 211 had never received a dosage. The study concluded that there is a need for policies amongst transboundary population especially in people such as nomadic pastoralists [17].
Discussion
Implementing educational based programs
A common cause of vaccination denial in endemic countries of poliomyelitis is a lack of knowledge and acceptance of misconceptions about the vaccines. For instance, in Pakistan’s Khyber Pakhtunkhwa Province, as informed in Murakami’s study, “the local interpretations (perceptions that OPV contained birth control or pork, that OPV was a foreign/central plot against Muslims, and that vaccination was against the Hadith and the fate determined by god)” shows the need for the implementation of an educational system which serves to not only debunk the rumored beliefs of local naysayers, but also serves to educate the importance of vaccination practices.
Utilizing practices that have worked in the United States for educational issues, one method to educate the local population of these endemic regions can be done via the usage of physicians.
As found in Chung’s study, parents who were hesitant to get vaccinations for their children were persuaded to do so when educated by a physician. Moreover, the study found that parents who were reluctant to vaccinate their children are more likely to surround themselves with parents of similar belief. Hence, implementing an educational program not only assists in convincing one parent to vaccinate, but indirectly leads to the breakthrough of a social circle’s point of view on vaccines spreading the usage of vaccination.
Another way of implementing an educational program is via the usage of media. As seen in the study done by Shah, journalists are vital in spreading information about polio vaccination especially in areas that may be hard to reach or that show a resistance to the usage of vaccinations. However, journalists themselves are not completely educated in the topics of vaccination, thus having a physician educate them via an interview can help information reach these resistant areas and for journalists to convey accurate information to endemic regions themselves.
A final way to implement educational based programs is to focus on the diverse concerns of the region. For instance, people of Pakistan may have different concerns as opposed to people in Nigeria, especially on sensitive topics such as religion. As such, implementing educational programs unique to population concerns can show a change in vaccination programs. As concluded in Greenfield’s study, targeting physicians based on ethnicity to educate their respective demographic helps to break down both cultural and religious concerns for vaccination practices. Moreover, the study also verified that parents are likely to change their respective views on vaccination if educated by physicians.
Implementing a change in method of vaccination administration
Aside from wild type poliovirus causing poliomyelitis in endemic countries, another concern is circulating vaccine derived poliovirus type 2 (cVDPV2). This is seen in all endemic countries and is a cause of concern due to the method of administrating the polio vaccination orally. Moreover, cVDPV2 becomes a larger concern in these endemic countries because they have low immunization rates for polio prophylaxis, putting the population at a higher risk for contracting the virus from unsanitary conditions. Thus, a change in the method of vaccination from the oral vaccine to the injected, inactivated vaccination should be implemented.
As informed by Wallace, “since 2000, the United States has exclusively used IPV, resulting in prevention of 8-10 vaccine-associated paralytic poliomyelitis cases annually.” A country such as the United States, in which vaccination is readily accessible and herd immunity is much greater than the endemic countries utilizes the IPV over OPV, it is imperative to implement this change in Nigeria, Pakistan, and Afghanistan. As shown by Iqbal, adverse effects of implementing an inactivated poliovirus vaccine are minimal making it safe to be utilized with other childhood vaccinations. Furthermore, when given without other vaccinations, Iqbal reported that IPV shows minimal to no adverse effects.
Further proof of implementing a vaccination change from OPV to IPV can be seen in the study from Saleem. The study shows that adding a dosage of IPV to trivalent or monovalent OPV not only helps to elicit a stronger immune response within the receiver, but also decreases the shedding of poliovirus in fecal matter. Moreover, Jenkins shows in his study that paralysis caused by cVDPV has no significant difference in clinical severity when compared to paralysis contracted by a strain of wild polio virus. In addition, Jenkins illustrates that prophylaxis by OPV is lower in type 1 and type WPV than is in the already eradicated type 2 WPV. For these reasons, implementing the usage of IPV is more beneficial than OPV, as it not only reduces the risk of cVDPV, but also raises immunity within the population.
Implementing law mandated programs for vaccination
The last set of implementation is that endemic countries can utilize from the United States are mandatory vaccination laws and procedures. Applying laws not only help to eradicate polio, but also help to contain possibilities of breakouts. One such method to implement successful laws is through educational institutes. As proven in Barraza’s study, each state has a set of unique laws in place, which help to protect the residents of the state. For instance, the state of California implementing vaccination laws, making it mandatory for parents to vaccinate their children irrespective of their personal or religious beliefs can be utilized in regions found in Pakistan and Afghanistan, where vaccination practices are nullified from disproven information based on religious beliefs. Moreover, as shown in Barraza’s study, to guarantee that laws are followed, protocols such as failure to enroll an unvaccinated child in school can be mandated. Furthermore, passing laws allowing more healthcare workers to administer vaccinations as the US has done, allows for greater access to vaccinations. These are especially important for populations that are consistently migrating through transboundaries of countries such as Nigeria, as shown in Bawa’s study. To further provide vaccination, laws targeting travelers to and from endemic regions can be implemented. As informed by Wallace, the CDC has set strict guidelines for residents of the United States for receiving vaccination for polio before traveling to any countries in the world in which contracting poliovirus is a possibility. These guidelines are set for every case unique to the duration of the time a traveler may have before their departure, for the amount of time planned to reside in their destination, and the age of the traveler. Moreover, as shown by Wallace, in order for an individual to visit the United States from a country where poliovirus is a possibility, proper immunization records must be provided for entry into the country. Hence, endemic countries implementing strict policies and procedures for vaccination as the United States has done not only helps to increase vaccination practices, but helps to decrease the spread of disease to other countries that have already successfully eradicated the virus.
