Heather L Schmidtknecht*
Department of Nursing, Winona State University, Winona, MN, USA
*Corresponding Author:
Heather L Schmidtknecht
Assistant Professor
Department of Nursing
Winona State University
Winona, MN 55987, USA
Tel: 5074299985
E-mail: hschmidtknecht@winona.edu
Received Date: October 05, 2017; Accepted Date: October 11, 2017; Published Date: October 18, 2017
Citation: Schmidtknecht HL (2017) Increasing Colorectal Cancer Screening Uptake in Patients:Provider-Initiated Discussion at Every Primary Care Patient Encounter. J Healthc Commun. 2:70. doi: 10.4172/2472-1654.100111
Keywords
Colorectal cancer; Primary care; Cancer screening; Immunochemical testing
Introduction
Colorectal cancer killed 51,651 people in the United States in 2014 [1], despite this type of cancer being almost completely preventable and, if diagnosed in early stages, highly treatable [2]. The U.S. Preventive Services Task Force (USPSTF) currently recommends routine stool-based screening or directvisualization screening for asymptomatic patients at average risk of colorectal cancer, offering an array of screening options to allow patient-centered decision-making [3]. Colorectal cancer screening is recommended for all people 50-75 years of age at specified intervals depending on the type of screening used, as well as the screening results [2]. However, only 58.2% of people in the United States had received appropriate screening based on their age, past screening participation, and the results of past screenings in 2013 [4].
Two common barriers to colorectal cancer screening cited in the research include lack of knowledge about the importance of colorectal cancer screening [5] and lack of provider recommendation for screening [5-7]. To respond to this lack of awareness, resources in the United States have been concentrated on population-based interventions to inform the public of the importance of colorectal cancer screening. As an example, Centers for Disease Control (CDC) launched the Screen for Life: National Colorectal Cancer Action Campaign in 1999, and it is still at work today. This campaign provides multi-media messages about the importance of colorectal screening for everyone between 50-75 years of age. It emphasizes that colorectal cancer does not always cause symptoms, thus making screening especially important to allow for removal of precancerous adenomatous polyps and the diagnosis of colorectal cancer in its earliest stages, when it is most treatable. In addition, it emphasizes that the risk for colorectal cancer increases with age, reinforcing the importance of getting screened at the recommended intervals until age 75, even if initial screening included no abnormal findings. Finally, it provides a guide on how to speak with providers about colorectal cancer screening [8]. Although the population-based interventions discussed above will move forward efforts to increase colorectal cancer screening rates, there is overwhelming evidence that lack of provider recommendation for colorectal screening is a significant barrier to screening uptake [5-7,9-16].
Addressing Barriers for Providers
Provider-level barriers cited in review of the literature include but are not limited to, lack of knowledge of screening recommendations and options for screening other than colonoscopy [3,5,12,13,17]. The U.S. Preventive Services Task Force (USPSTF) currently recommends routine stool-based screening or direct-visualization screening for asymptomatic patients at average risk of colorectal cancer. Stool-based screening is recommended on a yearly basis and options include guaiac-based fecal occult blood tests (gFBOT), fecal immunochemical tests (FIT), or fecal immunochemical testing combined with stool DNA testing (FIT-DNA). Direct-visualization screening recommendations include colonoscopy every 10 years, CT colonography every 5 years, or flexible sigmoidoscopy every 5 years (or every 10 years if combined with annual FIT testing). The USPSTF recommendations intentionally offer an array of screening options to allow patient-centered decision-making [3].
In addition, CDC is working to better inform health care providers and is currently offering Continuing Medical Education (CME) entitled, Screening for Colorectal Cancer: Optimizing Quality [17]. The CME modules review the menu of options for effective colorectal cancer screening, how to decide which option is best for each patient, and the importance of offering patients forms of colorectal cancer screening other than colonoscopy when appropriate, to promote adherence to screening recommendations.
Provider-Initiated Discussion
In current practice, provider-initiated discussion of preventive screening is typically reserved for periodic health examination encounters. Although this is a logical time for discussion of preventive screening, many patients do not schedule periodic health examinations and only present to the primary care clinic for acute illness or chronic illness management. Therefore, a significant number of individuals do not receive these recommendations. In addition, there are individuals who receive colorectal cancer screening recommendations, yet do not follow-through to uptake of actual screening [13]. There are recommendations to increase the quantity and the quality of colorectal screening discussions [12], yet there remains a gap in the literature as to how to elevate practice to this level.
