- (2011) Volume 12, Issue 4
James L Buxbaum1, Scott W Biggins2, Karen C Bagatelos3, John M Inadomi4, James W Ostroff3
1Division of Gastrointestinal and Liver Diseases, University of Southern California, Keck School of Medicine. Los Angeles, CA, USA
2Division of Gastroenterology and Hepatology, University of Colorado Denver Health Sciences Center. Aurora, CO, USA
3Division of Gastroenterology and Hepatology, University of California - San Francisco. San Francisco, CA, USA.
4Division of Gastroenterology, University of Washington. Seattle, WA, USA
Received March 7th, 2011 - Accepted April 20th, 2011
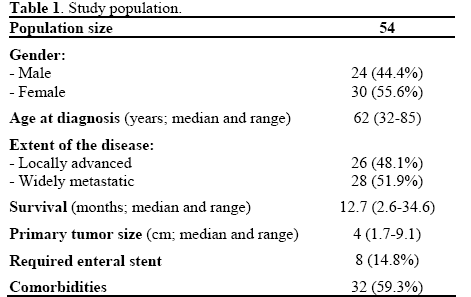
Context Endoscopically placed metal stents, which are patent for 4-9 months, have been the favored decompressive strategy for biliary obstruction due to inoperable pancreatic cancer in order to minimize interventions. However, in the past decade chemotherapeutic options have improved survival. This raises the question of whether metal stents will continue to be the optimal method of decompression. Objective We performed a study to determine the outcome of patients with non-operatively managed pancreatic adenocarcinoma with regards to the development of cholangitis. Design We reviewed all ERCP performed for malignant distal biliary obstruction in between December 1999 and December 2005 at University of California, San Francisco (UCSF). Patients Only patients who received chemotherapy for pancreatic adenocarcinoma were included. Patients who underwent surgical biliary diversion procedures were excluded. Primary outcome measurement The primary outcome was the development of cholangitis requiring hospitalization. Results Among 200 patients with malignant distal biliary obstruction who underwent endoscopic biliary decompression procedures, 54 met study criterion. Metal stents were employed in 90.7% of these cases. The median survival of this population was 12.7 months (range: 2.6-34.6 months). Only 3 of 26 patients (11.5%) surviving one year or less developed cholangitis compared to 13 of 28 (46.5%) who survived more than one year. Thus patients surviving greater than one year had a five fold increase in the odds of developing cholangitis (odds ratio: 4.92; P=0.017). Conclusions This cohort of inoperable pancreatic cancer patients undergoing chemotherapy survived longer than the expected patent period of metal stents employed for biliary decompression. The occurrence of cholangitis requiring hospitalization does increase markedly among long term survivors.
Cholangitis; Cholestasis, Extrahepatic; Pancreatic Neoplasms; Stents
During the past ten years chemotherapy for advanced pancreatic cancer has significantly improved [1]. Prior to the introduction of gemcitabine less than 5% of patients survived to one year, following its introduction in the mid-late 1990’s the percentage increased to nearly 20% [2]. Recent studies indicate that the addition of other agents such as the epidermal growth factor receptor, erlotinib, further improves survival [3]. Administration of gemcitabine at a fixed dose rate to optimize the pharmacokinetics of this agent adds additional benefit and improves median survival to 8 months in patients with advanced pancreatic cancer [4]. Many patients with advanced pancreatic cancer are involved in trials with gemcitabine in combination with erlotinib, platinum agents, radiation therapy, and promising new agents such as bevacizumab and cetuximab. The median survival of patients at our center (UCSF) with locally advanced disease treated with gemcitabine (at a fixed dose rate) and cisplatin followed by consolidative chemoradiation is 13.5 months [5].
Biliary obstruction occurs in 70-90% of patients with advanced pancreatic cancer [6]. Endoscopic management of obstruction has lower morbidity and mortality than bypass surgery and percutaneous drainage [7, 8, 9]. Previous studies, as well as a metaanalysis of their findings, suggest that metal stents have improved patency but similar rates of therapeutic success and complications compared to plastic stents [6, 10, 11, 12, 13, 14]. Metal stents were also cost effective, particularly when used in patients without hepatic metastasis and with a tumor size of less than 3cm [15].
However, the majority of these studies were performed in the pre-gemcitabine era and the median survival ranges from 3-6 months, less than current survival estimates, and less than the associated median patency of expandable metal stents. The survival of patients treated with modern chemotherapy for advanced pancreatic cancer is improving and approaching the limits of the efficacious period of metal stents. This study considers the implications of prolonged survival on the management of biliary obstruction in this group with regards to the development of cholangitis.
