Key words
Italy, Northern African migrants, office
visits, personal communication, women’s health
Introduction
Studies of interpreting from the field of applied
linguistics have shown that interpreters are active
participants in the interaction between the other individuals
in the conversation (Davidson, 2000, 2001,
2002; Bolden, 2000; Mason, 2001; Wadensjo¨, 1998).
Wadensjo¨ (1998) has suggested that the interpreter’s
activities can be seen as primarily oriented towards the
joint construction of meaning by interpreting both
what is said and what is implied. Interpreters therefore
need to consider the meanings and purposes that are achieved through a conversation, and thus they play a
double role, as they both interpret and coordinate
communication. For this reason, interpreting may
be understood as a form of mediation. The interpreter–
mediator is the only participant in the interaction
who is able to understand everything that the
others in the conversation say. Therefore he or she can
define the context of the encounter, draw attention to
the production of shared topics, and manage misunderstandings.
This paper focuses on this dual role as it
emerged from analysis of conversations between interpreters,
patients and doctors in an Italian healthcare
setting.
Background
Mediation
Mediation is a strategy that is used to enable individuals
who are in conflict to resolve their differences and
modify their relationship (Carnevale and Pruitt, 1992).
The intervention of a third party, namely the mediator,
does not seek to establish who is right or wrong
(Bush and Folger, 1994; Mulcahy, 2001). Rather, the
mediator intervenes as a provider of opportunities
to talk, inducing both parties to introduce and deal
with particular issues (Fisher and Shapiro, 2005; Katz
Jameson et al, 2006; Schulz, 2006) and construct
acceptable solutions (Picard and Melchin, 2007;
Winslade, 2006; Winslade and Monk, 2000). However,
doubts have been raised about the effectiveness
of mediation in promoting balanced power relationships.
Welsh and Coleman (2002, pp. 345–6) have
observed that mediators may ‘become de facto agents
of the status quo invested in maintaining the stability
of the current social system and stopping the conflict
before it moves beyond the affected institutions.’
Therefore an important question concerns the effectiveness
of mediation in challenging the status quo
and in empowering the less influential (Gwartney et al,
2002), for example, in medical systems (Bolden, 2000;
Davidson 2000, 2001).
Interpreters as mediators in
healthcare
Interpreter-mediated interaction is a triadic interaction
involving an interpreter as the third party in a
communication process between individuals who do
not share a common language. Interpreter-mediated
interactions help to create an effective form of intercultural
communication, giving voice to cultural
diversity in the interaction (Baraldi, 2006). Situations
that require interpreters are increasingly common in
western medical systems where healthcare providers encounter migrant patients (Angelelli, 2004; Baraldi
and Gavioli, 2007; Cambridge, 1999; Bu¨hrig and
Meyer, 2004; Po¨chhacker and Kadric, 1999; Tebble,
1999). The development of rapport between doctors
and patients is considered very important for the
successful outcome of treatment and care (Barry et al,
2001; Charles et al, 1999; Epstein et al, 2005; Heritage
and Maynard, 2005, 2006; Mead and Bower, 2000;
Zandbelt et al, 2005, 2006). The patient’s feelings and
wishes and the doctor’s affective involvement in the
interaction are considered of primary importance
(Barry et al, 2001) in helping the patient to comply
with treatment (Kiesler and Auerbach, 2003; Mangione-
Smith et al, 2003; Robinson and Heritage, 2005; Stivers,
2002). In this respect, healthcare providers are invited
to observe illness through the patient’s lens and to
‘treat the patient, rather than just the disease’ (Heritage
and Maynard, 2006, p. 355).
These western expectations mean that migrant
patients may encounter severe difficulties in presenting
their case histories, concerns and worries. The difficulties
involved in handling emotional expressions
in interpreter-mediated patient–doctor interactions
have been reported in several studies (Bolden, 2000;
Cambridge, 1999; Davidson, 2000; Hsieh, 2010;
Po¨chhacker and Kadric, 1999). Instead of relaying
the patient’s concerns in full to the doctor, interpreters
tend to summarise what the patient has said, focusing
on medical problems and treatments. Consequently,
emotional expressions may be overlooked or omitted.