Future Directions
Eradication of polio in the endemic countries of Afghanistan, Pakistan, and Nigeria is difficult due to the unique challenges presented within each country. Moreover, due to the rising cases of both wild type poliovirus and circulating vaccine derived poliovirus since 2015, it is imperative that new methods are tried. As such, the methods proposed in this paper can play a vital role in not only preventing cases, but also ridding the poliovirus within the world. Furthermore, the rising cases of poliovirus in these endemic countries show not only the lack of vaccination, but the lack of herd immunity when it comes to the disease. Thus, promoting these newly implemented methods can be useful in tackling both these issues. For instance, various studies presented in this paper have supported higher vaccination practices by parents when educated by a physician. When vaccinating a child, the parents build herd immunity in their social circle by decreasing the number of hosts available for a virus. In addition, future vaccination practices of other parents in the social circle may also change as they personally experience a child who had no adverse effects to vaccination. Furthermore, implementing laws to set strict vaccination schedules also leads to an increase in herd immunity as children are attending schools and daycares with up to date immunizations. Moreover, when educating parents on accurate vaccination practices, it builds a more trustful and compliant patient-physician relationship. Lastly, the Global Polio Initiative has shown that although their hard work has paid off in the majority of the world, their consistent struggle to rid these endemic countries of the illness requires a change in approach. Hence, implementing the proven methods proposed in this paper are vital to bringing a fresh approach to solving an age old crisis. If implemented correctly, it is a firm belief that the future of the world can be one with the poliovirus a thing of the past as seen with many vaccine preventable disorders of the past.
Limitations of research
The research provided in this paper focuses on major issues faced by endemic countries preventing vaccination practices for polio. However, the limitation to these researched programs is seen in how the United States dealt with similar issues via law policies, vaccination methods, and education. It does not take into account issues such as instability by war and terrorism faced commonly by countries such as Afghanistan and Pakistan. These lead to difficulty in providing the general population with vaccination and a further spread of disease via a decrease in immunity.
Conclusion
The proposed implementations seen in this paper have proved to be vital in the successful eradication of polio in the United States. As such, it is imperative that these practices are utilized in the endemic countries to build awareness and raise vaccination practices so that polio is eradicated worldwide. Moreover, implementing the proposed practices can lead to a rise in vaccination practices for other disorders as the goal of raising awareness in these developing countries is successfully utilized as hypothesized.
References
- Whatever happened to Polio?-Timeline (n.d.) Smithsonian National Museum of American History. Retrieved from https://amhistory.si.edu/polio/timeline/index.htm
- Our mission (n.d.) Global Polio Eradication Initiative. Retrieved from http://polioeradication.org/who-we-are/our-mission/
- 10 facts on polio eradication (2017) World Health Organization. Retrieved from https://www.who.int/features/factfiles/polio/en/
- What is Polio? (2017) Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/polio/about/index.htm
- Pakistan (n.d.) Global Polio Eradication Initiative. Retrieved from http://polioeradication.org/where-we-work/pakistan/
- Nigeria (n.d.) Global Polio Eradication Initiative. Retrieved from http://polioeradication.org/where-we-work/nigeria/
- What is vaccine-derived polio? (2017) World Health Organization. Retrieved from https://www.who.int/features/qa/64/en/
- Chung Y, Schamel J, Fisher A, Frew PM (2017) Influences on immunization decision-making among US parents of young children. Matern Child Health J 21: 2178-87.
- Shah SFA, Ginossar T, Weiss D (2019) This is a pakhtun disease: pakhtun health journalists’ perceptions of the barriers and facilitators to polio vaccine acceptance among the high-risk pakhtun community in Pakistan. Vaccine 37: 3694-703.
- Greenfield LS, Page LC, Kay M, Li-Vollmer M, Breuner CC, et al. (2015) Strategies for increasing adolescent immunizations in diverse ethnic communities. J Adolesc Health 56: S47-53.
- Murakami H, Kobayashi M, Hachiya M, Khan ZS, Hassan SQ, et al. (2014) Refusal of oral polio vaccine in northwestern Pakistan: a qualitative and quantitative study. Vaccine 32:1382-7.
- Iqbal S, Shi J, Seib K, Lewis P, Moro PL, et al. (2015) Preparation for global introduction of inactivated poliovirus vaccine: safety evidence from the US vaccine adverse event reporting system, 2000-12. Lancet Infec Dis 15:1175-82.
- Saleem AF, Yousafzai MT, Mach O, Khan A, Quadri F, et al. (2018) Evaluation of vaccine derived poliovirus type 2 outbreak response options: A randomized controlled trial, Karachi, Pakistan. Vaccine 36:1766-71.
- Jenkins HE, Aylward RB, Gasasira A, Donnelly CA, Mwanza M, et al. (2010) Implications of a circulating vaccine-derived poliovirus in Nigeria. New England J Med 362: 2360-9.
- Barraza L, Schmit C, Hoss A (2017) The latest in vaccine policies: selected issues in school vaccinations, healthcare worker vaccinations, and pharmacist vaccination authority laws. J Law Med Ethics 45: 16-9.
- Wallace GS, Seward JF, Pallansch MA (2014) Interim CDC guidance for polio vaccination for travel to and from countries affected by wild poliovirus. MMWR Morb Mortal Wkly Rep 63:591-4.
- Bawa S, Afolabi M, Abdelrahim K, Abba G, Ningi A, et al. (2018) Transboundary nomadic population movement: a potential for import-export of poliovirus. BMC Pub Health 18:13-6.