In this retrospective study, we consecutively reviewed all patients who underwent ERCP at the University Hospital at the University of California, San Francisco, with the purpose of relieving biliary obstruction due to biopsy confirmed pancreatic adenocarcinoma. Patients who were treated between December 1999 and December 2005 were reviewed. Follow up to time of death or for at least two years for all long term survivors was obtained.
Patients who underwent a Whipple procedure or an operative choledochoenteral bypass prior to endoscopic intervention were excluded. Only patients who exclusively underwent chemotherapy or chemotherapy and radiation for their malignancy were included. Baseline demographic variables included the patient’s sex, age at diagnosis, and medical comorbidities including diabetes mellitus. Additionally, features of the tumor such as size and whether it was widely metastatic or locally advanced were considered. The endoscopic management and chemotherapy regimen of each patient was analyzed in detail. Endoscopic interventions included the placement of a removable 10 French, 9 centimeter Cotton-Leung® plastic biliary stent (Cook Medical, Bloomington, IN, USA) or Zilver® 30 french, 8 centimeter uncovered, expandable metal biliary stent (Cook Medical, Bloomington IN). Percutaneous drainage procedures were also assessed when performed after a failed endoscopic intervention in this group.
We took a special interest in those patients who developed cholangitis requiring hospital admission. This endpoint was particularly significant in this group because it required a postponement or discontinuation of chemotherapy. Cholangitis was defined as jaundice, fever (temperature greater than 38.5 degrees centigrade), and abdominal pain or two of these three elements combined with radiographic evidence of biliary obstruction (computed tomography or ultrasound examination) and evidence of abnormal liver tests and elevated inflammatory markers [16]. Complications of the endoscopic procedures including bleeding, perforation, and pancreatitis were also analyzed.
Prior the initiation of the study the UCSF Institutional Review Board granted a waiver of consent. Given the retrospective design and the nature of pancreas adenocarcinoma most of the study subjects had already passed away at the time of the study, information was strictly coded to protect confidentiality, and the risk to study subjects was minimal. The study protocol was fully in compliance with the ethical guidelines for research involving human subjects set forth by the World Medical Association in Helsinki in 1964 and revised in Tokyo in 2004.
Frequencies, as well as mean±SE and median and interquartile range (IQR) and range were used as descriptive statistics. Univariate logistic regressions were performed to determine whether survival, age, sex, comorbidities, tumor size, extent, and requirement for enteral stent predicted the development of cholangitis. We also examined the association between survival time and development of cholangitis using multivariate logistic regression analysis, adjusting for the presence of significant potential covariates revealed in the univariate analyses. Odds ratio and 95% confidence intervals (95% CI) were computed. An unpaired t-test was used to assess whether individuals who developed cholangitis required more procedures for the management of biliary obstruction compared to those who did not and to assess whether the duration of hospitalizations for cholangitis associated with metal stents was different from that associated with plastic stents. Computation was performed using STATA® software (College Station, TX, USA). Two-tailed P values less that 0.05 were considered significant.
Population
Among the 200 patients with malignant distal biliary obstruction 155 (77.5%) were confirmed to have adenocarcinoma, the remainder whom had other malignant tumors including pancreatic neuroendocrine neoplasms, ampullary carcinoma, and distal cholangiocarcinoma were excluded. Of the 155 patients with adenocarcinoma, 54 (34.8%) were treated with contemporary chemotherapy, 19 (12.3%) were excluded because they underwent palliative biliary diversion surgery, and the remainder 82 (52.9%) declined chemotherapy or did not follow up with the endoscopy, oncology, or other services of the university after initial stent placement. The median age at diagnosis of this group of 54 patients was 62 years (interquartile range, IQR: 56-75 years) and the median survival was 12.7 months (IQR: 5.7-16.5 months) from the time of diagnosis (Table 1). The study population was divided evenly between those who had locally advanced (26, 48.1%) and widely metastatic (28, 51.9%) tumor involvement (Table 1). The median and mean survival of patients with locally advanced disease were 15.2 and 15.8 months, respectively while the median and mean survival of those with metastatic disease were 7.6 and 10.4 months, respectively. ERCP with stent placement to achieve biliary decompression was performed a median of 1.7 months (IQR: 0.8-4.3 months) after diagnosis. Cardiac, pulmonary, endocrine, and other major comorbidities were found in 32 (59.3%) of these patients, with 11 (20.4%) of all patients having diabetes mellitus.