Thus interpreters become gatekeepers, controlling what
is passed between doctor and patient, and fuelling
asymmetrical power relationships between the two
parties (Davidson, 2000, 2001; Bu¨hrig and Meyer,
2004).
Migrants in this research
Recent data (from 2011) indicate that there are 89 346
immigrants (12.7% of the resident population) in the
Modena district, and 69 060 immigrants in the Reggio
Emilia district (13% of the resident population). In
both cases, the majority of migrants originate from
Morocco and Albania. Modena also has a population
of Tunisian migrants, and Reggio Emilia has quite
large Indian and Chinese communities.
The major driver for institutional change in healthcare
systems is the requirement to provide appropriate
services for migrant women who are pregnant or who
already have children, When using healthcare services,
migrant women encounter different and unfamiliar
cultural constructions of health, disease, therapy,
sexuality and motherhood which their husbands and
fathers may not understand or approve of, and which
may therefore be a source of conflict. As a result,
healthcare providers are being encouraged to reorganise their services in innovative and creative ways based on
migrant-friendly models, which may potentially be
extended to all patients. For example, intercultural
mediators have been appointed by the General Hospital
Board and Local Health Board in Modena to help
in reception, obstetrics, nursery, paediatrics, gynaecology,
neonatology and the family advice bureau.
Reggio Emilia Local Health Board uses intercultural
mediators in the outpatients’ departments and specialised
units for the care of women and children.
Outline of the study
This paper is based on a project undertaken in Emilia
Romagna, Italy, entitled ‘Interlinguistic and intercultural
communication: analysis of interpretation
as a form of mediation for the bilingual dialogue
between foreign citizens and institutions.’ The aims
of this project were as follows:
1. to create a method of analysing healthcare practices
2. to draw up specific criteria to identify good practices
3. to develop criteria for selecting models of good
practice for evaluative analysis, pointing out the
indicators of effectiveness concerning their functionality,
correspondence to patients’ needs, and
opportunities for access
4. to develop instruments to monitor these models,
with reference to the reduction of inequalities and
barriers
5. to develop guidelines to be used in personnel
training.
Ethical considerations
The project was reviewed and approved by a Management
Coordination Committee consisting of the research
coordinator and the coordinators of the
healthcare service. The Committee was in charge of
decision making on knowledge protection, ethical and
legal issues.
Written information about the project was provided
for doctors, interpreters and patients. This
included details of the aim of the project, a request
for permission to audio-record each conversation,
and details of how the results would be used. Written
permission was requested from patients, interpreters
and doctors. The privacy of participantswas preserved
according to the Italian Data Protection Act 675 (31
December 1996).
Before each recording, the participants were
reminded about the aims of the research, what taking
part involved, and their right to withdraw. Assurances
about anonymity were important to avoid anyone being blamed or stigmatised as a result of taking part
in the research. Removing or changing names was not
always enough to ensure anonymity. In such cases the
ethical need for anonymity was prioritised over scientific
considerations about documentation. These ethical
considerations are not and cannot possibly be
exhaustive. Ethical research practice requires continuous
reflexivity and coping with ethical problems as
they arise. This requires dialogue at two levels, between
researchers as a means of collectively sharing
experience, and between researchers and participants
in the ongoing research project.
Participants
Four doctors, four nurses and four interpreters took
part in the research. All of the healthcare professionals
were of Italian origin and were native speakers of
Italian. The interpreter originated from Tunisia and
Jordan, spoke Arabic, and had been living in Italy for
at least 6 years at the time of this research. Other
interpreters who took part in the project originated
from Ghana and Nigeria and spoke English. All of
these professionals had undergone formal training to
enable them to work as intercultural mediators. Resolution
265 of the Regional Government of Emilia-
Romagna (2005) establishes training standards for
intercultural mediators. In order to be qualified as
intercultural mediators in public services, it is necessary
to follow courses organised by training centres
approved by the regional authorities. The minimum
duration of such a training course is 200 hours,
including at least 40 hours of traineeship. The interpreters
involved in this research were professional
mediators who were officially recognised by theEmilia
Romagna regional authorities. Although the research
involved patients who spoke various languages other
than Italian, this paper is based on Arabic–Italian
interactions. Thus the 55 patients who were involved
in the interactions that we discuss in this paper are
Arabic speakers, most of them fromMorocco, Tunisia
and Egypt.
