Case Report - (2016) Volume 17, Issue 3
Hiroshi Ohkawara1, Akiko Shichishima-Nakamura1, Kazuhiko Ikeda1,2, Masumi Sukegawa1, Miki Furukawa1, Takahiro Sano1, Koki Ueda1, Satoshi Kimura1, Akiomi Yoshihisa1, Hideyoshi Noji1, Kazuei Ogawa1,Yasuchika Takeishi1
1Department of Cardiology and Hematology, Fukushima Medical University, Fukushima, Japan
2Department of Blood Transfusion and Transplantation Immunology, Fukushima Medical University, Fukushima, Japan
*Corresponding Author:
Hiroshi Ohkawara
Department of Cardiology and Hematology
Fukushima Medical University
1 Hikariga-oka, Fukushima, Fukushima, 960-1295, Japan
Phone +81-24-547-1190
Fax +81-24-548-1821
E-mail ohkawara@fmu.ac.jp
Received January 15th, 2016 – Accepted March 06th, 2016
Context Pancreatic pseudocysts, which are known to be a common complication of chronic pancreatitis, occasionally result in spontaneous intestinal perforation. However, multiple perforations of pancreatic pseudocysts into internal organs are rarely seen. Case report A 46-yearold man was admitted to our hospital complaining of left upper abdominal pain, where a palpable mass was found. Abdominal computed tomography scan showed a large pancreatic pseudocyst in the tail of the pancreas and a splenic artery pseudoaneurysm. The pseudoaneurysm was treated by urgent percutaneous transarterial embolization. Endoscopic examinations revealed fistulas that had ruptured into the stomach and transverse colon. The patient had a high fever with prolonged elevated C-reactive protein. Contaminated fluid/debris was eliminated from the infected pseudocyst cavity under colonoscopy and ileostomy, followed by spontaneous closure of the fistulas. Conclusion This is a rare patient of a ruptured pancreatic pseudocyst in the stomach and colon, complicated by a splenic artery pseudoaneurysm.
Keywords
Colon; Embolization, Therapeutic; Fistula; Pancreatic Pseudocyst; Stomach
INTRODUCTION
Spontaneous ruptures occur in less than 5% of patients with pancreatic pseudocysts, and perforation of the pseudocyst into the surrounding visceral structure is rare [1- 3]. The activation of pancreatic enzymes and the vulnerability of pseudocysts occasionally causes spontaneous perforation into other internal organs, and some patients of spontaneous perforations of the pseudocyst into surrounding organs have been reported [4- 7]. Splenic artery pseudoaneurysm, which occurs as a potentially serious complication of chronic pancreatitis, has also been rarely reported [8- 12]. Herein, we present a rare patient of a large pancreatic pseudocyst communicated with the operative stomach and colon, and this patient was associated with a splenic artery pseudoaneurysm.
CASE REPORT
A Forty-six--year-old man was admitted to our hospital with left upper abdominal pain, where he had found a palpable mass. On examination, a palpable mass was found and he was revealed to develop severe hypotension (systolic blood pressure 64 millimeters of mercury). He had chronic alcohol-related pancreatitis and underwent subtotal gastrectomy for gastric ulcers 16 years previously. Abdominal computed tomography (CT) scan revealed a large pancreatic pseudocyst (12 cm in diameter; Figure 1a) in the tail of the pancreas, and a hemorrhagic splenic artery pseudoaneurysm (4 cm in diameter; Figure 1b). The CT scan also showed air and accumulation of fluid/debris in the pseudocyst cavity, indicating gastrointestinal perforation into the pseudocyst (Figure 1a). Peripheral blood examination showed leukocytosis and anemia, with a white blood cell count of 14.5 × 109/L and hemoglobin level of 65 g/L. Serum biochemical analysis showed low levels of amylase 18 IU/L (normal range: 25–125 IU/L), alkaline phosphatase 245 IU/L (normal range: 44–147 IU/L), and C-reactive protein 17 mg/L.
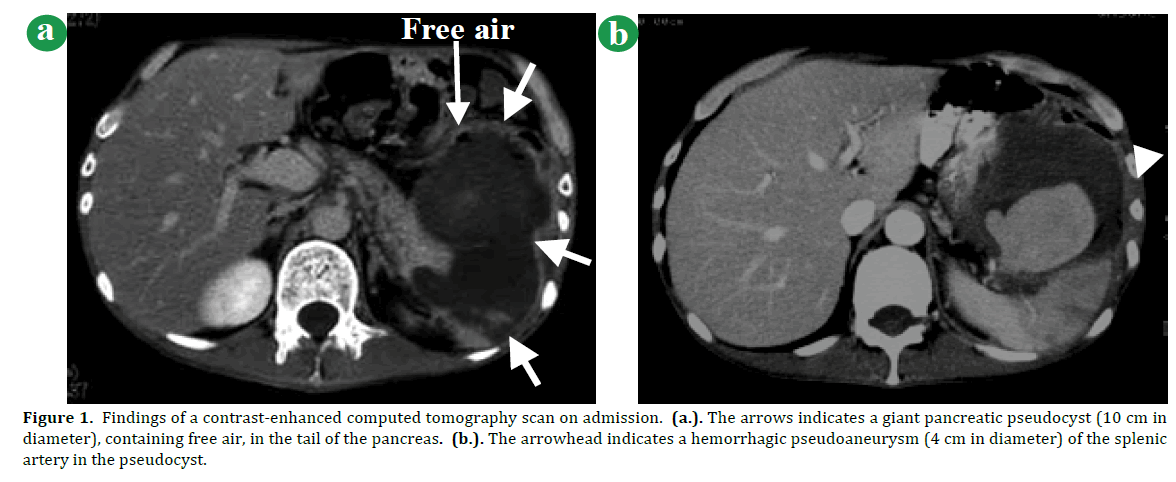
Figure 1. Findings of a contrast-enhanced computed tomography scan on admission. (a.). The arrows indicates a giant pancreatic pseudocyst (10 cm in diameter), containing free air, in the tail of the pancreas. (b.). The arrowhead indicates a hemorrhagic pseudoaneurysm (4 cm in diameter) of the splenic artery in the pseudocyst.