Endoscopic Management, Complications, and Chemotherapy
Decompression was initially achieved by endoscopic stenting in 50 (92.6%) of patients. Percutaneous decompression was initially performed in the remaining 4 patients; they subsequently underwent rendezvous procedures to enable endoscopic management. Frequently, patients had a plastic biliary stent placed while they underwent diagnostic workup and were considered for surgical resection. This stent was often replaced with a metal stent after the diagnosis of unresectable tumor was confirmed. The duration of the evaluation process was 1 to 4 weeks. In total 49 (90.7%) of the cohort had metal stents placed at some point in their management course, of whom 40 patients (74.1% of the total cohort) had a metal stent placed within 4 weeks; the remainder 5 (9.3%) were managed strictly with plastic stents.
Plastic stents were changed prophylactically every 3 months or exchanged for metal stents. The endoscopic placement of metal or plastic stents was performed to relieve obstructed metal stents. Percutaneous decompression was performed when endoscopic management of the obstructed stent was unsuccessful.
In total 134 ERCP were performed in this group in order to manage biliary obstruction and enable chemotherapy. There were two complications (3.7%), one episode of pancreatitis (1.9%) and one episode of post sphincterotomy bleeding (1.9%), both following the placement of metal stents. These complications were managed medically and the patients were able to continue their chemotherapy course without interruption. All of the patients underwent contemporary chemotherapy, most as part of clinical trials employing gemcitabine (n=48, 88.9%) given in combination with cisplatin (n=39, 72.2%), capecitabine (n=1; 1.9%), or alone 8 (14.8%). Nine (16.7%) patients who were able to complete six 28-day cycles of fixed dose gemcitabine combined with cisplatin subsequently underwent radiation therapy potentiated with capecitabine. Among the 39 patients who were treated with combined gemcitabine and cisplatin, 25 (64.1%) were treated with one or more additional agents including bevacizumab, capecitabine, docetaxel, irinotecan, oxaliplatin, cetuximab, and erlotinib. The 6 patients who did not receive gemcitabine were treated with capecitabine as a single agent.
Development of Cholangitis
Sixteen (29.6%) of the patients developed cholangitis which required hospitalization. The median total time of hospitalization for these patients was 8 days (IQR: 5-11 days), in some cases this reflected multiple shorter inpatient stays. Patients who developed cholangitis required a mean of 3.9±0.7 procedures (±SE) whereas those who did not develop cholangitis required 1.7±0.2 procedures (P<0.001).
In univariate analyses survival duration and tumor size were associated with the development of cholangitis (Table 2). Survival greater than one year was associated with a five-fold increase in the risk of development of cholangitis. In the multivariate logistic regression analysis controlling for age, sex, comorbidities, tumor size, tumor extent, and requirement for enteral stent, survival greater than one year was associated with a significantly increased risk of cholangitis. In the univariate and multivariate analysis, the odds of cholangitis decreased by half for each centimeter increase in tumor size. There was a trend toward, but no statistically significant difference, in the proportion of patients who developed cholangitis with locally advanced (9/26; 34.6%) versus metastatic disease (7/28; 25.0%). Age, gender, the presence of comorbidities, or the requirement for an enteral stent, were also not predictive of the development of cholangitis.
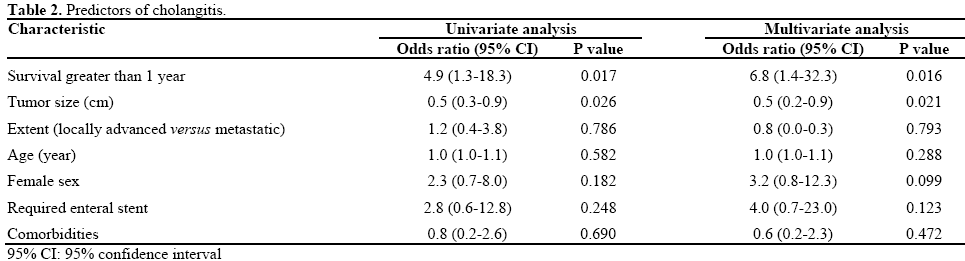
Only three out of 26 patients surviving less than one year developed cholangitis (11.5%) while nearly one half (13/28, 46.4%) of patients surviving longer than one year developed cholangitis (Figure 1). As noted previously most patients were managed with the placement of metal biliary stents. The length of hospitalization for cholangitis associated with metal stents was 6.5±1.0 days (mean±SE) versus 4.9±0.5 days for cholangitis associated with plastic stents (P=0.342).
Figure 1. The number of patients who survived for each particular duration in months is depicted. Those who developed cholangitis are represented with darkened boxes, those who did not develop cholangitis are represented with horizontally lined boxes. Patients with a survival greater than 12 months had a higher rate of developing cholangitis compared to those who survived less than 12 months (P=0.017).