Provider-initiated colorectal cancer screening discussions at every primary care patient encounter results in repeated provider-initiated discussion related to the need for colorectal cancer screening, which projects the importance of this screening recommendation, as well as repeatedly opens a dialogue concerning barriers to follow-through with prior recommendations, as applicable. This practice also increases the quality of colorectal screening discussions, as the provider engages in tailored discussions of the patient’s individual risk level, their previous experiences with screening, and the barriers they face to complete recommended screening. The importance of the patient-provider discussion is widely cited in the literature as a critical factor in decreasing barriers to screening and providing individualized screening recommendations with a high probability of uptake [5-7,12-16].
Putting it all Together
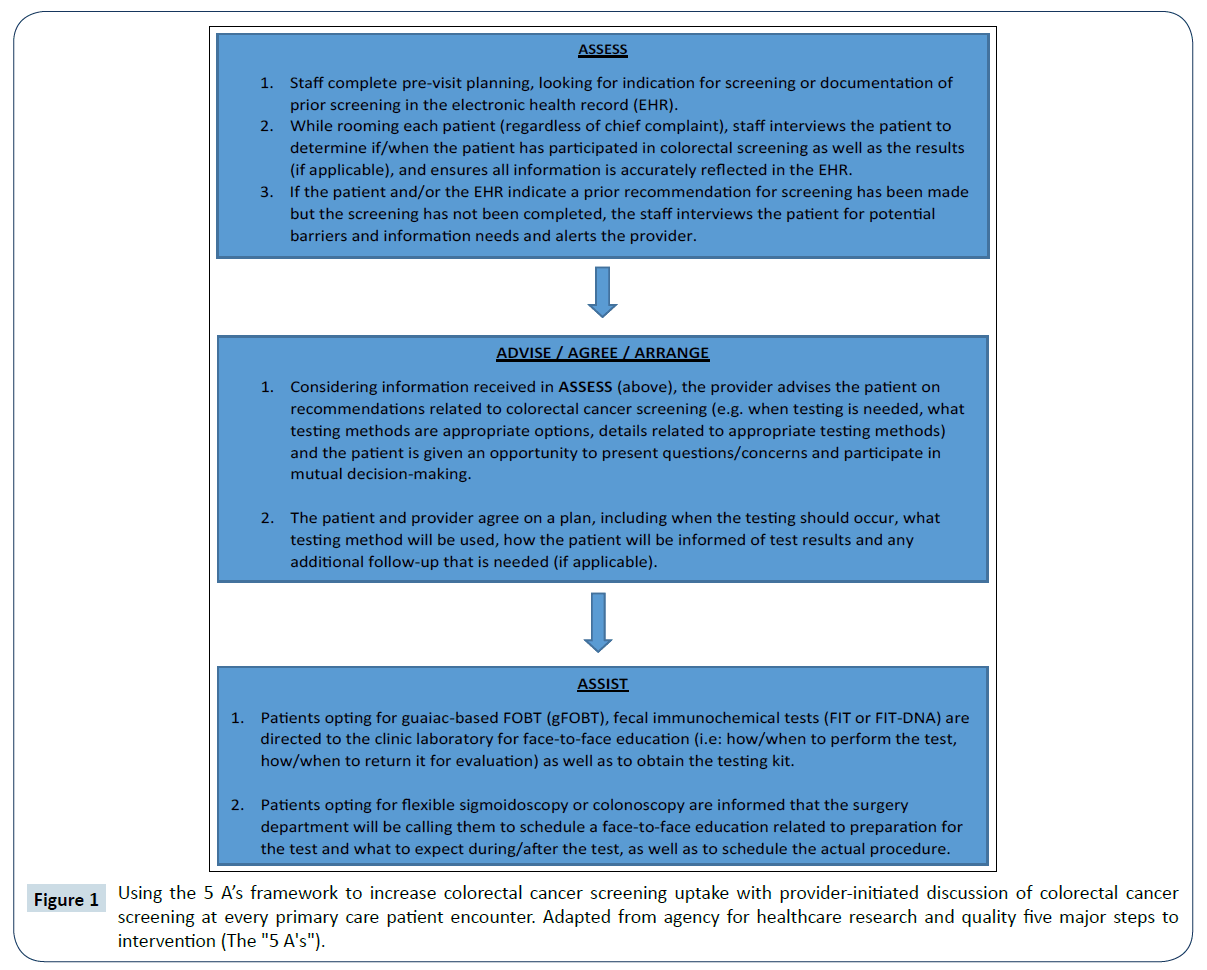
Five Major Steps to Intervention (the "5 A's") is an intervention model previously used by Agency for Healthcare Research and Quality (AHRQ) for use with tobacco cessation [18]. The 5 A’s (assess, advise, agree, assist, and arrange) can be applied to provider-initiated discussion of colorectal cancer screening as depicted in Figure 1. The responsibility for implementation of this intervention model can be shared by the primary care team. The “ASSESS” process begins with pre-visit planning where staff look for indication for screening or documentation of prior screening in the electronic health record (EHR). Next, the staff that is rooming the patient who will interview the patient related to their colorectal screening status and/or experiences at the same time as they are collecting information related to their chief complaint, and current medications. The information collected can be recorded or updated in the EHR, which makes it accessible to the provider. The “ADVISE/AGREE/ARRANGE” process begins as the provider then discusses the information with the patient in an individualized manner to address their specific health status, as well as their particular experiences, questions, and concerns. The provider then makes a patient-specific recommendation for colorectal screening, the patient has an opportunity to pose questions and concerns, and they agree on a plan for colorectal cancer screening. The “ASSIST” process completes the intervention as the logistical information needed to complete colorectal cancer screening as recommended is shared and mutually agreed upon.