As the mediation service is used predominantly in
the areas of nursery, infant care and women’s health,
most of the patients involved in the research were
women. With regard to the present paper, 51 patients
(92.72%) were women, and only 5 patients (7.28%)
were men.
Data collection and analysis
The data consisted of 55 conversations, in Arabic and
Italian, in two public healthcare services, namely
the Centro per la Salute Delle Famiglie Straniere
(Healthcare Support Centre for Foreign Families) in
Reggio Emilia, and the Consultorio (Local Centre for Health and Social Services) in Vignola (Province of
Modena). In most cases (47 cases, 85.4%) these
conversations concerned issues related to obstetrics,
nursery, paediatrics, gynaecology and neonatology.
The conversations took place in general hospital
settings, between Italian doctors who did not speak
Arabic, Arabic-speaking patients who did not speak
Italian, and interpreters, acting as intercultural mediators,
who spoke both languages and who facilitated
communication between the other two parties. Each
conversation was audio-recorded, transcribed and
analysed using two socio-linguistic methods of analysis.
The first was based on conversation analysis (CA)
and the ways in which participants in a conversation
talk according to a coordinated system of turn-taking
(Sacks et al, 1974). CA looks at the mechanisms that
invite participants in a conversation to talk, and at the
acceptance or rejection of their contributions in subsequent
interaction (Schegloff, 1980; Pomerantz, 1984).
CA suggests that responses to contributions are very
important in explaining how each participant reacts
and how they achieve an understanding of what is
going on (Mason, 2006, p. 364). What we gained from
CAwas an understanding of the system through which
the speakers achieved their understanding.
The second analytical approach was derived from
studies on intercultural communication (e.g.Gudykunst,
2005; Samovar and Porter, 1997; Ting-Toomey and
Kurogi, 1998), as we considered interpreter-mediated
interaction to be a form of intercultural communication.
We analysed the use of language and language
diversity from the perspective of intercultural communication,
observing whether the features of bilingual
or multilingual talk in the interaction reproduced
and/or tackled particular cultural aspects of the interactions.
In the following section we discuss three types of
interaction, namely those which exclude or inhibit the
patient from communicating with the doctor, those
which include the patient but not the doctor, and
three-way interactions that include the patient, the doctor and the interpreter/intercultural mediator. In
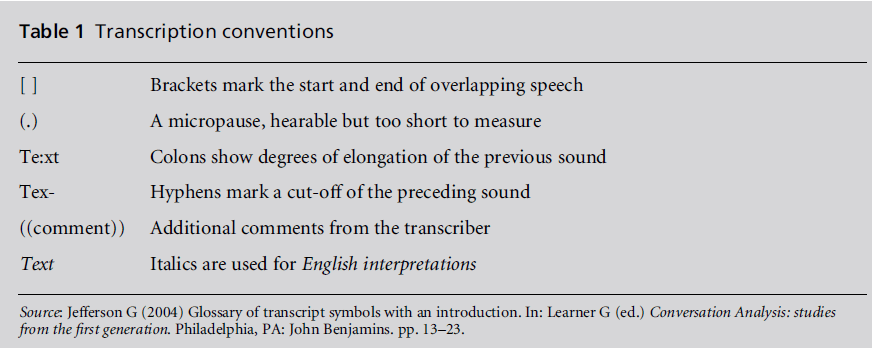
each instance we present extracts from our data using
transcription conventions set out by Jefferson (2004)
(see Table 1). In each extract the following code
applies: D = Italian healthcare provider of the institution;
IM = Arabic-speaking interpreter/intercultural
mediator; P = Arabic-speaking patient.