The intent of this study was to critically evaluate the endoscopic management of biliary obstruction in inoperable pancreatic cancer patients receiving contemporary chemotherapy. This group of patients, the majority receiving optimally dosed gemcitabine combined with other agents, demonstrated a median survival of greater than one year. In most cases biliary obstruction was managed by permanent self expandable metal stents. Stent related cholangitis was closely correlated with longer survival and required complex management involving additional procedures and significant periods of hospitalization.
In prior studies evaluating the endoscopic therapy of malignant biliary obstruction, the median survival ranged from 4.5-15.1 months (Table 3). Most of these studies did not report the use of chemotherapy and most included patients with tumors other than adenocarcinoma of the pancreas [10, 11, 12, 13 14, 17, 18, 19, 20, 21, 22]. Among studies in which the majority of subjects had pancreas cancer the longest reported median survival was 11 months. The median survival in our study, 12.7 months, exceeds that in the endoscopic literature but is consistent with improved survival recently reported in patients receiving combination chemotherapy [23, 24].
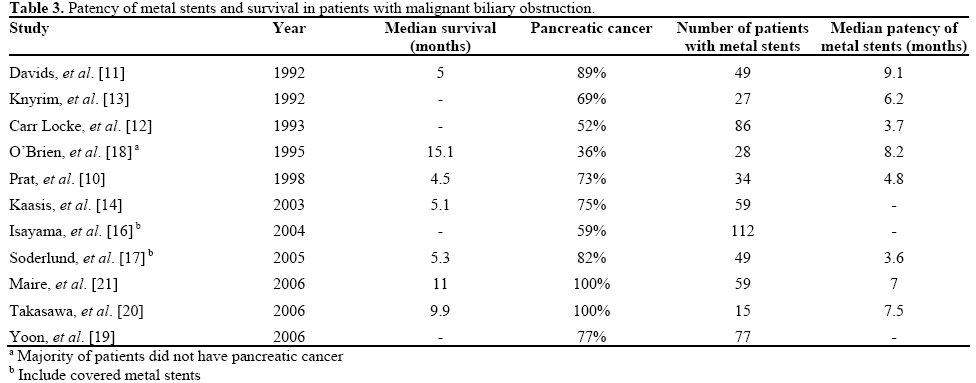
In patients with inoperable pancreatic cancer the current strategy is to manage biliary obstruction with metal stents. Major studies of the management of malignant biliary obstruction have demonstrated that the median patency of metal stents ranged from 3.6 to 9.1 months (Table 3). The median patency of metal stents in all of the studies, weighted by the relative number of patients, was 5.8 months. Most of our patients were initially managed with metal stents. Consistent with the literature, few of them had problems associated with metal stents during the first 12 months of survival.
However, we observed that after 12 months, far beyond the patency range of metal stents, there was an increase in the development of cholangitis. This result remained significant after adjusting for potential confounders. Patients who developed cholangitis required a two fold increase in the number of endoscopic procedures required to maintain a decompressed biliary system and generally more than one week of inpatient management.
Metal stent occlusion typically results from tumor ingrowth blocking the lumen or overgrowth causing external compression of the stent [25]. Management of expandable stent obstruction is complex; uncovered metal stents generally are not removable and maneuvers to restore patency, such as the placement of a plastic or metal stent, into the obstructed stent are relatively short lived [26, 27]. In our study, we found that the length of hospitalization for cholangitis with a metal stent tended to be longer than with a plastic stent. Although this difference did not reach the threshold for statistical significance, larger studies with more events may be able to detect a difference. Additionally, we observed a trend that the longest surviving group of patients who developed cholangitis associated with metal stents frequently developed recurrent infections (data not shown).
An alternative management strategy, used in a minority of our patients, is to employ plastic stents which are prophylactically exchanged. The subsequent use of a metal stent is based on the patient’s response to chemotherapy. In the only major study of prophylactic stent exchange in malignant biliary obstruction, Prat et al. showed that this approach achieved an equivalent period of symptom free (cholangitis free) survival compared to metal stent placement but that it requires more procedures and hospital management [10]. However, this study enrolled patients between 1993 and 1995 and the median survival was between 4.5 months (metal stent group) and 5.6 months (prophylactic exchange group), compared to the 12.7 months in our group.