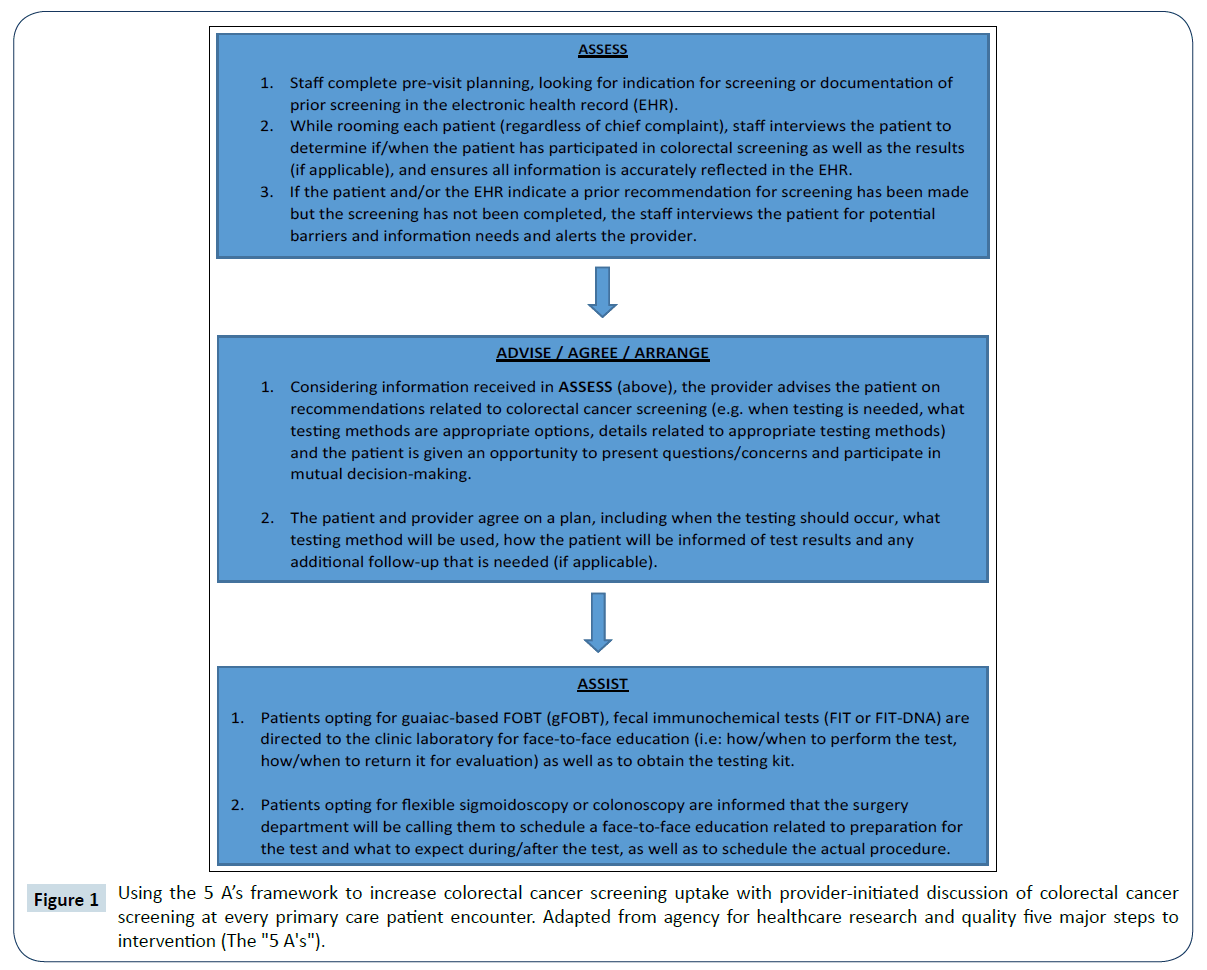
Figure 1: Using the 5 A’s framework to increase colorectal cancer screening uptake with provider-initiated discussion of colorectal cancer screening at every primary care patient encounter. Adapted from agency for healthcare research and quality five major steps to intervention (The "5 A's").