Interactions that exclude or
inhibit the patient
The most common types of exclusion were reduced
renditions, a term that refers to situations in which the
IM cut out some of the patient’s and doctor’s talk
(Wadensjo¨, 1998). Reduced renditions usually occurred
when the interpreter was passing information from
the patient to the doctor, and vice versa. In excerpt
CS5 (see Appendix) the patient asks two questions
(turns 3 and 5) to try to find out whether the doctor
is going to treat her leg in the office. Instead of
translating the patient’s questions, the interpreter
responds directly, hindering patient–doctor communication.
In turn 2, the interpreter produces a reduced rendition
of the doctor’s contribution in the previous turn
(‘she is giving you the ointment’), leaving out the
information about the drug not being available at
the doctor’s office. This reduced rendition indicates a
doctor-centred culture (Barry et al, 2001) in which the
patient is expected to follow instructions and the
doctor does not have to account for his or her
decisions. In this excerpt, reduced rendition creates
some concern for the patient, who is told that the
doctor is going to treat her leg with the ointment and
to buy the drug at the pharmacy in the same turn (turn
3). The interpreter uses the word ‘give’ instead of
‘prescribe’, so the patient understands ‘giving you’ as
‘treating you with the ointment.’
Table 1: Transcription conventions
Consequently, the patient is uncertain about the
doctor’s intentions. Moreover, she does not know that
the drug is not available because the interpreter did
not tell her this in turn 2, and she has no reason to
believe that the doctor will not treat her leg in the
office. In order to solve this problem, the patient
initiates a repair sequence in turn 3: ‘Is she giving it
to me?’ The repair is completed by the IM, who
responds to the patient without translating the request
to the doctor: ‘They do not have it’ (turn 4).
The doctor has not said anything to justify the new
piece of information which arrives too late in the
interaction, and the patient understands it as a way
to cover the fact that the doctor does not want to treat
her. The patient’s reiteration of the question in a
different format (turn 5) is evidence of her dissatisfaction.
The IM’s actions create distance between the
two parties, making the creation of common ground
between them very unlikely. The IM notices the
patient’s increasing dissatisfaction and tries to mitigate
it.However, she does not interpret the question to
the doctor but provides a direct response (turn 6),
thus increasing the distance between them. We can
imagine the attitude that the patient will have towards
medical prescriptions if she believes that the doctor is
not interested in her health.
Reduced renditions speed up encounters between
doctors and patients and so appear to support the
functionality of the healthcare system. However, we
may ask what kind of system functionality is supported
by these actions. Recent research (Leanza et al,
2010; Schouten et al, 2007) has confirmed the efficacy
of reduced renditions in keeping the interaction coherent
by, for example, censoring a part of the medical
discourse that might not be comprehensible to the
patient or a part of the patient’s discourse that might
not be relevant to healthcare treatment. However, the
same research shows that reduced renditions also
hinder the trust-building process between patient
and healthcare provider because they create more
distance between the principal participants. Thus
reduced renditions, interruptions and substitutions
pose a threat to the therapeutic process and, paradoxically,
compromise the core values (i.e. selfdeterminism
and informed decision making) of the
western medical system (Hsieh, 2010).
Interactions that include
patients
The IM’s actions could promote the patient’s active
involvement in the medical encounter by encouraging
their self-expression, and giving voice to their concerns,
doubts, needs and requests. This was achieved through two types of interactional practices, namely
dyadic (patient–interpreter) and triadic (patient–interpreter–
doctor).
In dyadic interactions, the IM supported the voice
of the patient through backchannelling (Schegloff,
1982; Schiffrin, 1999), using short conversational
markers such as acknowledgement tokens (e.g. ‘Sı`’,
‘Yeah’, ‘OK’), which convey that the stated information
has been received, continuers (e.g. ‘hmmm’,
‘mmh’), which maintain the flow of conversation and
the desire of the current speaker to continue his or her
turn, and echoing, which serves as a floor-yielding
device that provides feedback to demonstrate that
attention has been paid to what is being said. These
conversational markers provide space for the speakerin-
turn to go on, adding or completing their contribution
with the help of the IM. Thus the IM and the
speaker are both involved in the interpreting process.