Transarterial embolization with stainless steel coils was performed to treat the ruptured pseudoaneurysm, and the large pseudocyst was subsequently reduced in size. Endoscopic examinations revealed fistulas, which ruptured into both the stomach and transverse colon (Figures 2a,b). Endoscopic retrograde cholangiopancreatography did not reveal any communication between the main pancreatic duct and the pseudocyst (Figure 2c). The patient had a high fever with prolonged elevated C-reactive protein (12 mg/L), indicating an infected pancreatic pseudocyst. The colonoscope, which was similar in diameter to the colonic fistula, was inserted into the pseudocyst cavity through the colonic fistula into the operative stomach (Figure 2d), and a potential refractory infection aggravated by fecal contamination in the pseudocyst cavity was observed under colonoscopy (Figure 2b).
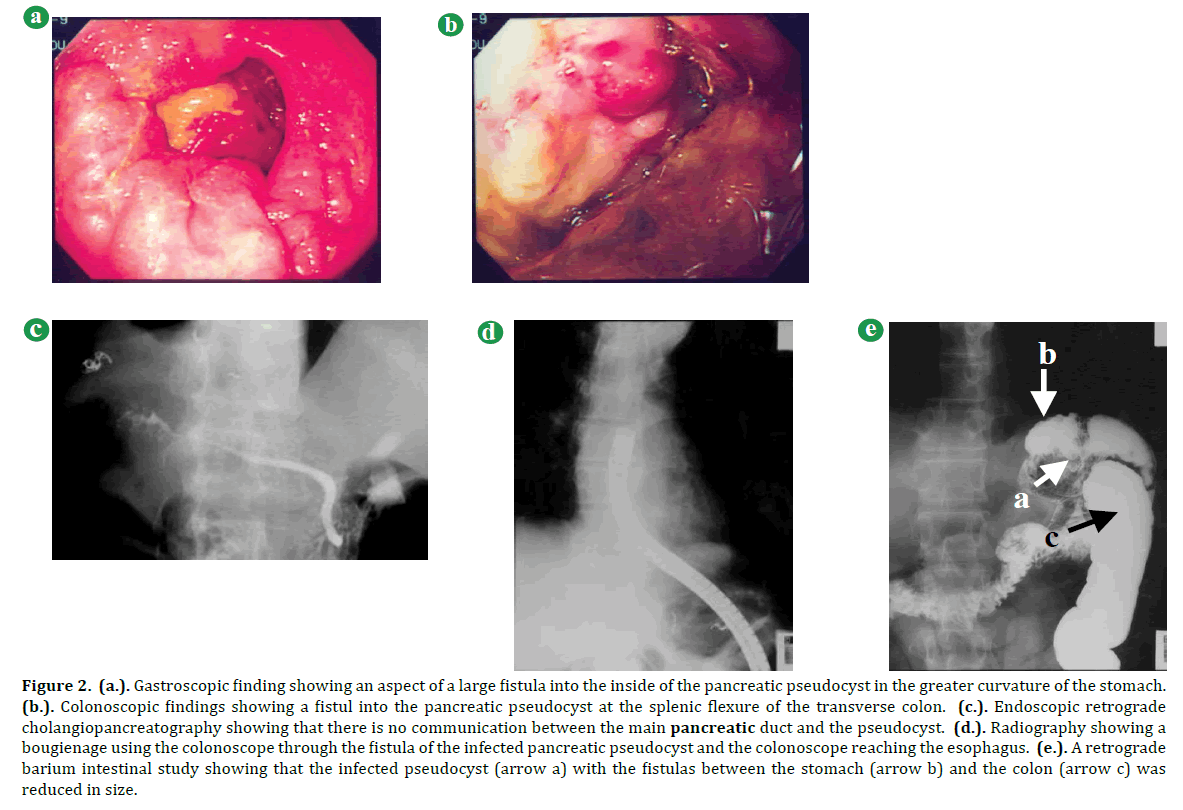
Figure 2. (a.). Gastroscopic finding showing an aspect of a large fistula into the inside of the pancreatic pseudocyst in the greater curvature of the stomach. (b.). Colonoscopic findings showing a fistul into the pancreatic pseudocyst at the splenic flexure of the transverse colon. (c.). Endoscopic retrograde cholangiopancreatography showing that there is no communication between the main pancreatic duct and the pseudocyst. (d.). Radiography showing a bougienage using the colonoscope through the fistula of the infected pancreatic pseudocyst and the colonoscope reaching the esophagus. (e.). A retrograde barium intestinal study showing that the infected pseudocyst (arrow a) with the fistulas between the stomach (arrow b) and the colon (arrow c) was reduced in size.