Conclusion
Colorectal cancer continues to cause significant morbidity and mortality in the United States, despite the availability of preventive screening. Although patients have many barriers pertaining to uptake of colorectal cancer screening, most often cited is lack of knowledge and lack of provider recommendation. Population-based interventions are cost-effective ways of increasing the knowledge of the general public. Offering choices on colorectal screening methods and allowing the patient to participate in shared decision-making increases colorectal screening recommendation adherence. Despite these interventions, multiple missed opportunities every day within established primary care practices exist, and can be captured with provider-initiated discussion of colorectal cancer screening recommendations at every primary care patient encounter.
References
- https://www.cdc.gov/uscs.
- Klabunde CN, Joseph DA, King JB, White A, Plescia M (2013) Vital signs: colorectal cancer screening test use—United States, 2012. Morb Mortal Wkly Rep 62: 881-888.
- US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, et al. (2016) Screening for colorectal cancer: US preventive services task force recommendation statement. J Am Med Assoc 315: 2564–2575.
- National Center for Health Statistics (2016) Cancer: Healthy people 2020 midcourse review (Chapter 5). Hyattsville, MD.
- Wang J, Moehring J, Stuhr S, Krug M (2013) Barriers to colorectal cancer screening in Hispanics in the United States: an integrative review. Appl Nurs Res 26: 218-224.
- Holden, DJ, Harris R, Porterfield DS, Jonas DE, Morgan LC, et al. (2010) Enhancing the use and quality of colorectal cancer screening: evidence report/technology assessment (190). Ann Intern Med 52: 668-672.
- Guessous I, Dash C, Lapin P, Doroshenk M, Smith RA, et al. (2010) Colorectal cancer screening barriers and facilitators in older persons. Prev Med 50: 3-10.
- Vital signs: colorectal cancer screening test use—United States, 2012.
- Baron RC, Melillo S, Rimer BK, Coates RJ, Kerner J, et al. (2010) Intervention to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers: a systematic review of provider reminders. Am J Prev Med 38: 110-117.
- Escoffery C, Rodgers KC, Kegler MC, Ayala M, Pinsker E, et al. (2014) A grey literature review of special events for promoting cancer screenings. BMC Cancer 14: 454-468.
- Escoffery C, Rodgers KC, Kegler MC, Haardörfer R, Howard DH, et al. (2014) A systematic review of special events to promote breast, cervical and colorectal cancer screening in the United States. BMC Public Health 14: 274-287.
- Holden DJ, Jonas DE, Porterfield DS, Reuland D, Harris R (2010) Systematic review: enhancing the use and quality of colorectal cancer screening. Ann Intern Med 152: 668-676.
- Meissner HI, Klabunde CN, Breen N, Zapka JM (2012) Breast and colorectal cancer screening: U.S. primary care physicians' reports of barriers. Am J Prevent Med 43: 584-589.
- Powe BD, Faulkenberry R, Harmond L (2010) A review of intervention studies that seek to increase colorectal cancer screening among African Americans. Am J Health Promot 25: 92-99.
- Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, et al. (2012) Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med 43: 97-118.
- Steinwachs D, Allen JD, Barlow WE, Duncan RP, Egede LE, et al. (2010) NIH State-of-the-Science conference statement: enhancing use and quality of colorectal cancer screening. NIH Consens State Sci Statements 27: 1-31.
- https://www.cdc.gov/cancer/colorectal/pdf/sfl_backgrounder.pdf
- https://www.cdc.gov/cancer/colorectal/quality/index.htm#pc