In excerpt CO1 (see Appendix), the IM expresses
her attentiveness and understanding through feedback
tokens (‘Ah’, ‘mmh’, ‘Ah, I understand you’). In
turn 122, the IM encourages the patient to express her
concerns, making her participation relevant as a
person with specific needs and worries rather than a
generic sick person who is expected to provide a list of
current symptoms. In this excerpt, the IM systematically
encourages the patient to express her doubts
about the therapy, thus promoting her participation
in the conversation. Being empowered as an active
participant, the patient is confident enough to finally
advance a request for clarification (turn 123).
In triadic interactions, all three participants (patient,
doctor and IM) are involved in the conversation. The
IM’s actions bring the doctor into the conversation
through the use of formulations of the patient’s contributions.
Formulations are summaries or the gist of
what someone has said (Heritage, 1985). They provide
directions for subsequent turns by inviting responses
in so far as they ‘advance the prior report by finding a
point in the prior utterance and thus shifting its focus,
redeveloping its gist, making something explicit that
was previously implicit in the prior utterance, or by
making inferences about its presuppositions or implications’
(Heritage, 1985, p. 104). In our study, the
IM’s formulations consisted of interpretations which
followed patient–IM dyadic sequences, but with adaptations
to accommodate the doctor. Formulations
enabled IMs to build, expand and recreate the meanings
of previous dyadic sequences according to presuppositions
and orientations for which they were
responsible. Formulations are not word-for-word
interpretations of contributions in previous dyadic
sequences, but rather they rely on the IM’s discursive
initiative and willingness to create common ground
between the patient and the doctor. Thus the IM acts
as both interpreter and mediator.
Specifically, formulations are conversational resources
available to the IM in order firstly to provide
an interpretation that highlights content from previous
sequences, secondly, to make explicit what was
thought in previous turns of talk to be implicit or
unclear, and thirdly, to propose inferences about
presuppositions or implications of the participants’
contributions (Baraldi and Gavioli, 2008). Formulations
are informational when they elicit an explanation
from the doctor which the patient is somehow
inhibited from requesting, and affective when they
bring the patient’s emotions, doubts and concerns
into the conversation.
Excerpt CO23 (see Appendix) is an example of an
informational formulation. In the course of the examination
of a pregnant woman, it becomes apparent
that the fetus is not yet in the appropriate position. In
turn 59 the doctor reassures the patient about this
issue, and in turn 60 the IM offers reassurance and
further suggestions to the patient. The doctor is then
re-involved in the interaction in turn 63, through an
informational formulation which is introduced by the
IM to obtain therapeutic recommendations for the
patient’s benefit. In CO23, the informational formulation
is an initiative motivated by the IM’s interpretation
of the patient’s situation.
Affective formulations may be understood as discursive
initiatives undertaken by the IM to give voice to
the patient’s emotions, which in most cases manifest
themselves implicitly. Patients rarely talk about their
emotions directly and without prompting. Instead
they provide clues about their feelings, thus providing
health professionals and IMs with ‘potential emphatic
opportunities’ (Beach and Dixson, 2001, p. 39). Affective
formulations focus on the emotional point of
the patient’s utterances, giving the doctor the chance
to share and become involved in the affective dimension
of the interaction. In this way the doctor is made
aware of the patient’s concerns, and the patient
assumes an identity that goes beyond the generic social
role of being sick.
In excerpt CO11 (see Appendix), the patient reports
a delay in her menstrual period, but mitigates the
relevance of this information by assuming that her
period will start within the next few days. Through
affective formulations, the IM brings the patient’s
emotions, which have remained implicit up to that
moment, to the fore, making them a topic for communication
and concern. The IM’s formulation, ‘She’s a
bit worried’ (in turn 65), is affective because, while
making current symptoms available to the doctor, it
highlights the patient’s emotional situation which
could otherwise have gone unnoticed in previous
turns. The IM’s formulation of affective understanding
involves the doctor in the affective exchange,
and promotes a shift from a dyadic to a triadic
interaction.