Prat et al. also demonstrated that metal stents were cost effective in patients surviving more than 6 months with the mean overall cost per patients for patients whose stents were exchanged prophylactically was $6,770 compared to $4,643 for metal stents [10]. Nearly half of the patients in our study who survived greater than twelve months required inpatient management for stent related cholangitis. The patients who developed cholangitis required a median of eight days of hospitalization. At our institution the cost per day of hospitalization for cholangitis is greater than $5,000. The total cost for an ERCP with plastic stent placement at our institution is $3,400 compared to $4,600 for ERCP with metal stent placement. It is plausible that a strategy of prophylactic plastic stent exchange may be more cost effective than metal stent placement if it diminishes the frequency and duration of hospitalization for cholangitis in patients with long survival.
An additional advantage of plastic stents is that blockage, which is typically due to the formation of a bacterial biofilm within the stent, can be easily remedied by the exchange of the occluded stent with another plastic stent or metal stent [28]. In our center plastic stent exchange procedures are typically performed as same day, outpatient procedures.
In the past, metal stent placement was proposed for patients with biliary obstruction due to colorectal cancer, lymphoma, and breast cancer [29]. Over the last ten years the survival of patients with these malignancies has improved [30]. It is our practice to manage biliary obstruction in this group with serially placed plastic stents, which has also been reported in recent literature [31]. We have observed that many of these patients survive longer than three years and that bile duct narrowing can improve with chemotherapy; making the placement of permanent metal stents less advantageous. As the survival of pancreatic cancer improves, a similar rationale may emerge.
Another important alternative for potentially long surviving patients is operative biliary bypass. In their randomized trial of endoscopic stenting versus surgical bypass in distal biliary obstruction, Smith et al. report that both methods are effective palliative procedures but that surgical procedures are associated with higher initial complications, 29%, compared to 11% for endoscopic stenting but fewer long term complications (9% versus 43%) for endoscopic stent placement [8]. As the survival of patients with pancreas cancer improves the relative risks and benefits of these modalities will need to be prospectively studied. Artifon et al. report that endoscopic therapy (with metal stents) may result in a better quality of life and be less costly than surgery [9]. Nevertheless, the mean survival in their population was only 6.0 months compared to 10.4 months in comparable (metastatic) patients in our group. Additionally, they included only patients with tumor metastatic to the liver which represents only a portion of those with unresectable disease. In the current study the 26 patients with locally advanced disease had a mean survival of 15.8 months. While not statistically significant there was a trend towards a higher rate of cholangitis in these patients compared to those with metastatic disease (35% versus 29%), potentially related to their greater survival. In patients with locally advanced disease, particularly those with good functional status, operative biliary decompression should also be considered in the setting of obstruction.
An informed strategy would be to identify predictors of long survival to optimize therapy. In a multivariate analysis Prat et al. identified that tumor size less than 3 cm was the best predictor of prolonged survival. The presence of liver metastasis was not found to be a predictor though a comparison of metastatic versus locally advanced disease was not performed and remains an important topic for future work. Predictors of response to chemotherapy would also inform the endoscopic and surgical management of biliary obstruction. Promising work measuring transporter levels for gemcitabine suggests that this may eventually be done at the molecular level [32].
Limitations of this study are that it is retrospective and nonrandomized. In more than 90% of cases metal stents were used to achieve biliary decompression. Serial use of plastic stents (less than 10% of patients) tended to be used later in the period of enrollment. The practical implication of this work is that careful consideration is critical prior to the placement of a stent in patients with inoperable pancreatic adenocarcinoma receiving chemotherapy. While self expandable metal stents have a median patency of 4-9 months and provide superb drainage during this time period, this study has shown that in patients with a prolonged median survival of greater than 12 months, they are associated with a significant increase in serious biliary infections. Plastic stent placement with prophylactic exchange and eventual metal stent placement, while not a perfect alternative, is a consideration in this group. Previous strategies may have to be reconsidered as the survival of these patients improves with contemporary chemotherapy. The use of “covered” metal stents is also a possibility. Although tumor ingrowth along uncovered ends, higher migration rates, and increased risk of cholecystitis may be problematic, they may be removable [17, 18, 20, 33]. Particularly as chemotherapy improves it will be necessary to revisit operative bypass procedures as a solution for potential long survivors.
The authors wish to thank the UCSF GI Health Outcomes, Policy, and Economics (HOPE) Research Program for assistance with the statistical analysis. Scott Biggins is supported by grants from the National Center for Research Resources (KL2 RR024130), from the National Institute of Diabetes and Digestive and Kidney Diseases (DK076565) and from Agency for Healthcare Research and Quality (DK076565). This project was also supported by NIH/NCRR SC-CTSI Grant Number UL1 RR031986
None