We eliminated the contaminated fluid/debris in the pseudocyst and cleaned the infected cavity with a saline solution. Subsequently, the size of the pseudocyst was reduced, and the serious infection in the cavity was improved. Retrograde barium intestinal study showed that the size of the pseudocyst was markedly reduced (Figure 2e). The patient underwent an ileostomy, after that the fistulas closed spontaneously and the ileectomy reversed.
Finally, the patient maintained an asymptomatic state, and follow-up CT scans showed no sign of recurrence over a nine-year follow-up period (Figures 3ab).
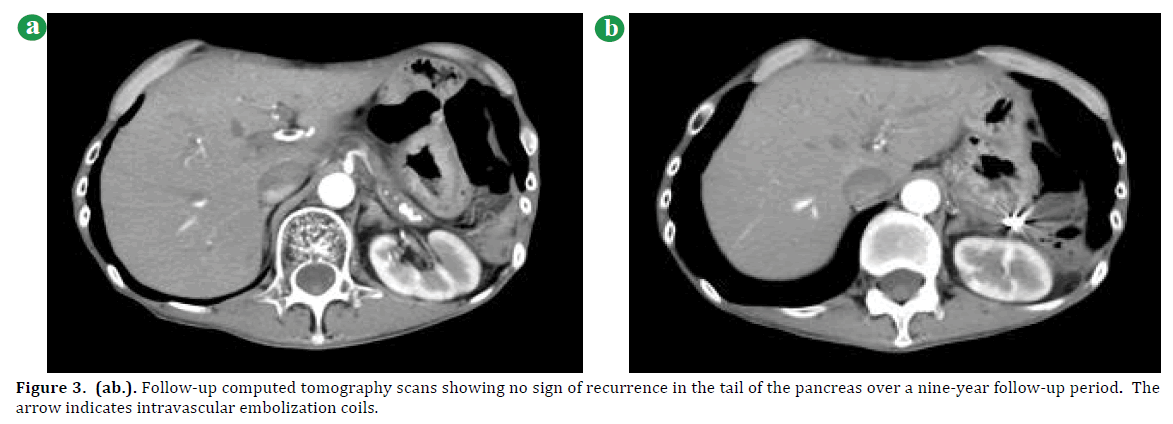
Figure 3. (ab.). Follow-up computed tomography scans showing no sign of recurrence in the tail of the pancreas over a nine-year follow-up period. The arrow indicates intravascular embolization coils.
DISCUSSION
Pancreatic enzymes and cytokines activated by chronic pancreatitis induce pseudocyst formation, potentially resulting in spontaneous perforation into the surrounding hollow viscera [13, 14]. Endoscopic therapies such as transmural or transpapillary drainage and surgical procedures are useful for the treatment of pancreatic pseudocysts [15- 18]. Fistulization of pancreatic pseudocysts into surrounding viscera usually requires surgical treatment [17- 20]. It has been reported that an infected pancreatic pseudocyst with a colonic fistula can be treated successfully with a combination of endoscopic drainage and antibiotics [21]. Splenic artery pseudoaneurysm, which is a complication of chronic pancreatitis or trauma, is rarely seen and surgical or endovascular treatment of the pseudoaneurysm is usually required [9- 11]. A pseudoaneurysm is caused either by enzymatic activation of peripancreatic arteries or erosion of a visceral artery by a pancreatic pseudocyst [14, 22].
To our knowledge, this is the first reported patient of a pancreatic pseudocyst fistulized into two hollow viscera associated with a splenic artery pseudoaneurysm. In this patient, enzymatic activation due to worsening pancreatitis and extrinsic compression of the enlarged pseudoaneurysm may potentially induce spontaneous perforations. Since fecal contamination can result in serious infection or hemorrhage, rupture of a pancreatic pseudocyst into the colon generally requires operative intervention [19, 20]. In this patient, the remaining fluid/debris in the pseudocyst indicated a refractory infection aggravated by fecal contamination, and the elimination of the contaminated fluid/debris under colonoscopy and ileostomy was effective for the treatment of the infected pseudocyst cavity.
In conclusion, we described a rare patient with a large pancreatic pseudocyst that ruptured into the stomach and colon, complicated by the hemorrhagic splenic artery pseudoaneurysm. The patient was recovered from severe bleeding resulting from the artery pseudoaneurysm with urgent transarterial embolization, and that the infected pseudocyst with fistulas closed spontaneously after an ileostomy.
Conflict of Interest
The authors declare no conflict of interest.