The IM’s affective formulation offers the doctor the
opportunity to tune into the emotional status of the
patient, and to reassure her as necessary. Affective
formulations are inclusive because, while highlighting
the emotions of the patient, they also involve the
doctor in the formation of affective relations. By
producing an affective formulation, the IM develops
and emphasises an implicit emotional expression as a
basis for subsequent interaction. Affective formulation
reveals the IM not as a neutral conduit, but
rather as an active mediator of the preceding talk. In
particular, the IM’s active participation concerns the
patient’s implicit, difficult and embarrassed emotional
expressions, providing a way to include such expressions
in the triadic sequence, and for it to be
treated in a patient-centred interaction involving the
doctor (Baraldi and Gavioli, 2007).
Conclusion
The dual function of interpreter and mediator can
make positive contributions to patient-centred care
and treatment. This paper has focused on how these
two functions are intertwined and how they affect
doctor–patient communication. When the interpreter
acts effectively as a mediator, otherwise hidden factors,
such as the patient’s emotional expressions, can
be relayed to the doctor, thus creating opportunities
for him or her to respond. If the interpreter does not
act in this way, the patient’s feelings may be neglected.
Analysis of emergency visits in two large paediatric
departments in the USA (Flores et al, 2012) suggests an
association between the number of previous hours
of interpreter training and error numbers, types and
potential consequences in English–Spanish mediated
interactions. Well-trained professional interpreters
demonstrated a significantly lower likelihood of errors
than ad-hoc interpreters such as family members or
other hospital staff. The study suggests that training
for interpreters might have a major impact on reducing
interpreter errors and their consequences in healthcare,
while improving quality of care and patient safety.
Although we agree with the importance of professional
training for interpreters, we also argue that the
complexity of the mediator’s task needs to be acknowledged.
According to the literature on dialogue interpreting
(Angelelli, 2004; Baker, 2006; Bolden, 2000;
Davidson, 2000, 2001; Mason, 1999, 2006; Wadensjo¨,
1998), in triadic interactions the interpreters are the
only participants who can effectively understand all of
the content and the intentions of the other participants.
This implies that interpreters are never neutral
conduits, and that errors are not the only issue.
Interpreter–mediators necessarily coordinate the contingent
and changeable construction of a difference between cultural presuppositions and the corresponding
distribution of communicative resources, through
their translation activity in intercultural contexts.
Our data suggest that the dual roles of interpreter–
mediators are crucial in enabling patients to make
their voices and their wishes heard during medical
encounters. We have observed how reduced renditions
may exclude the patient or the doctor from the
conversation and from relevant healthcare information.
On the other hand, we have seen how the use of
formulations improves the emotional rapport between
patient and doctor, taking the medical encounter well
beyond a mere exchange based on standardised roles.
In our analysis of patient–doctor conversations, interpreter-
mediators contribute to dialogue management
in at least two ways, first, as responders, affiliating
with the patient in dyadic interactions, and secondly,
as coordinators, affiliating with the patient and then
involving the doctor. As responders, interpretermediators
have an opportunity to check and echo
the patient’s perceptions and emotions, actively listen
to and appreciate their expressions, provide positive
feedback, and express personal concern for them. In a
more complex interaction, this can form the basis of
an important step in patient care.
CONFLICTS OF INTEREST
None.
References
- Angelelli CV (2004) Medical Interpreting and Cross-cultural Communication. Cambridge: Cambridge University Press.
- Baker M (2006) Contextualization in translator- and interpreter- mediated events. Journal of Pragmatics 38:321ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â37.
- Baraldi C (2006) Diversity and adaptation in intercultural mediation. In: Busch D (ed.) Interkulturelle Mediation. EinetheoretischeGrundlegungtriadischerKonfliktbearbeitung in interkulturellbedingtenKontexten. Frankfurt: Peter Lang.
- Baraldi C and Gavioli L (2007) Dialogue interpreting as intercultural mediation. An analysis in healthcare multicultural settings. In: Grein M and Weigand E (eds) Dialogue and Culture. Amsterdam: John Benjamins. pp. 155ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â75.
- BaraldiCandGavioli L (2008) Cultural presuppositions and re-contextualisation of medical systems in interpretermediated interactions. Curare 31:193ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â204.
- Barry CA, Stevenson FA, Britten N et al (2001) Giving voice to the lifeworld. More human, more effective medical care? A qualitative study of doctorÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âpatient communication in general practice. Social Science and Medicine 53:487ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â505.
- Beach WA and Dixson CN (2001) Revealing moments: formulating understandings of adverse experiences in a health appraisal interview. Social Science and Medicine 52:25ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â44.
- Bolden GB (2000) Toward understanding practices of medical interpreting: interpretersÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ involvement in history taking. Discourse Studies 4:387ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â419.
- BuÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâèhrig K and Meyer B (2004) Ad hoc-interpreting and the achievement of communicative purposes in doctorÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âpatient communication. In: House J and Rehbein J (eds) Multilingual Communication. Amsterdam: John Benjamins. pp. 43ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â62.
- Bush BRA and Folger JP (1994) The Promise of Mediation: responding to conflict through empowerment and recognition. San Francisco, CA: Jossey-Bass Publishers.
- Cambridge J (1999) Information loss in bilingual medical interviews through an untrained interpreter. The Translator 5:201ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â20.
- Carnevale PJ and Pruitt DG (1992) Negotiation and mediation. Annual Review of Psychology 43:531ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â82.
- Charles C, Gafni A and Whelan T (1999) Decision-making in the doctorÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âpatient encounter: revisiting the shared treatment decision-making model. Social Science and Medicine 49:651ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â61.
- Davidson B (2000) The interpreter as institutional gatekeeper: the socialÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âlinguistic role of interpreters in SpanishÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â English medical discourse. Journal of Sociolinguistics 4:379ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â405.
- Davidson B (2001) Questions in cross-linguistic medical encounters: the role of the hospital interpreter. Anthropological Quarterly 74:170ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â78.
- Davidson B (2002) A model for the construction of conversational common ground in interpreted discourse. Journal of Pragmatics 34:1273ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â300.
- Epstein RM, Franks P, Fiscella K et al (2005) Measuring patient-centered communication in patientÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âdoctor consultations: theoretical and practical issues. Social Science and Medicine 61:1516ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â28.
- Fisher R and Shapiro D (2005) Beyond Reason: using emotions as you negotiate. New York: Viking.
- Flores, G, Abreu M, PizzoBarone C et al (2012) Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Annals of Emergency Medicine DOI: 10.1016/j.annemergmed.2012.01.025.
- Gudykunst WB (ed.) (2005) Theorizing About Intercultural Communication. Thousand Oaks, CA: Sage.
- Gwartney P, Fessenden L and Landt G (2002) Measuring the long-term impact of a community conflict resolution process. Negotiation Journal 18:51ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â74.
- Heritage J (1985) Analysing news interviews: aspects of the production of talk for an overhearing audience. In: Van Dijk T (ed.) Handbook of Discourse Analysis. Volume 3. Discourse and dialogue. London: Academic Press. pp. 95ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 117.
- Heritage J and MaynardDW(eds) (2005) Communication in Medical Care: interactions between primary care physicians and patients. Cambridge: Cambridge University Press.
- Heritage J and MaynardDW(2006) Problems and prospects in the study of physicianÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âpatient interaction: 30 years of research. Annual Review of Sociology 32:351ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â74.
- Hsieh E (2010) ProviderÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âinterpreter collaboration in bilingual health care: competitions of control over interpreter- mediated interactions. Patient Education and Counselling 78:154ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Jefferson G (2004) Glossary of transcript symbols with an introduction. In: Lerner G (ed.) Conversation Analysis: studies from the first generation. Philadelphia, PA: John Benjamins. pp. 13ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â23.
- Katz Jameson J, BotkerAMand Jones TS (2006) Like talking to a brick wall: implications of mediation metaphors for mediation practice. Negotiation Journal 22:199ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â207.
- Kiesler DJ and Auerbach SM (2003) Integrating measurement of control and affiliation in studies of physicianÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â patient interaction: the interpersonal circumplex. Social Science and Medicine 57:1707ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â22.
- Leanza Y, Boivin I and Rosenberg E (2010) Interruptions and resistance: a comparison of medical consultations with family and trained interpreters. Social Science and Medicine 70:1888ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â95.
- Mangione-Smith R, Stivers T, Elliot M et al (2003) Online commentaries during the physical examination: a communication tool for avoiding inappropriate antibiotic prescribing? Social Science and Medicine 56:313ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â20.
- Mason I (ed.) (1999) Dialogue interpreting. The Translator Special Issue 5(2). Mason I (2001) Triadic Exchanges: studies in dialogue interpreting. Manchester: St Jerome.
- Mason I (2006) On mutual accessibility of contextual assumptions in dialogue interpreting. Journal of Pragmatics 38:359ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â73
- Mead N and Bower P (2000) Patient centredness: a conceptual framework and review of the empirical literature. Social Science and Medicine 51:1087ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â110.
- Mulcahy L (2001) The possibilities and desirability of mediator neutrality ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â towards an ethic of partiality? Social and Legal Studies 10:505ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â27.
- Picard CA and Melchin KR (2007) Insight mediation: a learning-centered mediation model. Negotiation Journal 23:35ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
- PoÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâèchhacker F and Kadric M (1999) The hospital cleaner as healthcare interpreter: a case study. The Translator 5:161ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 78.
- Pomerantz A (1984) Pursuing a response. In: Heritage J and Atkinson JM (eds) Structures of Social Action. Cambridge: Cambridge University Press. pp. 152ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â63.
- Robinson JD and Heritage J (2005) The structure of patientsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ presenting concerns: the completion relevance of current symptoms. Social Science and Medicine 61:481ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â93.
- Sacks H, Schegloff EA and Jefferson G (1974) A simplest systematics for the organization of turn-taking for conversation. Language 50:696ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â735.
- Samovar LA and Porter RE (eds) (1997) Intercultural Communication: a reader. Belmont, CA: Wadsworth.
- Schegloff EA (1980) Preliminaries to preliminaries: ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âCan I ask you a question?ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ Sociological Inquiry 50:104ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â52.
- Schegloff EA (1982) Discourse as an interactional achievement: some uses of ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âuh huhÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ and other things that come between sentences. In: Tannen D (ed.) Analyzing Discourse: text and talk (Georgetown University Roundtable on Languages and Linguistics 1981).
- Washington, DC: Georgetown University Press. pp. 71ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â93.
- Schiffrin D (1999) ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ãâ¹Ã
âOhÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ as a marker of information management. In: Jaworski A and Coupland N (eds) The Discourse Reader. London: Routledge. pp. 275ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â88.
- Schouten BC, Meeuwesen L, Tromp F et al (2007) Cultural diversity in patient participation: the influence of patientsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ characteristics and doctorsÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ communicative behaviour. Patient Education and Counselling 67:214ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â23.
- Schulz JL (2006) Confectionery and conflict resolution? What chocolate reveals about mediation. Negotiation Journal 22:251ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â77.
- Stivers T (2002) Participating in decisions about treatment: overt patient pressure for antibiotic medication in pediatric encounters. Social Science and Medicine 54:1111ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â30.
- Tebble H (1999) The tenor of consultant physicians: implications for medical interpreting.
- The Translator 5:179ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 200. Ting-Toomey S and Kurogi A (1998) Facework competence in intercultural conflict: an updated face-negotiation theory. International Journal of Intercultural Relations 22:187ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â225.
- WadensjoÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâè C (1998) Interpreting as Interaction. London: Longman. WelshNAand Coleman PT (2002) Institutionalized conflict resolution: have we come to expect too little? Negotiation Journal 18:345ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â50.
- Winslade J (2006) Mediation with a focus on discursive positioning. Conflict Resolution Quarterly 23:501ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â15.
- Winslade J and Monk G (2000) Narrative Mediation: a new approach to conflict resolution. San Francisco, CA: Jossey- Bass.
- Zandbelt LC, Smets EMA and Oort FJ (2005) Coding patient-centred behaviour in the medical encounter. Social Science and Medicine 61:661ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â71.
- Zandbelt LC, Smets EMA, Oort FJ et al (2006) Determinants of physiciansÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ patient-centred behaviour in the medical specialist encounter. Social Science and Medicine 63:899ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â 910.
Appendix